Anne Garland RMN, MSc.
School of Health Sciences
The University of Nottingham
The role of shame, self-criticism and self-compassion
In persistent, treatment resistant depression
Chapter one: Introduction and overview
Depression and co-morbid disorders
Motivation for conducting this study
The cognitive science of depression
The evidence base for Cognitive Behaviour Therapy (CBT)
TABLE 1: DSM-5 DIAGNOSTIC CRITERIA FOR MAJOR DEPRESSIVE DISORDER (APA 2013 P 160–161)
TABLE 2: DSM-5 DIAGNOSTIC CRITERIA FOR PERSISTENT DEPRESSIVE DISORDER (APA 2013 P 168–169)
Defining and treating persistent, treatment resistant depression
The way forward in persistent, treatment resistant depression
The Practicality of theories: Defining a decision-making process
The conundrum of defining Shame as an affect
Cognitive-affective models of shame
Cognitive-Attributional theories of shame
Lewis’ attributional theory of self-conscious emotions
Standards, Rules and Goals (SRG’s)
Internal versus external evaluations
Attributions about self: Global versus Specific
Step 1: Survival-Goal Relevance
Step 2: Attentional Focus on Self and Activation of Self-Representations
Step 3: Identity-Goal Relevance
Step 4: Identity-goal congruence
Step 5: Internality attributions
Step 6: Stability, Globality, controllability attributions
The evolutionary and biopsychosoical psychology model of shame
The definition of self-criticism
The psychoanalytic Formulation of Self-criticism
The Behavioural Formulation of Self-criticism
The cognitive formulation of self-criticism
The evolutionary formulation of self-criticism
Theories of the nature and origins of self-criticism and self-blame
Defining compassion and self-compassion
An evolutionary formulation of compassion
Compassion as an appraisal elicited emotion
Compassion as a motivational system
Self-kindness versus self-judgment
Common humanity versus isolation
Mindfulness versus over identification or avoidance
Examining the Practicality of these theories of shame using Brawley’s criteria
A critique of Gilbert’s theory of shame
Philosophical Pragmatism as an epistemological foundation
Convergent Parallel Mixed Methods
The power calculation in this PhD study
Inclusion and exclusion criteria for the RCT
Step 1: Testing the psychometric status of OAS; FSCR and SCS
Rationale for chosen measures of shame, self-criticism and self-compassion
The forms of self-criticising/attacking and self-reassuring scale (FSCRS)
Step 2: Modelling variance in depressive symptoms against shame, self-criticism and selfcompassion
Rationale for chosen measures of depression
Hamilton Depression Rating Scale-17 (HDRS-17)
Beck Depression Inventory-I (BDI-I)
The Patient Health Questionnaire (PHQ-9)
Description of Qualitative Data Collection Method
TABLE 5: TYPES OF QUESTIONS FOR IN-DEPTH INTERVIEWS
Establishing reliability and validity of the OAS, FSCR and SCS
Modelling variance of depression in relation to shame, self-criticism and self-compassion
An overview of Interpretative Phenomenological Analysis
The argument for epistemological coherence: The Primacy of Praxis revisited
Process for obtaining informed consent
Fieldwork and safety guidelines
Ethics Approval to conduct this research
Chapter 4 Quantitative Results
I. Univariate and multivariate regression analysis
The demographic profile of the study cohort
TABLE 6: DEMOGRAPHIC CHARACTERISTICS OF THE STUDY COHORT AT BASELINE
Descriptive Statistics for Other as Shamer Scale (OAS) baseline
TABLE 10: SUMMARY STATISTICS FOR OAS AT BASELINE
TABLE 11: DISTRIBUTION FOR EACH SUB-SCALE OF OAS AT BASELINE
TABLE 12: CRONBACH’S ALPHA SCORES AT BASELINE FOR OAS SCALE
TABLE 13: ITEM STATISTICS FOR SUB-SCALE INFERIOR AT BASELINE
TABLE 14: ITEM STATISTICS FOR SUB-SCALE INFERIOR AT BASELINE
TABLE 15: ITEM STATISTICS FOR SUB-SCALE EMPTINESS AT BASELINE
TABLE 16: ITEM TO ITEM CORRELATION FOR SUB-SCALE EMPTINESS AT BASELINE
TABLE 17: ITEM STATISTICS FOR SUB-SCALE MISTAKES AT BASELINE
TABLE 18: ITEM TO ITEM CORRELATION FOR SUB-SCALE MISTAKES AT BASELINE
Split-Half Reliability for OAS at baseline
TABLE 19: SUMMARY ITEM MEANS STATISTICS FOR OAS AT BASELINE
Test-retest reliability for OAS at baseline and 6 months
TABLE 21: TEST-RETEST RELIABILITY FOR OAS AT BASELINE AND 6 MONTHS
Confirmatory Factor Analysis (CFA)
TABLE 22: THE CONTINUOUS LATENT VARIABLES AND INDICATORS TESTED FOR OAS, FSCSR AND SCS
Confirmatory Factor Analysis for Other as Shamer Scale
FIGURE 6: CONFIRMATORY FACTOR ANALYSIS PATH DIAGRAM FOR THE OTHER AS SHAMER SCALE (OAS)
Descriptive Statistics for Forms of Self-Criticising Self -Reassuring Scale (FSCRS)
TABLE 24: SUMMARY STATISTICS FOR FSCSR AT BASELINE
TABLE 25: DISTRIBUTION FOR EACH SUB-SCALE OF FSCSR AT BASELINE
TABLE 26: CRONBACH’S ALPHA FOR FSCSR AT BASELINE
TABLE 27: ITEM STATISTICS FOR SUB-SCALE INADEQUATE SELF AT BASELINE
TABLE 28: ITEM TO ITEM CORRELATION FOR SUB-SCALE INADEQUATE SELF AT BASELINE
TABLE 29: ITEM STATISTICS FOR SUB-SCALE HATED SELF AT BASELINE
TABLE 30: ITEM TO ITEM CORRELATION FOR SUB-SCALE HATED SELF AT BASELINE
TABLE 31: ITEM STATISTICS FOR SUB-SCALE REASSURED SELF AT BASELINE
TABLE 33: SUMMARY ITEM MEANS STATISTICS FOR FSCSR AT BASELINE
TABLE 34: SPLIT HALF RELIABILITY SCALE STATISTICS FOR FSCSR AT BASELINE
Test-retest reliability for FSCSR at baseline and 6 months
TABLE 35: TEST -RETEST RELIABILITY FOR FSCSR BETWEEN BASELINE AND 6 MONTHS
Confirmatory Factor Analysis for the Forms of Self-Criticism and self-Reassurance Scale (FSCSR)
TABLE 36: MODEL FIT INDICES FOR FSCSR
Descriptive Statistics for Self-Compassion Scale (SCS) baseline
TABLE 37: SUMMARY STATISTICS FOR SELF-COMPASSION SCALE (SCS) AT BASELINE
TABLE 38: DISTRIBUTION FOR EACH SUB-SCALE OF SCS AT BASELINE
TABLE 39: CRONBACH’S ALPHA FOR SCS AT BASELINE
TABLE 40: ITEM STATISTICS FOR SUB-SCALE SELF-KINDNESS AT BASELINE
TABLE 41: ITEM TO ITEM CORRELATION FOR SUB-SCALE SELF-KINDNESS AT BASELINE
TABLE 42: ITEM STATISTICS FOR SUB-SCALE SELF-JUDGMENT AT BASELINE
TABLE 43: ITEM TO ITEM CORRELATIONS FOR SUB-SCALE SELF-JUDGEMENT AT BASELINE
TABLE 44: ITEM STATISTICS FOR SUB-SCALE COMMON HUMANITY AT BASELINE
TABLE 45: ITEM TO ITEM CORRELATIONS FOR SUB-SCALE COMMON HUMANITY AT BASELINE
TABLE 46: ITEM STATISTICS FOR SUB-SCALE ISOLATION AT BASELINE
TABLE 47: ITEM TO ITEM CORRELATIONS FOR SUB-SCALE ISOLATION AT BASELINE
TABLE 48: ITEM STATISTICS FOR SUB-SCALE MINDFULNESS AT BASELINE
TABLE 49: ITEM TO ITEM CORRELATIONS FOR SUB-SCALE MINDFULNESS AT BASELINE
TABLE 50: ITEM STATISTICS FOR SUB-SCALE OVERIDENTIFICATION AT BASELINE
TABLE 51: ITEM TO ITEM CORRELATIONS FOR SUB-SCALE OVERIDENTIFICATION AT BASELINE
TABLE 52: SUMMARY ITEM MEANS FOR SCS AT BASELINE
TABLE 53: SPLIT HALF RELIABILITY SCALE STATISTICS FOR SCS AT BASELINE
Test-retest reliability for SCS at baseline
Confirmatory Factor Analysis (CFA) for SCS
TABLE 55: MODEL FIT INDICES FOR SCS
TABLE 57: INFLUENCE OF OAS, FSCSR AND SCS ON BDI-I UNIVARIATE AND MULTIVARIATE REGRESSION MODELLING
TABLE 58: INFLUENCE OF OAS, FSCSR AND SCS ON PHQ-9 UNIVARIATE AND MULTIVARIATE REGRESSION MODELLING
TABLE 59: DEFINITION OF ‘COGNITION’ WITHIN IPA
Emergent themes and sub-themes in the qualitative data
1. Childhood adversity and social milieu
3. The function of self-criticism 4. Absence of self-compassion
1. Childhood adversity and the social milieu
Reluctance to speak about childhood
I. Not good enough/inferior/failure-self-criticism
ii. unimportant/not counting/not worthy-self-blame
iii. Bad/inadequate/insignificant/worthless: self-hate/loathing
3. The function of self-criticism/self-hating
i. Intellectual appreciation with good intentions
ii. Not understood/incomprehension
7. Memory and information processing biases in depression
Examination of the psychometric properties of the OAS, FSCSR and SCS in the study cohort
Suggested revisions to the OAS
Previous studies of the psychometric properties of the OAS
Examination of the FSCSR and its sub-scales in relation to persistent treatment resistant depression
Previous studies of the psychometric properties of the FSCSR
Examination of the SCS by sub-scale in relation to persistent treatment resistant depression
Previous studies of the psychometric properties of the SCS
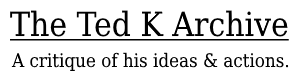
evolutionary biopsychosocial model
Defining the parameters of approval and subjugation
Shame of not meeting expectation: Every expectation
Shame, ridicule and humiliation: No expectation
Riven with shame: trapped and defeated
Clinical implications of these findings and avenues for future research
Frost, J. (2019). Regression Analysis: An Intuitive Guide for Using and Interpreting Linear
Health Research Authority (HRA) (2015) East Midlands-Nottingham Research Ethics
Appendix III: Proposed criteria for Multiple-Therapy-Resistant (MTR) Major Depressive Disorder
Appendix VI: Theories of shame measured against Brawley’s (1993) Practicality of a theory criteria
Appendix VII: Consort diagram of participant flow through RCT
Appendix VIII: Email invitation to participate as a healthy control in the study
Appendix IX: Healthy Controls: Screening Questionnaire Introduction and Background Information
Invitation to take part in the study
Involvement of the General Practitioner/Family doctor (GP)
Appendix XII: Other as Shamer Scale
Appendix: XIII: The Forms of Self-Criticising and Self-Reassuring Scale (FSCRS)
Appendix XIV: Self Compassion Scale (SCS)
Appendix XV: Hamilton Depression Rating Scale-17</strong> (Hamilton, 1960)
Appendix XVI: Beck Depression Inventory-I (BDI-I)
Appendix XVII: The Patient Health Questionaire-9 (PHQ-9)
Appendix XVIII: Qualitative Interview Topic Guide
Background information and rapport building
Appendix XIX: Histogram and box plot for the OAS sub- inferior at baseline
Appendix XX: Histogram and box plot for the OAS sub-scale emptiness at baseline
Appendix XXI: Histogram and box plot for the OAS sub- mistakes at baseline
Appendix XXII: Histogram and box plot for the FSCSR sub-scale inadequate self at baseline
Appendix XXIII: Histogram and box plot for the FSCSR sub- hated self at baseline
Appendix XXIV: Histogram and box plot for the FSCSR sub-scale reassured self at baseline
Appendix XXV: Histogram and box plot for the SCS sub-scale self-kindness at baseline
Appendix XXVI: Histogram and box plot for the SCS sub-scale self-judgement at baseline
Appendix XXVII: Histogram and box plot for the SCS sub-scale common humanity at baseline
Appendix XXVIII: Histogram and box plot for the SCS sub-scale isolation at baseline
Appendix XXIX: Histogram and box plot for the SCS sub-scale mindfulness at baseline
Appendix XXX: Histogram and box plot for the SCS sub-scale overidentification at baseline
Appendix XXXI: Example of steps of qualitative data analysis (participant 12)
Appendix XXXII: Photographs of an example of a mind map (participant 12)
Appendix XXXIII: Biographies of participants in qualitative arm of this PhD study
Appendix XXXIV: The subscales and items of the OAS
Appendix XXXV: The sub-scales and items of the FSCSR
Abstract
Background
In 2017 the World Health Organisation (WHO), declared depression to be the leading cause of disability adjusted life years lost due to ill-health. Further, it is well established in the research literature that depression is a relapsing illness. In using Cognitive -Behavioural Therapy (CBT) with patients diagnosed with persistent, treatment resistant depression two clinical observations underpin this thesis. Firstly, that shame and self-criticism are key features of depression and secondly that standard Beckian CBT interventions have limited impact in tackling shame and self-criticism in this patient group. Integrating Compassion Focused Therapy (CFT) with CBT interventions results in some amelioration of shame and selfcriticism, but this is limited empirically.
Aim
To examine shame, self-criticism and self-compassion in persistent, treatment resistant depression using the framework of Gilbert’s evolutionary psycho-biosocial formulation of emotional disorders.
Methods
Using a convergent parallel mixed methods design, the present study investigated the psychometric properties of three measures: the Other as Shamer Scale (OAS), Forms of SelfCriticism and Self-Reassurance Scale (FSCSR) and the Self Compassion Scale (SCS) in a sample recruited from a large National Institute for Health Research (NIHR) funded Randomised Controlled Trial (RCT). Internal consistency and test-retest reliability were assessed, and construct validity examined with Confirmatory Factor Analysis (CFA). Univariate and multivariate statistical analysis was conducted to test the degree to which levels of shame, self-criticism and self-compassion varied according to level of depression as measured on three well validated measures of depression. In addition, using semi-structured interviews, a subset of participants (n=10) from the Treatment as Usual Arm (TAU) of the RCT cohort were interviewed to explore their lived experience of depression, shame, self-criticism and selfcompassion. Interview data was analysed using Interpretative Phenomenological Analysis (IPA).
Findings
The OAS and FSCSR were found to be both reliable and valid measures when administered to this cohort. The descriptive goodness of fit indices and CFA supported the three-factor model (inferior, emptiness, mistakes) of external shame in the OAS and the three-factor (inadequate self, hated self, reassured self) model of internal shame in the FSCSR. The qualitative data provided evidence to support this conclusion. However, in the OAS the sub-scale emptiness did not perform as well as the inferior and mistakes sub-scales. This was also reflected in the qualitative data with no respondent speaking about emptiness as formulated within the OAS, but rather speaking about worthlessness as an aspect of external shame. Meanwhile, whilst the SCS demonstrated reliability it did not prove to be a valid measure in the cohort under study. The descriptive goodness of fit indices supported the six-factor model proposed by the SCS but the measure showed poor discriminant validity, due to issues of multicollinearity. In addition, the qualitative data analysis suggested the negative sub-scales of the SCS (selfjudgement, isolation and overidentification) appeared to tap directly into the psychopathology of depression. An unexpected finding in the quantitative data analysis was that levels of shame and self-criticism did not appear to be a function of severity of depression but appear to be more stable psychological constructs. However, the qualitative data contradicted this. Both forms of data collected in this thesis highlight the importance of attribution in depression and shame. The qualitative analysis yielded interesting data regarding the relationship between different childhood environments and the different forms of external and internal shame.
Conclusion
The OAS (a measure of external shame) and the FSCSR (a measure of internal shame) are reliable and valid measures when tested on a cohort with persistent, treatment resistant depression. Further, both the quantitative and qualitative results provided evidence to support the formulation of shame tested in this thesis, and the presence of an interrelated, but differentiated relationship between external and internal shame in this population. A model is proposed which integrates attributional theories of depression and shame, and an evolutionary psychobiosocial perspective, which takes into consideration the cognitive science of depression, specifically, the presence of intrusive, autobiographical, shame based emotional memories in depression and the role of rumination, thought suppression and dissociation, as affect regulation strategies. These memories, linked to childhood trauma, are important in the maintenance of persistent, treatment resistant depression. This study extends clinical knowledge of the phenomenology of shame, self-criticism and selfcompassion in the population studied.
Associated outputs
Publications
Guo, B., Kaylor-Hughes, C., Garland, A., Nixon, N., Sweeney, T., Simpson, S., Dalgleish, T., Ramana, R., Yang, M. and Morriss, R. (2017) Factor structure and longitudinal measurement invariance of PHQ-9 for specialist mental health care patients with persistent, major depressive disorder: Exploratory Structural Equation Modelling. Journal of Affective Disorders 219: pp. 1–8. Available at: https://doi.org/10.1016/j.jad.2017.05.020 (Accessed 23rd July 2020).
Morriss, R., Garland, A., Nixon, N., Boliang Guo., James, M., Kaylor-Hughes., C., Moore, R., Ramana, A., Sampson, C., Sweeney, T. and Dalgleish, T. (2016) Efficacy and cost effectiveness of a specialist depression service versus specialist mental healthcare to manage persistent depression: a randomised controlled trial. The Lancet Psychiatry 3 (9): pp. 821–831.
Morriss, R., Martunnen, S., Garland, A., Nixon, N., McDonald, R., Sweeney, T., Flambert, H., Fox, R., Kaylor-Hughes, C., James, M. and Yang, M., (2010) Randomised controlled trial of the clinical and cost effectiveness of a specialist team for managing refractory unipolar depressive disorder. BMC Psychiatry 10:100. Available at: doi:10.1186/1471-244X-10-100 (Accessed 16th June 2012).
Thomson, L., Barker, M., Kaylor-Hughes, C., Garland, A., Ramana, R., Morriss, R., Hammond, E., Hopkins, G. and Simpson, S. (2018) How is a specialist depression service effective for persistent moderate to severe depressive disorder?: a qualitative study of service user experience. BMC Psychiatry 18 (194): pp. 1–12. Available at: https://doi.org/10.1186/s12888-018-1708-9 (Accessed 23rd July 2020).
Presentations
A defence of pragmatism as an epistemological position in healthcare research 20th April 2013. 1-hour presentation at: Research Saturday Seminars part of School of Health Sciences PhD study programme.
Symposium conveener and speaker: British Association of Behavioural and Cognitive Psychotherapies (BABCP) 43rd Annual Conference, Warwick, 2015: ‘It’s Not Just What We Do It’s the Way That We Do It’: Improving clinical outcomes in CBT for complex chronic and recurrent depression through innovation in therapy and service delivery model.
Organiser and speaker at: CLAHRC NDL Mood Disorder Conference 2012/2013/2014. University of Nottingham and Nottinghamshire Healthcare NHS Trust.
Associated training
Completed Modules (Masters level) University of Nottingham SOCI4074: Philosophy of Research (10 credits level 4).
M14152: Foundations in Qualitative Methods 2011/12 (10 credits level 4).
EPID4022: Data organisation and management in epidemiology (DOME): A practical course in Stata. (10 credits level 4).
SOCI208: Research Design and Practice (10 credits level 4).
B74MMR: Mixed methods in Health Research 2012 (10 credits level 4).
Short Courses
Searching Healthcare Databases 16th November 2011.
Introduction to Good Clinical Practice -National Institute for Health Research (NIHR) Clinical Research Network 14th December 2011.
Introduction to Multilevel Statistical Modelling- Dr. Boliang Guo, Institute of Mental Health, June 2015.
Acknowledgements
First and foremost, I would like to thank the participants in the RCT in which this PhD study was based, alongside the patients diagnosed with persistent, treatment resistant depression, with whom I have had the privilege to share the psychotherapy endeavour over the last three decades. You have shown immense fortitude on this journey and through your determination to persevere have demonstrated that as humans we are wired to survive and thrive, sometimes against the odds. I am honoured to have learned all that I have from you-in no small way you have helped make me the clinician, researcher and educator I am today and to quote Joni Mitchell: ‘Part of you falls out of me in these words from time to time’.
This PhD has been a long time in the making. As with most journeys in my life I have walked the country mile. I have had many educational and professional experiences, that by dint of the place where and the generation into which I was born, I was never destined to have. I am especially grateful to those who have, on this journey, judged me by my merit and not by my gender, my accent, my class or my profession. I am where I am in part, because of you and I hold each of you in my heart always.
Thank you, Chris, my devoted and ever patient husband of thirty years. You have looked after me throughout this journey as you always do and as I always need to be-by watching over me and deploying wit and wisdom in equal measure, PRN. Thank you for the endless cups of tea and coffee and for your patience, generosity and sacrifice, which has, throughout, been immense. I could not have done this without you and I love you with all my heart and soul now and always.
Thank you to my friends and colleagues who have chivvied me along through this PhD and for believing in me, I treasure you all. Marie Armstrong for your constancy in encouraging me and your wise counsel and sound and practical problem solving when needed. Richard Fox, my friend, colleague and CBT clinical supervisor, you are the third eye in this thesis. Jane Lowey our clinical team secretary- you make a difference to all the lives you touch. Tim Carter and Tim Sweeney your empathy and help at key moments has been received with heartfelt gratitude. The managers and clinical leaders in Nottinghamshire Healthcare NHS Foundation Trust who supported the RCT and subsequently the establishment of the permanent SDS. My good friend Charles, your daily WhatsApp messages of encouragement have helped keep me going over the last 12 months. My friends at book club (in alphabetical order -Catherine, Chris, Lynne, Marie and Mel) our choice of literature, whether bringing edification or ennui (in the case of most of my choices), has been outshone only by our joyous and stalwart companionship. Our literary reveries have brought welcome respite from statistical equation modelling. The grandchildren, Grace, George, Elsie and Emme you have taught me so many things that a PhD never could -shame totems (Grace), Minecraft (George), Shimmer and Shine (Elsie and Emme) -my life is richer for your presence in it -thank you to you and your parents, Sara and Phil-know that you are loved and cherished.
I would like to thank all the members of the CLAHRC-NDL research team who have supported me throughout this PhD study, with special thanks to Boliang Guo and Cath Kaylor -Hughes, you made a big difference when I needed it. Gratitude also to Professor Paul Gilbert for sharing your time and intellect and good humour and for teaching me first-hand the theory and practice of CFT. A special thanks also goes to the staff at Duncan McMillan Library at the Trust who have been unstinting in their assistance in helping me find obscure publications. Your cheerful and willing disposition and tenacity in searching has helped enormously throughout this process.
Finally, with all my heart I wish to thank, in equal measure, my two PhD supervisors (in alphabetical order) Professor Patrick Callaghan and Professor Richard Morriss, who at different times held the role as my primary supervisor. You have both, with immense good grace, constancy and kindness walked these PhD country miles with me, which has been both a privilege and an honour. You have shown generosity in sharing your time, of which, I know, there is never enough. Your intellects are a privilege to behold and your clinical and academic acumen throughout this period of study has at different times, in equal measure, offered both inspiration and solace. We share a common bond in placing patients at the heart of our work, with the determination as clinicians, academics and educators, to advance knowledge and develop clinical interventions for complex mental health problems. With great affection and deep respect, thank you.
Preface
This study was part of a larger National Institute of Health Research (NIHR) funded randomised controlled trial (RCT) investigating the clinical and cost effectiveness of a Specialist Depression Service (SDS) offering NICE recommended pharmacological and psychological (CBT and MBCT) treatments, to patients diagnosed with persistent, treatment resistant depression. The RCT was part of a CLAHRC-NDL programme grant which ran between 2008–2013. I was a grant holder on the project alongside Professor Richard Morriss the lead for CLAHRC-NDL and one of my PhD supervisors. At the time of commencing this PhD I was employed as Consultant Nurse in Psychological Therapies in Nottinghamshire Healthcare NHS Trust, where the study was based. I was clinical lead for the SDS and for the RCT in service.
Regarding the PhD study I designed the research questions, chose the measures to be tested and the qualitative data collection and analysis process. The quantitative data was collected by the trial research associates. However, I completed my own data entry for the three psychometric measures tested in this thesis and under supervision of the team statistician Dr. Boliang Guo and Professor Morriss conducted the statistical analysis for these measures. I collected and analysed the qualitative data under the supervision of Professor Patrick Callaghan.
The ideas tested in this thesis emerge directly from my clinical work and the proposed model presented in the final chapter of this thesis is my own original work building, on the existing evidence base in the field of depression and founded in thirty years of my career working clinically and academically with people diagnosed with depression.
Contents
Abstract
Associated outputs
Associated training
Acknowledgements
Preface
List of Figures
List of Tables
List of Abbreviations
Chapter one
Introduction and overview
The significance of the study
Depression and co-morbid disorders
Motivation for conducting this study
The cognitive science of depression
The evidence base for Cognitive Behaviour Therapy (CBT)
Defining depression
Defining and treating persistent, treatment resistant depression
CBT Treatments for Depression
The way forward in persistent, treatment resistant depression
Chapter 2
Literature Review
Introduction
ThePracticality of theories: Defining a decision-making process
The conundrum of defining Shame as an affect
Cognitive-affective models of shame
Cognitive-Attributional theories of shame
Lewis’ attributional theory of self-conscious emotions
Standards, Rules and Goals (SRG’s)
Internal versus external evaluations
Attributions about self: Global versus Specific
Tracy and Robin’s appraisal-based process model of self-conscious emotions
Step 1: Survival-Goal Relevance
Step 2: Attentional Focus on Self and Activation of Self-Representations
Step 3: Identity-Goal Relevance
Step 4: Identity-goal congruence
Step 5: Internality attributions
Step 6: Stability, Globality, controllability attributions
Applying appraisal-based process models of self-conscious emotions in research
The evolutionary and biopsychosoical psychology model of shame
The definition of self-criticism
The psychoanalytic Formulation of Self-criticism
The Behavioural Formulation of Self-criticism
The cognitive formulation of self-criticism
76 The Attributional Theory formulation of self-blame
The evolutionary formulation of self-criticism
Theories of the nature and origins of self-criticism and self-blame
Defining compassion and self-compassion
An evolutionary formulation of compassion
87 Compassion as an appraisal elicited emotion
Compassion as a motivational system
Definition of self-compassion
Self-kindness versus self-judgment
Common humanity versus isolation
Mindfulness versus over identification or avoidance
Examining the Practicality of these theories of shame using Brawley’s criteria
A critique of Gilbert’s theory of shame
Why is the proposed study needed?
Chapter 3
Methods
Introduction
Research aims and objectives
Study Design
Philosophical Pragmatism as an epistemological foundation
Convergent Parallel Mixed Methods
PhD Study Context
The Study Sample
Sampling
The power calculation in this PhD study
Sample size
Recruitment Process
Inclusion and exclusion criteria for the RCT
Data Collection Methods
Detailed Description of Quantitative Data Collection Method
Step 1: Testing the psychometric status of OAS; FSCR and SCS
129 Rationale for chosen measures of shame, self-criticism and self-compassion
An overview of each measure
Other as Shamer Scale (OAS)
The forms of self-criticising/attacking and self-reassuring scale (FSCRS)
Self Compassion Scale (SCS)
Step 2: Modelling variance in depressive symptoms against shame, self-criticism and self- compassion
Rationale for chosen measures of depression
An overview of each depression measure
Hamilton Depression Rating Scale-17 (HDRS-17)
Beck Depression Inventory-I (BDI-I)
The Patient Health Questionnaire (PHQ-9)
Step 3: Exploring patients lived experience of shame, Self-criticism and self-compassion
Procedure for quantitative data collection
Description of Qualitative Data Collection Method
Quantitative data analysis
Establishing reliability and validity of the OAS, FSCR and SCS
144 Defining reliability
Defining validity
Testing reliability
Internal consistency
Modelling variance of depression in relation to shame, self-criticism and self-compassion
The argument for epistemological coherence: The Primacy of Praxis revisited
Ethical considerations
Data Management
Confidentiality
Process for obtaining informed consent
Fieldwork and safety guidelines
Ethics Approval to conduct this research
Chapter 4
Quantitative Results
Introduction
Question 1: To test the psychometric properties of the OAS, FSCSR and SCS in a cohort of patients
diagnosed with persistent, treatment resistant depression:
1. Descriptive statistics
2. Inferential statistics
I. Reliability
155 ii. Validity:
Question 2: To examine the degree to which variance in scores on depression measures taken at baseline can be accounted for by variance in levels of shame, self-criticism and self-compassion157
I. Univariate and multivariate regression analysis
The demographic profile of the study cohort
Healthy
Controls
Descriptive Statistics for Other as Shamer Scale (OAS) baseline
Reliability for Other as Shamer Scale (OAS) baseline
Split-Half Reliability for OAS at baseline
Test-retest reliability for OAS at baseline and 6 months
Confirmatory Factor Analysis (CFA)
Confirmatory Factor Analysis for Other as Shamer Scale
Descriptive Statistics for Forms of Self-Criticising Self -Reassuring Scale (FSCRS)
Reliability of the FSCSR at baseline
177 Split half reliability for the FSCSR at baseline
Test-retest reliability for FSCSR at baseline and 6 months
Confirmatory Factor Analysis for the Forms of Self-Criticism and self-Reassurance Scale (FSCSR) 186
Descriptive Statistics for Self-Compassion Scale (SCS) baseline
Reliability of SCS at baseline
Split half reliability for SCS at baseline
Test-retest reliability for SCS at baseline
Confirmatory Factor Analysis (CFA) for SCS
Objective 2: To determine how levels of shame, self-criticism and self-compassion correlate with
level of depression
Chapter 5
Qualitative results
Reflexivity
215 Emergent themes and sub-themes in the qualitative data
1. Childhood adversity and the social milieu
(i) No expectation
(ii) Every expectation
(iii) Behind closed doors
Reluctance to speak about childhood
3. Sense of self
224 I. Not good enough/inferior/failure-self-criticism
224 ii. unimportant/not counting/not worthy-self-blame
227 iii. Bad/inadequate/insignificant/worthless: self-hate/loathing
3. The function of self-criticism/self-hating
4. Absence of self-compassion
240 i. Intellectual appreciation with good intentions
240 ii. Not understood/incomprehension
Risky
iv. Not deserved
5. Avoidant coping
7. Memory and information processing biases in depression
Summary
[[#_Toc526213][Chapter
[[#_Toc526214][Discussion
[[#_Toc526215][Introduction
Summary of
Findings
Examination of the psychometric properties of the OAS, FSCSR and SCS in the study cohort
Examination OAS by sub-scale
Sub-scale inferior
Sub-scale emptiness
Sub-scale mistakes
Suggested revisions to the OAS
Previous studies of the psychometric properties of the OAS
Examination of the FSCSR and its sub-scales in relation to persistent treatment resistant depression
Subscale Inadequate self
Subscale Hated self
262 Subscale Reassured self
Previous studies of the psychometric properties of the FSCSR
Examination of the SCS by sub-scale in relation to persistent treatment resistant depression .267
Previous studies of the psychometric properties of the SCS
Summary of quantitative and qualitative data in this PhD thesis in the context of Gilbert’s
evolutionary biopsychosocial model
A continuum of shame and self-criticism and absence of self-compassion in persistent, treatment resistant depression
Defining the parameters of approval and subjugation
Shame of not meeting expectation: Every expectation
Shame, ridicule and humiliation: No expectation
Riven with shame: trapped and defeated
Clinical implications of these findings and avenues for future research
Strengths of this study
Limitations of this study
Conclusion
References
Appendices
Appendix I: Continuum of Schools of Cognitive Behavioural Psychotherapies (adapted from Gilbert 2007b)
Appendix II: Table of summary of the biological, psychological, genetic and clinical correlates of
Treatment Resistant Depression
(from Murphy, Saris and Byrne 2017 p. 4)
Appendix III: Proposed criteria for Multiple-Therapy-Resistant (MTR) Major Depressive Disorder
Appendix IV: A theoretical process model of self-conscious emotions (Tracy and Robins 2007a p10)
Appendix V: Appraisal model of compassion illustrating how witnessing negative outcomes
leads to felt compassion with moderation of relevance to self
(from Goetz, Keltner and Simon-Thomas 2010 p 356)
Appendix VI: Theories of shame measured against Brawley’s (1993) Practicality of a theory criteria
Appendix VII: Consort diagram of participant flow through RCT (from Morriss, Garland, Nixon, Boliang, et al, 2016)
Appendix VIII: Email invitation to participate as a healthy control in the study
Appendix IX: Healthy Controls: Screening Questionnaire
Appendix X: Participant Information Sheet
Appendix XI: Healthy Controls Participant Consent Form
Appendix XII: Other as Shamer Scale
Appendix: XIII: The Forms of Self-Criticising and Self-Reassuring Scale (FSCRS)
Appendix XIV: Self Compassion Scale (SCS)
How I Typically Act Towards Myself in Difficult Times
Appendix XV: Hamilton Depression Rating Scale-17 (Hamilton, 1960)
Appendix XVI: Beck Depression Inventory-I (BDI-I)
Appendix XVII: The Patient Health Questionaire-9 (PHQ-9)
Appendix XVIII: Qualitative Interview Topic Guide
Appendix XIX: Histogram and box plot for the OAS sub-scale inferior at baseline
Appendix XX: Histogram and box plot for the OAS sub-scale emptiness at baseline
Appendix XXI: Histogram and box plot for the OAS sub-scale mistakes at baseline
Appendix XXII: Histogram and box plot for the FSCSR sub-scale inadequate self at baseline ....371 Appendix XXIII: Histogram and box plot for the FSCSR sub-scale hated self at baseline
Appendix XXIV: Histogram and box plot for the FSCSR sub-scalereassured self at baseline
Appendix XXV: Histogram and box plot for the SCS sub-scale self-kindness at baseline
Appendix XXVI: Histogram and box plot for the SCS sub-scale self-judgement at baseline
Appendix XXVII: Histogram and box plot for the SCS sub-scale common humanity at baseline 376
Appendix XXVIII: Histogram and box plot for the SCS sub-scale isolation at baseline
Appendix XXIX: Histogram and box plot for the SCS sub-scale mindfulness at baseline
Appendix XXX: Histogram and box plot for the SCS sub-scale overidentification at baseline ....379
Appendix XXXI: Example of steps of qualitative data analysis (participant 12)
Appendix XXXII: Photographs of an example of a mind map (participant 12)
Appendix XXXIII: Biographies of participants in qualitative arm of this PhD study
Appendix XXXIV: The subscales and items of the OAS
Appendix XXXV: The sub-scales and items of the FSCSR
Appendix XXXVI: The items and sub-scales of the SCS
List of Figures
Figure 1: Empirically Grounded Clinical Interventions (Salkovskis 2002)
Figure 2: Lewis’s cognitive- attributional theory of self-conscious emotions (Lewis 2000 p
Figure 3: Lewis’ proposed relationship between shame and psychopathology (Lewis, 2000, p
Figure 4: An evolutionary and biopsychosocial model of shame (Gilbert 2007a p.301)
Figure 5: Convergent parallel mixed methods design (Creswell and Plano-Clark (2011, p 69)
Figure 6: Confirmatory Factor Analysis path diagram for the Other as Shamer Scale (OAS)
Figure 7: Confirmatory Factor Analysis path diagram for the Forms of Self-Criticising and Self-Reassuring Scale (FSCSR)
Figure 8: Confirmatory Factor Analysis path diagram for the Self Compassion Scale (SCS) . 202 Figure
9: Formulation of a continuum of shame, self-criticism and absence of self- compassion in persistent treatment resistant depression
List of Tables
Table 1: DSM-5 Diagnostic criteria for Major Depressive Disorder (APA 2013 p 160–161)
Table 2: DSM-5 Diagnostic Criteria for Persistent Depressive Disorder (APA 2013 p 168–169)
Table 3: DSM-5 Diagnostic Criteria for Bi-polar II Disorder (APA 2013 p 132–139)
Table 4: Summary of data collection and analysis methods
Table 5: Types of questions for in-depth interviews
Table 6: Demographic characteristics of the study cohort at baseline
Table 7: Participants clinical characteristics of depression at baseline
Table 8: Secondary clinical characteristics of the study cohort at baseline
Table 9: Mean scores (SD) on HDRS-17 and BDI-I for healthy control group versus study cohort
Table 10: Summary statistics for OAS at baseline
Table 11: Distribution for each sub-scale of OAS at baseline
Table 12: Cronbach’s Alpha scores at baseline for OAS scale
Table 13: Item statistics for sub-scale inferior at baseline
Table 14: Item statistics for sub-scale inferior at baseline
Table 15: Item statistics for sub-scale emptiness at baseline
Table 16: Item to item correlation for sub-scale emptiness at baseline
Table 17: Item statistics for sub-scale mistakes at baseline
Table 18: Item to item correlation for sub-scale mistakes at baseline
Table 19: Summary item means statistics for OAS at baseline
Table 20: Split Half Reliability scale statistics for OAS at baseline
Table 21: Test-retest reliability for OAS at baseline and 6 months
Table 22: The continuous latent variables and indicators tested for OAS, FSCSR and SCS ... 173
Table 23: Model Fit indices for OAS
Table 24: Summary statistics for FSCSR at baseline
Table 25: Distribution for each sub-scale of FSCSR at baseline
Table 26: Cronbach’s Alpha for FSCSR at baseline
Table 27: Item statistics for sub-scale inadequate self at baseline
Table 28: Item to item correlation for sub-scale inadequate self at baseline
Table 29: Item statistics for sub-scale hated self at baseline
Table 30: Item to item correlation for sub-scale hated self at baseline
Table 31: Item statistics for sub-scale reassured self at baseline
Table 32: Item to item correlations for sub-scale reassured self at baseline
Table 33: Summary item means statistics for FSCSR at baseline
Table 34: Split half reliability scale statistics for FSCSR at baseline
Table 35: Test -retest reliability for FSCSR between baseline and 6 months
184 Table 36: Model Fit indices for FSCSR
Table 37: Summary statistics for Self-Compassion Scale (SCS) at baseline
Table 38: Distribution for each sub-scale of SCS at baseline
Table 39: Cronbach’s Alpha for SCS at baseline
Table 40: Item statistics for sub-scale self-kindness at baseline
Table 41: Item to item correlation for sub-scale self-kindness at baseline
Table 42: Item statistics for sub-scale self-judgment at baseline
Table 43: Item to item correlations for sub-scale self-judgement at baseline
Table 44: Item statistics for sub-scale common humanity at baseline
Table 45: Item to item correlations for sub-scale common humanity at baseline
Table 46: Item statistics for sub-scale isolation at baseline
Table 47: Item to item correlations for sub-scale isolation at baseline
Table 48: Item statistics for sub-scale mindfulness at baseline
Table 49: Item to item correlations for sub-scale mindfulness at baseline
Table 50: Item statistics for sub-scale overidentification at baseline
Table 51: Item to item correlations for sub-scale overidentification at baseline
Table 52: Summary item means for SCS at baseline
Table 53: Split Half Reliability scale statistics for SCS at baseline
Table 54: Test retest for SCS at baseline and 6 months (**. CORRELATION is significant at 0.01 level (2 tailed)
Table 55: Model Fit indices for SCS
Table 56: Influence of OAS, FSCSR and SCS on HRSD-17 by univariate and multivariate regression modelling
Table 57: Influence of OAS, FSCSR and SCS on BDI-I univariate and multivariate regression modelling
Table 58: Influence of OAS, FSCSR and SCS on PHQ-9 univariate and multivariate regression modelling
207 Table 59: Definition of ‘cognition’ within IPA
List of Abbreviations
ACT: Acceptance and Commitment Therapy
APA: American Psychiatric Association
ATTS: Attitudes Towards Self Scale
ASQ: Attributional Style Questionnaire
BA: Behavioural Activation
BABCP: British Association of Behavioural and Cognitive Psychotherapies
BAP: British Association of Pharmacology
BDI-I: Beck Depression Inventory-I
BMI: Body Mass Index
CAT: Cognitive Analytic Therapy
CBASP: Cognitive Behavioural Analysis System
CBT: Cognitive behaviour Therapy
CFA: Confirmatory Factor Analysis
CFI: Comparative Fit Index
CFT: Compassion Focused Therapy
CLAHRC-NDL: Collaboration for Leadership in Applied Health Research and Care
CT: Cognitive Therapy
CVD: Cardiovascular Disease
DALY’s: Disability Adjusted Life Years
DoH: Department of Health
DEQ: Depressive Experiences Questionnaire
DSM: Diagnostic and Statistical Manual
DD: Double Depression
EFA: Exploratory Factor Analysis
FSCSR: Forms of Self-Criticism/Self-Reassurance Scale
GAF: Global Assessment of Functioning
GBD: Global Burden of Disease
HDRS-17: Hamilton Depression Rating Scale-17
ICD: International Classification of Diseases
IPA: Interpretative Phenomenological Analysis
IPT: Interpersonal Therapy
MBCT: Mindfulness Based Cognitive Therapy
MDD: Major Depressive Disorder
MSC: Mindful Self Compassion
NEMESIS: Netherlands Mental Health Survey and Incidence Study
NHS: National Health Service
NICE: National Institute for Health and Care Excellence
NIHR: National Institute for Health Research
NIMH: National Institute of Mental Health
NMC: Nursing and Midwifery Council
OAS: Others As Shamer Scale
PFQ-2: Personal Feelings Questionniare-2
PDD: Persistent Depressive Disorder
PTSD: Post Traumatic Stress Disorder
RCT: Randomised Controlled Trial
RSMEA: Root Mean Squared Error of Approximation
SCID: Structured Clinical Interview for DSM-IV
SCS: Self Compassion Scale
SDS: Specialist Depression Service
SEM: Standard Error of Measurement
STAR*D: Sequenced Treatment Alternatives to Relive Depression
SCL-90: Symptom Checklist-90
SPSS: Statistical Package of the Social Sciences
TAU: Treatment as Usual
TOSCA: Test of Self-Conscious Affect
TLI: Tucker Lewis Index
WHO: World Health Organisation
WMA: World Medical Association
WLSMV: Weighted Least Square Mean Variance adjusted
YLD’s: Years Lived with Disability
Chapter one: Introduction and overview
The significance of the study
In 1973 Martin Seligman, in reference to the rate of diagnosis, described depression as ‘the common cold of psychiatry’. Over the proceeding four decades it has been suggested depression is reaching near pandemic levels in terms of both incidence and disease burden (Kramer, 1983). More recent and statistically rigorous epidemiological studies have challenged the idea that depression has reached epidemic proportions. Whilst Baxter, Scott, Ferrari, Norman, Vos and Whiteford (2014) found a 37% increase in prevalence of depression between 1990–2010, this can be predominately accounted for by population growth and ageing (cf: Whiteford, Degenhardt, Rehm, Baxter, Ferrari, Erskine, Charlson, Norman, Flaxman, Johns, Burstein, Murray and Vos 2013). Following the publication of the findings of the first World Health organisation (WHO) Global Burden of Disease (GBD) study in 2000 depression was declared ‘a major public health problem that affects patients and society’ (Ustun, Ayuso-Mateos, Chatterji, Mathers and Murray 2004). It is estimated depression affects over 120 million people worldwide with a lifetime prevalence ranging from 10% — 15% (Lepine and Briley 2011).
It is well established in the research literature that depression is a relapsing illness. The National Institute of Mental Health (NIMH) conducted a 10-year prospective observational study examining the recovery from and recurrence of major depressive disorder (Solomon, Keller, Leon, Mueller, Lavori, Shea, Coryell, Warshaw, Turvey, Maser and Endicott 2000). Recovery was defined as experiencing no symptoms of major depression or one or two symptoms at a mild level severity for a period of eight weeks. Meanwhile, recurrence was defined as meeting the diagnostic criteria for full Major Depressive Disorder (MDD) for at least two consecutive weeks. Recovery was only deemed to have occurred after an individual had first recovered from the preceding episode. Episodes of minor depressive disorder and chronic depression were excluded from statistical analysis. The study cohort consisted of 318 participants diagnosed with unipolar major depression who recovered from their intake episode and of these, 202 went on to experience a recurrence. The cumulative risk of recurrence at 1 year was 25%, at 2 years 42% and at 5 years 60%. Of these 202 who suffered a recurrence 172 recovered and were at risk of recurrence. Of these 172, 115 went on to experience a second recurrence and for this sub-group the cumulative probability of recurrence at 1 year was 41%, at 2 years 59% and at 5 years 74% (Solomon, Keller, Leon, Mueller et al 2000).
Overall, at each time point the cumulative probability of recurrence increased and the time to recurrence between each episode decreased, with the number of lifetime episodes of major depressive disorder being significantly associated with recurrence over the study period. Conversely, as the duration of recovery persisted the risk of recurrence reduced. The authors conclude that the probability a relapse of major depressive disorder is significantly influenced by the number of lifetime episodes experienced before any period of recovery or wellness. Further, with each successive episode the probability of recurrence increases, with the risk of recurrence increasing by 16% with each successive episode (Solomon, Keller, Leon, Mueller et al 2000). This study built on previous research by the authors (Keller, Lavori, Lewis and Klerman (1983) who examined predictors of relapse in depression and concluded that individuals diagnosed with unipolar depression are, most at risk of relapse following their first depressive episode. Further, if relapse does occur, they have a 20% chance of their illness taking a chronic course and with each subsequent relapse the chance of further relapses also increases. This in turn built on a body of research examining depressive recurrence and relapse across five decades (Murphy, Saaris and Byrne 2017; Fava 2003; Kupfer, Frank, Perel, Cornes, Mallinger, Thase, McEachran and Grochocinski 1992; Belsher and Costello 1988; Lee and Murray, 1988; Nystrom 1979).
Taking this lifetime risk of relapse and recurrence into consideration the human and economic cost of depression is immense. The second WHO GBD study published in 2010 cites that within the mental and substance use disorders group, at 40.5%, depressive disorders account for the highest proportion of burden across all mental disorders both in terms of the most
Disability-Adjusted-Life-Years (DALY’s) and, at 42.5%, the most Years-Lived with Disability (YLD’s). Further, in terms of the ten leading causes of total burden in 2010, mental disorders and substance use disorders accounted for 7.4% DALY’s and 22.9% YLD’s (Whiteford, Degenhardt, Rehm, Baxter, et al, 2013). A more recent WHO Global Burden of Disease (GBD) study (GBD, 2017), identified depression as possessing the greatest global burden of disease and declared it to be the leading cause of DALY’s (DALY’S) lost due to ill-health.
When considering persistent, treatment resistant depression, the focus of this PhD study, then those experiencing this form of depressive disorder are less productive, experience greater medical co-morbidity (see below for a more detailed discussion) and make more suicide attempts (Amital, Fostick, Silberman, Beckman and Spivak (2008). Rhebergen, Beekman, Graaf, Nolen, Spijker, Hoogendijk and Penninx (2010) using data from the Netherlands Mental Health Survey and Incidence Study (NEMESIS), conducted a study with a cohort of 7076 participants aged between 18–64 years. Data gathered over a three year period between 1996–1999, examined the recovery trajectories for social and physical functioning for participants diagnosed with Major Depressive Disorder (MDD) and/or dysthymia and what is termed ‘Double Depression’ (DD), dysthymia superimposed over MDD. The study found that compared to participants with no diagnosed depressive disorder all depressed groups showed significant impairment in terms of social and physical functioning. Dysthymia and DD had lower post-morbid physical functioning compared to MDD, after one year and three years. In addition, the study found that impaired social functioning was determined by neuroticism and impaired physical functioning by age, a co-occurring somatic complaint and neuroticism.
Depression and co-morbid disorders
Depression often exists co-morbidly with other mental health problems, notably, anxiety disorders, and with chronic physical health conditions. A study published in 2007 found that depressive and anxiety disorders were independently related to a range of chronic physical health conditions, with heart disease and chronic pain showing the strongest association with depressive and anxiety disorders (Scott, Bruffaerts, Tsang, Ormel, Alonos, Angermeyer, Benjet, Bromet, Giroamo, Graaf, Gasquet, Gureje, Haro, He, Kesselr, Levinson, Mneimneh,
Okaley-Browne, Posada-Villa, Stein, Takeshmia and Von Korff, 2007). Results from the World Health Survey (Moussav, Chatterji, Verdes, Tandon, Patel and Ustun, 2007) compared depression with four other chronic physical health conditions: angina, arthritis, asthma and diabetes and examined how the decline in health status associated with depression (Chapman, Perry and Strine 2005) compared with the decline in health status in these four chronic physical health conditions, alongside, what is the added effect of suffering with depression plus one or more of these chronic physical health conditions. This study showed that comorbidity between depression and chronic physical health conditions is common and that individuals suffering with a chronic physical health condition are more likely to suffer with depression than those with no such conditions. Also, depression is associated with a greater decline in overall health status than any of the four chronic physical health conditions studied. Further, depression co-occurring with any of these chronic physical health conditions results in a significantly greater decline in health status than from suffering from one or more of the physical health conditions alone. This decline in health status is accentuated further where depression and diabetes occur co-morbidly (Moussav, Chatterji, Verdes, Tandon, et al, 2007).
Chapman, Perry and Strine (2005) conducted a review of the research literature looking at the relationship between depression and asthma, arthritis, cardiovascular disease, cancer, diabetes and obesity. This comprehensive review yields sobering data. Briefly these can be summarised as follows from Chapman, Perry and Strine (2005). Almost 50% of people diagnosed with asthma report significant symptoms of depression, particularly where symptoms are disruptive to day to day functioning or are difficult to control. Similarly, for people with arthritis symptom severity and recurrence and restriction in mobility were correlated with greater severity of depression. The link between depression and cardiovascular disease (CVD) is well established. Depression is associated with risk factors for CVD such as smoking and reduced physical activity. In addition, those suffering with depression are more likely to suffer coronary artery disease and the risk of developing coronary heart disease is 1.6 times greater if the person also experiences depression. Depression is also predictive of a stroke and a person with significant depressive symptoms is twice as likely to have a stroke as someone with fewer symptoms. Depression is also associated with an increased risk for morbidity and mortality for a stroke and the onset of depression is common following a stroke. Equally, a person with a history of major depressive disorder is four times more likely to suffer a myocardial infarction than someone without such a history. In cancer, 21% of cancer patients are reported to be experiencing depression and increased depressive symptoms reduces survival rates. Depression is twice as common among people with diabetes as those without and its occurrence is associated with factors including coming to terms with the illness itself, diabetic complications, unemployment and the degree to which diabetes interferes with activities of daily living. Regarding obesity the authors note that most obese people do not suffer with a mood disorder, but the literature does reveal a significant positive relationship between Body Mass Index (BMI) and depressive symptoms. The authors conclude by highlighting the reciprocal relationship between chronic disease and depressive disorders and observe that, as discussed above, untreated depression is likely to develop into a chronic condition in its own right.
Motivation for conducting this study
The author of this thesis is a mental health nurse by profession and is trained in both behavioural and cognitive psychotherapy, with 30 years’ experience of using cognitive and behavioural interventions to treat persistent, treatment resistant depression. The author can be described as a clinical academic working in both a National Health Service (NHS) specialist depression service and academia, both as a trial therapist in two randomized controlled trials
(RCT) (Morriss, Garland, Nixon, Boliang Guo, James, Kaylor-Hughes, Moore, Ramana,
Sampson, Sweeney, and Dalgleish, 2016; Paykel, Scott, Teasdale, Johnson, Garland, Moore, Jenaway, Cornwall, Hayhurst, Abbott and Pope, 1999), a researcher and an educator.
The authors approach to research is founded in the Scientist Practitioner paradigm (Salkovskis 2002) and the motivation for choosing this PhD focus is clinical curiosity regarding the limitations of both cognitive and behavioural interventions when working with persistent, treatment resistant depression. Salkovskis (2002) observes that when a patient does not respond to a specific treatment intervention then the limitation resides in the intervention (not the patient and their clinical presentation) and he advocates utilising ‘empirically grounded clinical interventions’ (Salkovskis 2002) which brings together data from a range of sources (see figure 1 below) to develop more effective cognitive and behavioural clinical interventions.
][<strong>FIGURE 1: EMPIRICALLY GROUNDED CLINICAL INTERVENTIONS (SALKOVSKIS 2002)</strong>
Theory outcome research clinical guideline i.e. NICE
As Cuijpers, Berking, Andersson, Quigley, Kleiboer and Dobson (2013) observe, Cognitive Behaviour Therapy (CBT) is the most researched psychotherapy modality for adult depression. In a recent meta-analysis, the authors observe a fundamental challenge that exists not just for the researcher conducting a meta-analysis but for the practitioner of CBT, namely, how CBT is defined. This debate exists in all aspects of the CBT literature and clinical practice. Gilbert (2007b) identifies at least sixteen schools of cognitive and behavioural psychotherapies (see appendix 1) and describes the acronym CBT as an umbrella term that incorporates a broad church of theoretical orientations and attendant clinical interventions. As appendix I Illustrates this broad church spans a range of orientations from the traditional behavioural theories and models (i.e. Marks 1981) through to the Beckian cognitive perspective (Moore and Garland 2003; Fennell, 1989; Beck, Rush, Shaw and Emery, 1979) and what are considered to be more integrative approaches such Interpersonal Processes in Cognitive Therapy (Safran and Segal 1996) and Ryle’s Cognitive Analytic Therapy (CAT)(Ryle and Kerr, 2002). The evidence base for these different schools housed under the CBT umbrella is variable. It can also be said that the more integrative approaches, which draw on a combination of behavioural, cognitive, psychodynamic, gestalt and interpersonal psychotherapy theory and practice such as Schema Focused Therapy (Young, 2003; 1990;
Layden, Newman, Freeman and Eyers-Mors, 1998) Cognitive Analytic Therapy (Ryle and Kerr, 2002) and Dialectic Behaviour Therapy (Linehan, 1993) have, Like Beckian cognitive therapy itself, (see Weishaar 1993 for a biographical account of the development of Beckian cognitive therapy) emerged from clinical observation. This is often in the context of a clinical need to develop interventions for working with more complex clinical presentations where standard cognitive and behavioural interventions delivered within a standard treatment rationale have limited impact in terms of ameliorating symptomatology and social functioning.
The author of this thesis would, under the CBT umbrella, primarily align herself with cognitive therapy (Kinsella and Garland, 2008; Moore and Garland 2003). Further, in keeping with the Scientist Practitioner paradigm, the author would advocate utilising clinical interventions that have a coherent theoretical underpinning in terms of the cognitive and behavioural science (theory) and evidence base (experimental and outcome research) and from this should emerge a cogent clinical treatment rationale that forms the basis of clinical interventions. Frequently within both research and clinical practice behavioural and cognitive theories, rather than being integrated into coherent model, are inelegantly mixed in a way that the science is poorly articulated, and the intervention becomes technique orientated rather than theoretically derived and driven. As a result, there is often a disconnect between the theory underpinning the CBT model and the attendant clinical interventions.
The authors interest in Compassion Focused Therapy (CFT) (Gilbert, 2010b) began fifteen years ago following a workshop (Gilbert, 2007b) on the subject delivered by its founder Professor Paul Gilbert. At this time Gilbert proposed that CFT was a method of formulating emotional disorders that can be integrated into any psychotherapy modality. The author also received clinical supervision in the CFT approach over a three-year period (2010–2013) from Professor Gilbert whose own clinical origins lie in CBT. The authors clinical work with patients experiencing persistent, treatment resistant depression led to two important clinical observations. Firstly, that self-criticism was a key feature of their clinical presentation and secondly that standard Beckian clinical interventions that traditionally target self-criticism, notably challenging negative automatic thoughts and modifying conditional beliefs in the context of targeting low self-esteem (Fennell 1998) had limited impact in tackling self-critical thought processes. Further, when using cognitive interventions some patients would frequently articulate, what is referred to as the ‘head heart lag’, namely responding with ‘I see what you are saying (intellectually) but I don’t really believe it (emotionally)’. Among the patients who made such observations, it was often those who described childhoods characterised by sustained emotional abuse (Muris and Meesters 2014; Liu, Alloy, Abramson, Iacoviello and Whitehouse 2009; Alloy, Abramson, Smith, Gibb, and Neeren 2006; Bernet and Stein, 1999) and marked affectionless over control (Patton, Coffey, Posterino, Carlin and Wolfe, 2001), who exhibited high levels of self-criticism and pervasive avoidant cognitive, emotional and behavioural coping strategies. It was these clinical observations that led to the consideration of what factors might be impeding the effectiveness of cognitive and behavioural interventions for clients experiencing persistent, treatment resistant depression and following Paul Gilbert’s work (Gilbert, 2017a; 2007a; 2005b; 2003; 1998; 1995; 1997; 1992)I began to consider the role of shame in depression.
As is discussed in detail in chapter 3, shame and its psychological sequela are articulated across a broad range of academic disciplines and psychotherapy modalities, including Beckian cognitive therapy (Beck, Rush, Shaw and Emery, 1979). However, traditionally in mental health and psychiatry shame is formulated as a symptom of depression. Implicit within this formulation is the assumption that as depressed mood responds to both pharmacological and psychotherapeutic intervention then shame, and its sequela will be ameliorated without the need for targeted intervention. A further area of influence in my clinical and academic work is the cognitive science of depression. The clinical observation that led Beck to develop cognitive therapy was the spontaneous reporting of what he labelled negative automatic thoughts (see Weishaar 1993 p 19). In developing his early theoretical model Beck described negative thoughts as the cause of depression (Beck, 1963). Research in the cognitive science of depression has since demonstrated two well established factors that disprove this assertion. Firstly, the negative content to thought processes observed in depression are mood congruent and therefore a symptom of depression, rather than a causal factor (Bower, 1985; Teasdale, Taylor and Fogarty, 1980). That is, as depressed mood abates so does the negative tone of thought processes. This is a ubiquitous observation in clinical practice and has been demonstrated in experimental studies in cognitive science (see Harvey, Watkins, Mansell and
Shafran, 2004 for a comprehensive account) and in pharmacological studies (Peselow, Robins, Block, Barouche, and Fieve, 1990). The cognitive science of depression has some important observations to make regarding the formulation of self-criticism in depression. These observations are précised below.
The cognitive science of depression
Examining the ‘head heart lag’ phenomena from a cognitive science perspective Teasdale (1999) critiques Beckian cognitive therapy describing the model as a clinical model built from clinical observation and argues that, as a result, it does not account for the cognitive phenomena observed in depression. Here Teasdale is referring to the cognitive science of depression and the processes of self-critical and self-blaming rumination (Teasdale and Barnard, 1993), autobiographical memory bias (Williams and Broadbent, 1986) and over general memory (Watkins and Teasdale, 2004; 2001) which are considered by cognitive scientists to act in concert to maintain depressed mood. This literature is summarised briefly here from (Garland 2016).
When mood is depressed memory more readily recalls past, unpleasant, painful memories and actively screens out pleasant or neutral memories. In the cognitive science literature this is referred to as autobiographical memory (Williams, Barnhofer, Crane, Herman, Raes, Watkins, and Dalgleish, 2007). In addition, experimental studies (Raes, Hermans, Williams, Beyers, Eelen and Brunfaut, 2006; Williams and Broadbent 1986) demonstrate that people experiencing depression in comparison to non-depressed controls have difficulty moving through memory hierarchy to a specific level and tend to stop searching at a general description state. This is referred to as over general memory. A consistent finding in the cognitive science literature is that rumination is associated with both intensification and persistence of depressed mood (Nolen-Hoeksema 2000). Further, Watkins and Teasdale (2001) and Watkins, Teasdale and Williams, (2000) found that if rumination is experimentally reduced then memory becomes more specific. This has led Williams and colleagues to conclude that over-general memory and rumination are intertwined in a process where one exacerbates the other and that over-general memory arises in early development and may be linked to early trauma (Henderson, Hargreaves, Gregory and Williams, 2002). Williams, Barnhofer, Crane, Herman et al, (2007) conclude that over- general memory arises from a style of processing information in a verbally analytic way which manifests itself as depressive rumination. Importantly this process is outside of conscious awareness and serves the purpose of regulating affect and therefore is negatively reinforced (i.e. maintained) exactly because it enables this affect regulation. Williams, Barnhofer, Crane, Herman et al, (2007) therefore formulates over-general memory as an avoidant retrieval style which develops in early childhood and is aimed at reducing the recall of specific distressing memories. Williams,
Barnhofer, Crane, Herman et al, (2007) makes links to the work of Kuyken and Brewin (1995; 1994) who found that over general memory was associated with greater frequency and avoidance of intrusive, depressive memories. Thus, in early childhoods marked by trauma (i.e. emotional/physical/ sexual abuse/neglect) it can be argued that this proposed mechanism of affect regulation would be a useful default survival strategy in order to manage high levels of unregulated fear, anger, sadness and despair. However, this comes at a cost as this process of affect regulation reduces problem solving ability, impairs the capacity to be specific about future events, increases level of hopelessness and prolongs depressed mood (Williams, Barnhofer, Crane, Herman et al, (2007). Gilbert’s theory (Gilbert, 2007a) emphasises the role emotional memories play in activating threat systems in the brain, which in turn lead to the implementation of idiosyncratic safety strategies aimed at maintaining relational attachment. Of importance here are shame based traumatic emotional memories (Matos, Pinto-Gouveia and Costa, 2013). This is where this thesis began.
The evidence base for Cognitive Behaviour Therapy (CBT)
Whilst it is generally considered that the evidence base for CBT for depression is well established (National Institute for Health and Care Excellence (NICE) 2009) in recent years there has been questions raised regarding the true effect size of CBT for depression (Cuijpers, van Straten, Bohlmeijer, Hollon and Andersson 2010) with specific criticism of the early studies conducted by Beck and colleagues in the 1980’s. Notably, these criticisms include the observation that trials comparing CBT and pharmacotherapy utilised methodological factors that favoured CBT, and as a result, it can be argued such studies may have overestimated the efficacy of CBT for depression relative to antidepressant medication (Butler, Chapman, Forman and Beck 2006). Equally, with regards to antidepressant treatment trials some researchers question the veracity of the effect sizes reported on the grounds of publication bias (Turner, Matthews, Linardatos, Tell, and Rosenthal 2008). Such potential for bias has been reported in the CBT literature. Williams (1997) highlights the controversy surrounding the Elkin, Shea, Watkins, Imber, Sotsky, Collins, Glass, Pilkonis, Leber, Docherty, Fiester and Parloff (1989) research trial comparing CBT with pharmacotherapy and placebo and the lack of transparency regarding questions related to bias in how the data was analysed. In an increasingly politicised research environment, significantly influenced by economic drivers, such issues raise vital questions regarding the ethical practice of research and the dissemination of research findings and how results are utilised at a national and global level. This require researchers to endeavour to be diligent in upholding the principles of the Scientist- Practitioner paradigm and the World Health Organisation Guidelines for Good Clinical Research Practice (WHO 2005) within healthcare research. Hence there has been renewed endeavour to be more impartial and transparent in the reporting of research findings. In their 2010 meta-analysis of psychotherapy for depression study effect size and quality Cuijpers, van Straten, Bohlmeijer, Hollon et al (2010) concluded that one of the reasons effect sizes were overestimated in earlier meta-analyses is the inclusion of poorquality studies in those meta-analyses. In their 2010 study, only analysing higher quality studies of psychotherapy for adult depression yielded much smaller effect sizes than previous meta-analyses. This led to the conclusion that even controlling for the type of control group in the study, previous meta-analyses have overestimated the effect size of psychotherapy studies for adult depression (Cuijpers, van Straten, Bohlmeijer, Hollon et al 2010).
This led the authors to conduct a further, more robust meta-analysis (Cuijpers, Berking, Andersson, Quigley et al 2013) of CBT for adult depression both alone and in comparison to other treatments. In conducting the meta-analysis the researchers used a broad definition of CBT and compared CBT with control groups, pharmacotherapy and the following additional psychotherapies: non-directive supportive therapy, Behavioural Activation (BA), psychodynamic psychotherapy, Interpersonal Therapy (IPT), Problem Solving Therapy and what is termed ‘other psychotherapies’. From the 1,237 publications retrieved from the initial literature search, 115 RCT’s on CBT were included in the meta-analysis. Most of the studies used a community sample targeting adults with Major Depressive Disorder as the primary problem and used a Beckian (Beck, Rush, Shaw, Emery 1979) treatment protocol, with two thirds of the CBT treatments offering between 8–16 sessions. Most studies were conducted in the United States. The researchers deployed predetermined quality assessment and data extraction criteria and note that the quality of the studies included in the meta-analysis was not ideal in that only 43 of the studies chosen met at least three of the four quality criteria.
Their findings can be summarised as follows:
-
CBT has efficacy as a treatment for adult depression. The researchers compared CBT with wait list, care as usual and placebo or other control group and CBT was shown to be superior to all control groups. However, they note the effect size was significantly smaller in studies that compared CBT with placebo and/or other control groups, compared to CBT with waitlist or care as usual control groups (Cuijpers, Berking, Andersson, Quigley et al 2013 p 382).
-
The combination of CBT and pharmacotherapy is superior to pharmacotherapy alone in the treatment of depression. However, no difference was found for the efficacy between CBT and pharmacotherapy in direct comparison. The authors note this is not in keeping with previous meta-analyses that found superiority of CBT over antidepressants (Gloaguen, Cottraux, Cuccherat and Blackburn 1998; Dobson, 1989).
-
CBT was no more or less effective than the other psychotherapies included within the metaanalysis. However, the authors note the limitations of some of these comparisons given the small sample size for some of the psychotherapies reported. However, with reference to a previous meta-analysis conducted by themselves they conclude that: ‘differences between psychotherapies for the treatment of depression are small and
unstable across meta-analyses’
(Cuijpers, Berking, Andersson, Quigley, et al (2013 P. 384).
-
The authors also compared Cognitive Therapy (CT) trials with Cognitive-Behaviour Therapy (CBT) trials and concluded CT is no more effective than other forms of CBT.
Defining depression
There is much debate in the health sciences literature as to what is meant by the term ‘depression’ and its associated constructs. Summerfield (2006) observes the following:
‘in everyday usage, as much by doctors as by the general public. ‘depression’ can mean something figurative or literal, can denote a normal or abnormal state, and if abnormal either an individual symptom or a full-blown disorder. And though depression-as-disease may have acquired the status of a natural science category, this was an achievement rather than a discovery’
(Summerfield 2006, p 161)
This observation brings into focus the debate regarding the use of psychiatric diagnosis in both research and clinical practice. Central to modern healthcare and treatment is the concept of diagnosis. That is the classification of specific signs and symptoms of disease in order to define and categorise clinical syndromes. There are two main diagnostic systems used in mental health the WHO International Classification of Disease (ICD-10) (WHO, 1994) and the American Psychiatric Association (APA) Diagnostic and Statistical Manual (DSM-5) (American Psychiatric Association 2013), the latter being the system most frequently used for defining participant groups in research trials. This tradition of diagnosis also underpins the socalled disorder specific maintenance formulations in the cognitive and behavioural therapies (see Kinsella and Garland 2008) which form the foundations of the protocols designed to use in the randomised controlled trials on which the evidence for their efficacy is predicated. There is much controversy in both clinical and academic circles regarding the concept of diagnosis and how it is utilised in healthcare. Wykes and Callard (2010) offer a commentary on the potential of diagnosis to medicalise the human condition itself and its potential to accentuate feelings of stigma in relation to mental illness. These authors also observe how sole reliance on diagnosis can narrow access to treatment by dictating which treatments are deemed acceptable according to diagnosis.
In this PhD thesis diagnostic criteria have been utilised in order to define the population studied. This decision was dictated by the fact that the group studied in this thesis were a cohort of participants recruited to a research trial which used diagnostic criteria to define the population under study. The study (for which the thesis author was a grant holder) took a ‘pragmatic’ (used here in the everyday sense of its usage rather than philosophical definition described in chapter 3 of this thesis) definition of persistent depression (see Morriss, Garland, Nixon, Guo et al 2016), recruiting individuals who had not responded to treatment in secondary care mental health services for a period of at least 6 months and experiencing a primary unipolar depression which was not a consequence of another psychiatric disorder. The study also included participants who met diagnostic criteria for bi-polar II. The full inclusion criteria for the study sample for this thesis are described in chapter 3 and the study sample defined within the parameters of the concept of diagnosis is shown in table7 in chapter 4.
The authors position on the role of diagnosis in mental health care and treatment is usefully summarised by Craddock and Mynors-Wallace (2014) who advocate that diagnosis incorporate the following variables: lifetime course of the illness, suicidality, life time experience of symptoms classified within the diagnostic category, inter-episode functioning including cognitive functioning, co-morbid mental and physical health problems, co-morbid alcohol and substance misuse, life events associated with onset of episodes and full assessment of social and environmental factors both current and historical. All these factors taken together form a comprehensive psychobiosocial assessment and the information gathered is used to develop a formulation of problem maintenance and a treatment plan. This articulation of the definition of diagnosis is founded in the epistemological position articulated in chapter 3 of this thesis, the ‘primacy of praxis’.
What will follow is a definition of depression within the parameters of diagnosis as defined above, and in the context of the study participant sample recruited. The diagnostic criteria described here is restricted to MDD, Persistent Depression and Bi-polar II disorder. This definition of depression is informed by the two major diagnostic classification systems currently in use in both clinical practice and research, namely, DSM-5 (APA 2013) and ICD-10 (WHO 1994) the major features of which are summarised below. Given both diagnostic systems have considerable overlap both will not be described in detail here. Rather, the APA DSM-5 (APA 2013) diagnostic categories for depressive disorders are defined and the parallel definitions used in ICD-10 (WHO 1994) are cross referenced using the disorder coding indices from ICD-10 (i.e. F32.0 indicates MDD single episode, mild in ICD-10). When this PhD study was conducted the APA DSM-IV criteria (APA, 1994) were in use. The differences between the DSM-IV and DSM-5 criteria for depressive disorders are minimal. The changes incorporated into the DSM-5 are as follows: what is referred to as dysthymia in DSM-IV is now categorised as Persistent Depressive Disorder (PDD) in DSM-5 which also includes chronic depressive disorder and the previous dysthymic disorder (summarised from p 810–811 APA DSM-5 2013). The DSM-5 definition of PDD has been cited here as it best describes the population studied.
The DSM-5 diagnostic criteria for MDD and PDD (PDD) (APA 2013) are reproduced in tables 1 and 2, respectively. These categorisations are further defined within DSM-5 as follows. For MDD in terms of severity (mild, moderate, severe), with psychotic features, in partial remission, in full remission and unspecified and as a single episode or recurrent episode. In order to make a diagnosis terms are listed in the following order (p 161 APA DSM-5): MDD, single or recurrent episode, severity/psychotic/remission specifiers followed by any of the following further specifiers that apply in the current episode:
-
With anxious distress
-
With mixed features
-
With melancholic features
-
With atypical features
-
With mood-congruent psychotic features
-
With mood incongruent psychotic features
-
With catatonia
-
With peripartum onset
-
With seasonal pattern
For PDD there is a requirement to specify if the episode is in partial or full remission and whether onset is early (before age 21) or late (age 21 or older), alongside any of the further specifiers listed above under MDD. Further specifications for a diagnosis of PDD are (summarised from DSM-5 p 168):
-
With pure dysthymic syndrome: full criteria for MDD have not been met in at least preceding two years
-
With persistent major depressive episode: full criteria for major depressive episode have been met in at least the preceding 2 years
-
With intermittent major depressive episodes, with current episode: full criteria for a major depressive episode are currently met, but there have been periods of at least 8 weeks in at least preceding 2 years with symptoms below the threshold for a full major depressive episode
-
With intermittent major depressive episodes without current episode: full criteria for major depressive episode are not currently met, but there has been one or more major depressive episode in a least the preceding 2 years Specify if: mild, moderate or severe.
For Bi-polar II Disorder diagnosis there is a requirement to specify the current or most recent episode as hypomanic or depressed, alongside any of the further specifiers for the current episode listed above under the MDD criteria. If full criteria for a mood episode are not met, then it is necessary to indicate if this episode is in partial or full remission. If the full criteria for mood episode are met then the severity of the episode needs to be assigned (mild, moderate, severe) (summarised from APA DSM-5 criteria for Bi-Polar II Disorder pp 132–139).
The diagnostic criteria for Bi-polar II Disorder are shown in table 3 p 30).
As mirrored within the Craddock and Mynors-Wallace (2014) definition of diagnosis, the DSM5 classification also discusses diagnosis in a psychobiosocial context and identifies the following factors as being implicated in the vulnerability to and onset of MDD. Adverse childhood experiences and stressful life events are thought to play a role in increasing vulnerability to depression. In terms of temperament neuroticism is identified as a risk factor, particularly in the context of a stressful life event. Similarly, regarding genetic and physiological factors, first degree relatives of individuals experiencing a major depressive episode carry a risk factor two to four times greater than the general population, with hereditability accounting for 40% of this risk and within this the personality trait of neuroticism being the main genetic factor (summarised from APA DSM-5 2013 p 166). In comparison to individuals with MDD, those with PDD carry a higher risk for psychiatric comorbidity in general, particularly regarding anxiety disorders and substance use disorders. Early onset PDD is associated with DSM-IV cluster B and C personality disorder (summarised from APA DSM-5 p 171). In terms of Bi-Polar II Disorder risk and prognostic factors cited within DSM-5 (P 137) are: the risk of inheriting Bi-polar II Disorder is greatest among relatives of individuals with Bi-Polar II Disorder rather than those with Bi-Polar I Disorder. Bi-polar II
Disorder is associated with an increased incidence of co-occurring psychiatric disorders, the most common of which are anxiety disorders, with 75% of those diagnosed with Bi -Polar II Disorder having a co-morbid anxiety disorder (summarised from APA, DSM-5 diagnostic criteria for Bi-polar II Disorder, 2013, p 139).
TABLE 1: DSM-5 DIAGNOSTIC CRITERIA FOR MAJOR DEPRESSIVE DISORDER (APA 2013 P 160–161)
| Major Depressive Disorder (DSM diagnostic code 296. 296.20–296.36 ICD-10 equivalent F32) |
A: Five or more of the following symptoms present during the same 2-week period and represent a change from previous functioning. At least one of the symptoms is either depressed mood or loss of interest or pleasure (p 160)
Do not include symptoms clearly attributable to another medical condition (P 16–161)
1. Depressed mood most of the day, nearly every day indicated by subjective report (e.g. feels sad, empty, hopeless) or observation made by others (e.g. appears tearful)
2. Markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day (as indicated by either subjective account of observation)
3. Significant weight loss when not dieting or weight gain (e.g. a change of more than 5% body weight in a month) or decrease or increase in appetite nearly everyday
4. Insomnia or hypersomnia nearly everyday
5. Psychomotor agitation or retardation nearly every day (observable by others not merely subjective feelings of restlessness or being slowed down)
6. Fatigue or loss of energy nearly everyday
7. Feelings of worthlessness or excessive or inappropriate guilt (which may be delusional) nearly every day (not merely self-reproach or guilt about being sick)
8. Diminished ability to think or concentrate, or indecisiveness, nearly every day (either by subjective account or observation by others)
9. Recurrent thoughts of death (not just fear of dying) recurrent suicidal ideation without a specific plan, or a suicide attempt or a specific plan for committing suicide.
B: The symptoms cause clinically significant distress or impairment in social, occupational or other important areas of functioning
C: The episode is not attributable to the physiological effects of a substance or another medical condition Criteria A-C represent a major depressive episode
D: The occurrence of the major depressive disorder is not better explained by schizoaffective disorder, schizophrenia, schizophreniform disorder, delusional disorder or other specified and unspecified schizophrenia spectrum and other psychotic disorders |
E: There has never been a manic or hypomanic episode |
TABLE 2: DSM-5 DIAGNOSTIC CRITERIA FOR PERSISTENT DEPRESSIVE DISORDER (APA 2013 P 168–169)
|
Persistent Depressive Disorder (DSM -5 diagnostic code 300.3) (ICD-10 equivalent code
F34.1)
A. Depressed mood for most of the day, for more days than not, as indicated by either subjective account or observation by others, for at least 2 years
B. Presence, while depressed, or two (or more) of the following:
1. Poor appetite of overeating
2. Insomnia or hypersomnia
3. Low energy of fatigue
4. Low self-esteem
5. Poor concentration or difficulty making decisions
6. Feelings of hopelessness
C. During the two-year period of the disturbance the individual has never been without symptoms in criteria A and B for more than two months at a time
D. Criteria for major depressive disorder may be continuously present for two years
E. There has never been a manic episode or hypomanic episode and criteria have never been met for cyclothymic disorder
F. The disturbance is not better explained by a persistent schizoaffective disorder, schizophrenia, delusional disorder or other specified or unspecified schizophrenia spectrum and other psychotic disorder
G. The symptoms are not attributable to another medical condition (e.g. hypothyroidism)
H. The symptoms cause clinically significant distress or impairment in social, occupational or other important areas of functioning | TABLE 3: DSM-5 DIAGNOSTIC CRITERIA FOR BI-POLAR II DISORDER (APA 2013 P 132–139)
| Bi-polar II Disorder (DSM-5 diagnostic code 269.89 ICD-10 diagnostic code F31.81) |
For a diagnosis of Bi-polar II disorder must meet following criteria for a current or past hypomanic episode and the criteria for current or past major depressive episode (see table? For the criteria for major depressive episode):
Hypomanic episode: (p 132)
A. A distinct period of abnormally and persistently elevated, expansive or irritable mood and abnormally and persistently increased activity or energy lasting at least four consecutive days and present most of the day, nearly every day
B. During the period of mood disturbance and increased energy and activity three (or more) of the following symptoms have persisted (four if mood is only irritable), represent a noticeable change from usual behaviour, and have been present to a significant degree:
1. Inflated self-esteem or grandiosity
2. Decreased need for sleep (e.g. feels rested after only 3 hours of sleep)
3. More talkative than usual or pressure to keep talking
4. Flight of ideas or subjective experience that thoughts are racing
5. Distractibility (i.e. attention too easily drawn to unimportant or irrelevant external stimuli), as reported or observed
6. Increase in goal directed activity (either socially, at work or school, or sexually) or psychomotor agitation)
7. Excessive involvement in activities that have high potential for painful consequences (e.g. engaging in unrestrained spending sprees, sexual indiscretions or foolish business investments)
C. The episode is associated with an unequivocal change in functioning that is uncharacteristic of the individual when not symptomatic
D. The disturbance in mood and the change in functioning are observable by others
E. The episode is not severe enough to caused marked impairment in social or occupational functioning or to necessitate hospitalisation, If there are psychotic features the episode is by definition manic
F. The episode is not attributable to the physiological effects of a substance (e.g. a drug of abuse, a medication or another treatment)
To meet a diagnosis of Bi-polar II disorder:
A. Criteria have been met for at least one hypomanic episode (criteria A-F under hypomanic episode above) and at least one major depressive episode (criteria A-C under major depressive episode above)
B. There has never been a manic episode
C. The occurrence of the hypomanic episode(s) and major depressive episode(s) is not better explained by a persistent schizoaffective disorder, schizophrenia, delusional disorder or other specified or unspecified schizophrenia spectrum and other psychotic disorder |
D. | The symptoms of depression or the unpredictability caused by frequent alteration between periods of depression and hypomania causes clinically significant distress or impairment in social, occupational or other important areas of functioning |
Defining and treating persistent, treatment resistant depression
The NICE Guidance for the treatment of depression (NICE CG90 2009), utilising the evidence base cited above (Cuijpers, Berking, Andersson, Quigley et al 2013) recommends a combined treatment of CBT plus antidepressant medication for moderate to severe depression, with a variety of pharmacological and psychological augmentations recommended for more severe and complex clinical presentations. Similarly, the British Association of Pharmacology (BAP) publish recently updated guidelines covering evidence-based pharmacotherapy for treating depressive disorders (Cleare, Pariante, Young, Anderson, Christmas, Cowen, Dickens, Ferrier, Geddes, Gilbody, Haddad, Katona, Lewis, Malizia, McAllister-Williams, Ramchandani, Scott, Taylor and Uher, 2015).
The focus of this PhD thesis is persistent, treatment resistant depressive disorder. There is much debate in psychiatry regarding how to define and categorise treatment resistant depression given the heterogeneous nature of depression in terms of its clinical manifestations. According to Murphy, Sarris and Byrne (2017) the term ‘treatment resistant depression’ first appeared in the scientific literature in the 1970’s and has replaced the previously used term, ‘treatment refractory depression’. Conway, George and Sackheim (2017) observe that definitions vary widely and are prone to being vague. The prevalence of treatment resistant depression is hard to estimate because there is a lack of consensus regarding its definition (Nemeroff, 2007). Murphy, Sarris and Byrne (2017) make an important observation regarding prevalence rates when they describe what they refer to as ‘pseudoresistance’ (p 2). This is defined as treatment resistance resulting from diagnostic and/or treatment factors which, when adequately addressed, may lead to symptom remission and improved patient outcomes. According to the authors factors that contribute to this phenomenon include misdiagnosis, individual clinician differences, co-morbidity, inadequate treatment and patient heterogeneity. Data from the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) clinical trial, which to date is the most comprehensive study of treatment resistant depression, found that in 30% of individuals diagnosed with MDD the illness fails to make a response to treatment with both antidepressant medication and psychotherapy (Rush, Madhukar, Trivedi, Wisniewski, Nierenberg, Stewart, Warden, Niederehe, Thase, Lavori, Lebowitz, McGrath, Rosenbaum, Sackeim, Kupfer, Luther and Fava, 2006)
Murphy, Sarris and Byrne (2017) identify two important findings from the STAR*D trial. Firstly, for most participants, the treatments offered in the study were less efficacious than anticipated and therefore required sequential treatments following a non-response to the initial treatments. Further, participants with chronic or recurrent episodes of depression overall had poorer outcomes and required a greater number of treatment interventions to maximise response (Gaynes, Warden, Trivedi, Wisniewski, Fava and Rush (2009). Using the STAR*D data set as a starting point, researchers and clinicians have begun to develop a more operationalised approach to defining treatment resistant depressive disorder, which takes into consideration the individual’s response to a range of psychobiosocial interventions and which can be inform both research and clinical practice.
The research literature proposes a range of models for defining treatment resistant depression Murphy, Sarris and Byrne (2017) describe the evolution of these definitions (1997 – 2010), presenting a range of models proposing definitions of treatment resistant depression. Each iteration has according to Nemeroff (2007) been operationalised by the integration of empirical criteria and specific definitions of treatment response and remission included. Murphy, Sarris and Byrne (2017) also offer a comprehensive account of what they consider to be the biological, psychological, genetic and clinical correlates of treatment resistant depression. These are reproduced in appendix II. More recently McAllister-Williams and colleagues propose a definition of persistent, treatment resistant depression which they term Multiple-Therapy-Resistant Major Depressive Disorder (McAllister-Williams, Christmas, Cleare, Currie, Gledhill, Insole, Malzia, McGeever, Morriss, Robinson, Scott, Stokes, Talbot and Young 2018). This is reproduced in appendix III. This will be discussed in more detail here as, not only are the criteria derived from and devised for the UK NHS service delivery model, but they are clinically significant in that they represent current best evidence based practice principles for the treatment and management of persistent, treatment resistant depression. In this regard they resonate with the philosophical pragmatism position of this thesis (see chapter 3 for a full discussion of this concept). In addition, the criteria acknowledge the importance, where indicated, of using pharmacological and psychological interventions in tandem, a model for which there is not only an evidence base (Morriss, Garland, Nixon and Guo et al 2016), but which also presents a more holistic treatment rationale, which is of greater clinical utility in NHS practice. All too often psychological and pharmacological interventions are pitted against each other both in clinical and research arenas and this dichotomous rivalry can operate to the detriment of those most in need of clinical care and treatment.
The proposed criteria not only accommodate the standard evidence based psychological and pharmacological interventions currently widely available in the NHS (NICE Guidance, CG90, 2009), but recognise the potential clinical benefits of what are referred to as non-standard treatments. The authors report data from naturalistic studies indicating people with treatment resistant depression show a response rate of 10% over one year to standard treatments. Non-standard treatments are defined as interventions that may be of benefit to those suffering with persistent, treatment resistant depression, but which are not currently included in treatment guidelines (i.e. NICE Guidance CG90, 2009) or are only recommended for use in specialist services. Typically, such interventions have a less robust evidence base supporting their efficacy, they may carry greater risks in terms of use, be more invasive or more costly relative to other treatments. Examples of such treatments cited by Conway, George and Sackheim (2017) include: repetitive Transcranial Magnetic Stimulation (r-TMS), intravenous/intranasal ketamine, inhaled nitrous oxide, vagus nerve stimulation, deep brain stimulation and buprenorphine (p 9).
CBT Treatments for Depression
In mirroring this concept of non-standard treatments and CBT interventions for persistent treatment resistant depression, in the field of CBT research there continues an ongoing quest to develop more focused interventions for depression beyond the original Beckian protocol (Beck, Rush, Shaw and Emery 1979). These aim to either target the cognitive phenomena researched and described previously in this chapter (i.e. Rescripting of Depressive Intrusive
Memories (Brewin, Wheatley, Patel, Fearon, Hackman, Wells and Myers, (2009)); Mindfulness Based Cognitive Therapy (MBCT) (Ma and Teasdale (2004)); Rumination Focused Cognitive Therapy, (Watkins, Mullan, Wingrove, Rimes, Steiner, Bathurst, Estman, and Scott (2007)) and Attentional Control Training, (Papageorgiou and Wells (2000)) or to take a behavioural approach (Acceptance and Commitment Therapy, (ACT) Hayes, Luoma, Bond, Masuda and Lillis, (2006); Behavioural Activation (BA) Dimidjian, Hollon, Dobson, Schmaling, Kohlenberg,
Addis, Gallop, McGlinchey, Markley, Gollan, Atkins, Dunner and Jacobson, (2006) and Compassion Focused Therapy (CFT), Gilbert and Procter 2006). One exception to this cognitive or behavioural orientation is Cognitive Behavioural Analysis System (CBASP) (McCullough, 2000) which whilst utilising core CBT principles in terms of therapy structure it is largely interpersonal in focus in terms of its interventions, although draws on behavioural theory to account for some maintenance factors (Furukawa, Schramm, Weitz, Salanti, Efthimiou, Michalak, Watanabe, Cipriani, Keller, Kocsis, Klein, and Cuijpers, (2016).
The way forward in persistent, treatment resistant depression
The field of cognitive and behavioural psychotherapies is, to some extent embroiled in the same rivalries as psychological versus pharmacological treatments for depression. Equally, they fall foul of the same debates that are outlined earlier in this chapter regarding the definition of CBT. For example, the Behavioural Activation for depression protocol contains no intervention that would not be found in the cognitive therapy for depression protocol. When the author of this thesis debated this with Steve Hollon (Hollon, 2014) he stated that formal thought challenging as is found in the Beckian protocol is not part of the BA protocol. However, he did concede the BA protocol includes testing out negative predictions which, in second generation cognitive therapy is a core intervention defined as cognitive (BennettLevy, Butler, Fennell, Hackman, Mueller, and Westbrook, 2004).
In the clinical experience of the author of this thesis, whilst these interventions described above (both pharmacological and psychological) have merit in terms of their clinical utility, as the STAR*D (Rush, Madhukar, Trivedi, Wisniewski et al 2006) clinical trial observed no treatment for MDD (either psychological or pharmacological either standard or nonstandard) is, on its own, a panacea. Therefore, the STAR*D authors advocate sequential treatment steps in order to achieve symptom remission. It is the authors view that with regard to persistent, treatment resistant depression that an integrated, sequentially delivered psychobiosocial intervention is, currently, the most effective means by which to achieve symptom remission, to manage persistent symptoms, to improve occupational and social functioning and improve quality of life and this needs to be the future direction of treatment and care for persistent treatment resistant depression (Morriss, Garland, Nixon and Guo et al (2016).
Returning to Salkovskis (2002) and the concept of empirically grounded clinical interventions, more attention needs to be placed on targeting interventions according to clinical presentation and patient choice and acceptability of interventions (Curley, Smout and Denson 2019). In this regard, the author of this thesis would argue, given the heterogeneity of clinical presentations in depression, there is an argument for developing CBT treatment protocols that target specific psychological constructs that from the authors own clinical observation are central in persistent treatment resistant depression. One such construct is subjugation (Young 1990). It is the limitations of a using a standard Beckian approach alone when working with subjugation in this form of depression that led to the authors interest in CFT (CFT Gilbert and Choden, 2013). For the last eight years the author has been piloting the delivery of a group-based intervention for persistent, treatment resistant depression which draws on the cognitive science of depression literature and integrates standard Beckian clinical interventions for depression with Gilbert’s CFT (i.e. Gilbert and Irons, 2005. This thesis is one step in this journey of discovery.
Chapter 2 Literature Review
[[Introduction ]]
Following the introduction, this chapter will begin with a description of Brawley’s (1993) decision making process for defining the utility of a theoretical model. The decision was taken to include this process given the complex range of models reviewed in this chapter. This will be followed by a review of the literature defining each of the constructs under study in this thesis, shame, self-criticism and self-compassion. The purpose being to consider the role of these constructs in persistent, treatment resistant depression. These constructs will be reviewed in the context of Paul Gilbert’s theory which, using an evolutionary psychology foundation, posits the centrality of shame and self-criticism and self-compassion in emotional disorders (Gilbert, 2017a; 2017b; 2016; 2007a; 2005a; 2005b; 1998; 1995; 1992; 1989). Gilbert has developed a clinical model CFT (Gilbert and Procter 2006), which he states is not a model of psychotherapy but a biopsychosocial approach utilising a set of clinical interventions grounded in an evidence-based treatment rationale. It is drawn from evolutionary psychology (Gilbert 2017a; 2007a; 2001) and, Gilbert attests, can be integrated into any psychotherapy model. The specific aim of CFT is to target shame and self-criticism (which are viewed as being implicated in the persistence of emotional disorders) by the process of generating self-compassion.
One of the challenges of defining these constructs is the task of differentiating between them, whilst also considering their interplay in the context of the individuals subjective experience of depression. Concurring with Kaufman, (1974) the author of this thesis would observe from clinical experience, that shame in the context of persistent, treatment resistant depression is often the most difficult emotion for sufferers to describe, experience and tolerate. Again, drawing on clinical observation (Garland, 2016), self-criticism as a facet of the depressive experience is ubiquitous, with the corollary that most sufferers would question the idea of self-compassion. Rather, at best, for people suffering with persistent, treatment resistant depression, self-compassion is considered self-indulgent and frequently the very idea of selfcompassion is shame inducing in and of itself. Further, where self-criticism is especially pernicious, the dominant perception is that what is needed rather than the sustenance of self-compassion, is punishment, as compassion is undeserved because sense of self is experiences as one so inherently bad, flawed and worthless (Moore and Garland, 2003).
Universally people who experience persistent depression may describe being troubled by a range of emotions including sadness, anxiety, anger, guilt and shame. However, whether some emotions have more salience than others in the experience of depression and the interrelationship between these different emotional states as part of a clinical presentation are not well articulated in the both the research and clinical literature. Kim, Thibodeau and Jorgensen (2011) observe that in the discipline of psychiatry insufficient attention has been paid to delineating the range of emotions reported by depressed patients and call for more detailed analysis of the specific emotions experienced. The authors go on to note that there is a lack of research examining the conditions under which shame is linked to depressive symptoms, which they observe is not the case in other emotional disorders such as eating disorders, Post Traumatic Stress Disorder (PTSD) and Body image disturbance.
The Practicality of theories: Defining a decision-making process
As outlined in chapter one of this thesis the author would describe herself as a Scientist
Practitioner. In the field of psychology there is a long tradition of adopting the Scientist – Practitioner approach (Salkovskis, 2002) in order to develop clinical interventions to tackle health related problems. Central to this model is the reciprocal relationship between theory and clinical practice. Thus, in order to develop and implement clinical interventions that aim to ameliorate health related problems the clinician must use theory to guide clinical practice and in turn use the successes and failures of clinical interventions to modify the theory or the use of that theory. Brawley (1993) argues that the utility of any theory lies in its capacity to be used to understand clinical presentations and in turn develop effective clinical interventions. However, as Brawley observes a complicating factor in the process of making decisions about how to intervene clinically is the fact that there is usually more than one theory to take into consideration. In order to address this Brawley suggests a decision-making process for identifying which theory it is reasonable to use as a basis for advancing our theoretical understanding and informing clinical practice. Brawley argues that how we decide which theories we choose to underpin our clinical practice should be guided by the principle of ‘the practicality of employing psychological theories’ (p 100). Here Practicality is used as defined in the philosophical tradition of Pragmatism (Biesta, 2010; Hookway 2006), which is the epistemological position taken in this thesis and which is discussed more fully in chapter three.
Brawley (1993) proposes a set of criteria for measuring the Practicality of a theory in order to determine its utility as a theory in informing clinical practice. Thus, the Practicality of a theory can be defined by the number of stable traits associated with the theory. Brawley identifies six such characteristics as follows:
1. Focuses on processes susceptible to social change
2. Adequately describes the relationship between key sets of variables so they can be targets for change
3. Has an associated set of assessment of the theoretical variables
4. Has a substantive research base (basic and applied) that indicates the theory is valid?
5. Offers concepts that can be translated into operational manipulations thought to affect behavioural/cognitive change
6. Based on having the above characteristics, has a basis for detecting why (i.e. conceptual measurement, manipulation level) an intervention failed to produce change
A basic principle in science is to compare theories, the most common approach being to compare theory A against Theory B. This is often seen as a useful endeavour if two theories claim to explain the same phenomenon and the variables articulated within each theory are entirely different from each other. The purpose of this being to discard theories that are less accurate in terms of understanding a phenomenon. However, as Brawley (1993) asks the reader to consider, the fact that in the process of comparing theory A and Theory B the purpose is not only to identify the differences, strengths and weaknesses of each theory but also to identify similarities and commonalities between the theories under comparison. Based on this premise Brawley (1993 p 101) argues that rather than compare one theory against another it is legitimate to consider a merging of theories if these theories have:
-
complimentary or overlapping factors
-
are related to a majority of socially learned variables that can be used as a target for change
-
are related to aspects of self-regulation on a continuum of volitional and nonvolitional behaviour
Taking this approach according to Brawley militates against the fragmentation of knowledge which in turn has potential to limit its application. Therefore, in order to develop theories three criteria need to be considered (p 102):
1. Model testing which deals with matching tests to model content, proper manipulations, presence of interactions and tests of multiplicative variables
2. Concept differentiation which considers variable similarities and differences
3. Distinctions between static and dynamic models
In examining the range theoretical models of shame, self-criticism and self-compassion the criteria and process advocated by Brawley will be used to examine the similarities and differences between these theoretical models. Where clinical interventions related to each theory have been developed these will also be discussed.
This literature review will first review theories of shame, self-criticism and self-compassion.
These will then be critiqued using the Brawley (1993) criteria as a foundation.
The conundrum of defining Shame as an affect
Theories regarding the nature, origins and definition of shame are diverse and this diversity has been vigorously debated across a range of academic disciplines for over a century. These disciplines include anthropology, psychiatry, sociology, social-personality psychology (specifically theories of self and theories of emotion), psychotherapy (both psychoanalytic and cognitive) and genetics.
Kaufman (1974) observed that our language lacks the vocabulary to adequately capture the experience of shame and reflects:
‘Various clinicians, theorists and writers have hold of some aspect or other of shame, but few have been able to apprehend it fully’
(Kaufman, 1974, p 568).
Gilbert (1998) observes that a range of shame theories exist which draw from two key theoretical positions psychoanalysis and Kohutian self-psychology. Gilbert continues by describing how shame theories can be theoretically conceptualised as follows, summarised from (Gilbert 1998, p 3):
-
Affect (e.g. Kaufman 1989; Nathanson 1987; Tomkin 1963)
-
Cognitive-affective (e.g. Lewis 1992; Tangney and Dearing 2002)
-
Cognitive-behavioural (e.g. Beck, Emery and Greenberg 1985; Klass 1990)
Further, according to Gilbert (1998) these different theoretical models place different emphasis on the components and mechanism of shame. Thus, as summarised from (Gilbert, 1998 p 4) shame can be viewed:
-
As a primary emotion in its own right
-
As a composite of other emotions such as fear, anger or self-disgust
-
As cognitions and beliefs about the self (e.g. see self/others see self as inferior/ weak /flawed)
-
As behaviours and actions (e.g. running away, concealing, hiding or attacking)
-
As evolved mechanisms (e.g. the expression of shame in humans seems to use the same biobehavioural system as animals in the animal kingdom expressing submissive behaviour)
-
As interpersonal dynamic interrelationships (e.g. shamed and ‘shamer’)
Tangney, Wagner and Gramzow (1992) observe that the most comprehensive account of shame and guilt and psychopathology exists in the psychoanalytic literature. They note that Freud himself focused largely on the role of guilt and he posited that guilt emerged from impulses deemed forbidden, which gave rise to self-punishment, manifest in the form of obsessional neurosis, masochism and depression. In contrast Freud did not develop a comprehensive hypothesis regarding the origins of shame beyond labelling it as a reaction formation against sexually exhibitionist impulses (see Tangney, Wagner, Fletcher and Gramzow 1992 p 469).
Early definitions of shame emerged from the psychoanalytic psychotherapy tradition and are based on clinical observation and articulated as an existential commentary on the experience of shame. Below is a definition from Tomkin (1963):
‘If distress is the affect of suffering, shame is the affect of indignity, of defeat, of transgression and alienation. Though terror speaks to life and death and distress makes the world a vale of tears, yet shame strikes deepest into the heart of man. While terror and
distress hurt, they are wounds inflicted from outside which penetrate the smooth surface of the ego; but shame is felt as an inner torment, a sickness of the soul. It does not matter
whether the humiliated one has been shamed by laughter or whether he mocks himself. In either event he feels himself naked, defeated, alienated, lacking in dignity or worth’
(Tomkin, 1963, p 118).
The 1970’s saw the emergence of self-psychology in psychoanalysis and with this came formulations of shame as being central in a range of psychiatric diagnoses including depression, bi-polar disorder, schizophrenia and narcissism. Tangney, Wagner and Gramzow (1992 p 469) cite Kohut, (1971), Morrison, (1987) and Nathanson, (1987) as examples of these formulations. The same authors also note the important contribution H.B. Lewis (1971) made to the theoretical research literature by presenting an integrated account of the different roles shame and guilt may play in psychopathology. This distinction is described more fully in the definition of self-criticism section of this chapter. In brief, H.B. Lewis argued that shame is more closely aligned to the experience of depression and guilt to paranoia and obsessivecompulsive syndromes. Tangney, Wagner, Fletcher and Gramzow (1992) describe H.B. Lewis’ theory as an integration of psychodynamic and cognitive principles in which individual differences in cognitive style gives rise to distinct modes of superego functioning which in turn give rise to different symptom profiles. H. B. Lewis terms these ‘field dependence’ versus ‘field independence’ (Tangney, Wagner, Fletcher and Gramzow (1992 p 470). Field dependence represents a less differentiated sense of self which is more vulnerable to the global experience of shame and therefore to depression. This is contrasted with field independence where there is a better differentiated sense of self which creates a vulnerability for experiencing guilt (where a distinction is made between self and behaviour) which gives rise to obsessional and paranoid symptomology.
The work of Tangney focuses on shame and guilt in the interpersonal and intrapersonal realm (Tangney and Dearing 2002; Tangney, 1991) and she cites her body of research as evidencing the distinction between behavioural and characterological self-blame identified by H.B. Lewis (Tangney and Dearing, 2002). Thus, for Tangney (Tangney, 1991) when an individual experiences a shame reaction there is not a clear distinction made between self and behaviour (characterological self-blame) and between self and other. Thus, she argues shame proneness is associated with a reduced capacity to empathise for the position of the other and an increased likelihood of a self-focused personal distress response. She posits that the shame prone individual may experience difficulty responding effectively in situations of interpersonal conflict where the person may feel responsible for the distress of the other and that this may be such an intensely painful emotional experience that a process of externalisation of blame occurs in which the shamed individual responds with anger and hostility to the other person. This phenomenon is discussed further below in the self-criticism and self-blame section.
Traditionally in psychiatry shame is formulated as a biological symptom of depression and as such its intensity and duration is considered to be mediated by the severity of depressed mood. Therefore, as the severity of depression decreases and mood improves, levels of shame reduce. Many contemporary theorists and researchers (e.g. Kim, Thibodeau and Jorgensen 2011; Tangney and Dearing 2002) observe that work in emotion research has failed to adequately differentiate between the range of emotional states associated with depression. A relatively newly emerging field in the study of emotions is that of self-conscious emotions (Tracy and Robins, 2007a). This work proposes a distinction be made between what is referred to in the literature as basic emotions and self-conscious emotions and from this cognitive-affective models of shame have emerged.
Cognitive-affective models of shame
There is a consensus in the field of emotion research that a distinction can be drawn between basic emotions and self-conscious emotions. Tracy and Robins (2007a; 2006; 2004) define basic emotions as falling into a small category of emotions which are biologically based (that is prewired and genetically derived), shared with other animals, occur across cultures and can be identified by universally recognisable facial expressions and or bodily postures. These basic emotions are anger, fear, disgust, sadness, happiness and surprise. The authors go on to contrast these basic emotions with what are defined as self-conscious emotions which differ in that; they rely on verbal report in order to be identified and described; they are culturally specific in that their triggers, their subjective experience and consequences vary across societies and social groups and only in very recent years have universally recognisable non-verbal expressions for some self-conscious emotions been identified across cultures. The self-conscious emotions are shame, guilt, embarrassment and pride.
From an evolutionary psychology perspective self-conscious emotion are said to be ‘prosocial’, that is they serve the function of engendering adaptive social behaviours. In particular, what is referred to in the literature as ‘self-blaming moral emotions’ (shame and guilt) are considered important in terms of the development and maintenance of interpersonal relationships, as they provide a mechanism for social regulation by facilitating a balance between the individuals own innate drives and the rights and needs of others (Bastin, Harrison, Davey, Moll and Whittle 2016).
Tracy and Robins (2007a) also observe that self-conscious emotions are often subsumed by basic emotions in what they refer to as a linguistic hierarchy such that, for example, sadness is seen to subsume shame and joy subsumes pride. The wok of Tracy and Robins (2006; 2004) draws on earlier work by Lewis (2007; 2000) and he also refers to this tendency to subsume self-conscious emotions in basic emotions. He argues that self-conscious emotions are not a by-product of basic emotions which deserve lower status than the cognitive-attributional processes with which they are associated. He contests a reciprocal relationship between cognition and emotion in which emotions give rise to cognitions and cognitions give rise to emotions and in this respect self-conscious emotions warrant an equal footing with basic emotions.
Tracy and Robins (2007a; 2006; 2004) describe five features of self-conscious emotions which distinguish them from basic emotions and which they argue must be accounted for in any comprehensive model of self-conscious emotions. These features are as follows:
1. Self-conscious emotions require self-awareness and self-representations. In this context sense of self is formulated as consisting of two facets; an on-going sense of self-awareness (the ‘I’ self) and the capacity for complex self-representations (the ‘me’ sense). In the latter, what is being referred to is the mental representations individuals make of themselves that constitute their identity. It is via these processes that an individual makes self-evaluations and in turn experience self-conscious emotions. These self-representations are not confined to the cognitive content of self but the individual’s relational, social and collective self-representations. This last point resonates with an evolutionary perspective (Gilbert 2007a) in observing that humans are biologically wired to be social and thus our self-representations reflect how we see ourselves in relation to close others (e.g. as a romantic partner), social groups (e.g. as a friend) and broader cultural groups (e.g. as a woman).
2. Self-conscious emotions emerge later in childhood than basic emotions. Research (Lewis 2007) suggests that most basic emotions emerge within the first 9 months of life. The first signs of self-conscious emotions in the form of embarrassment emerge between the ages of 18–24 months. Meanwhile more complex emotions such as shame, guilt and pride do not emerge until a child reaches age three years. Thus, it is argued, unlike basic emotions which are biologically derived and present from birth because they are necessary for survival, self-conscious emotions are cognition derived and thus they only emerge when the child begin to develop the cognitive capacity to generate such emotions.
3. Self-conscious emotions facilitate the attainment of complex social goals. A fundamental assumption of all theories of emotion is that both basic and selfconscious emotions have evolved through a process of natural selection to promote survival goals (i.e. staying alive and reproducing). This seems common sense when considering emotions such as fear for example i.e. feeling fear when encountering a predator. Self-conscious emotions are believed to have evolved to promote what
Tracy and Robins (2007a; 2006; 2004) define as certain social goals such as the maintenance or enhancement of status or prevention of group rejection. The authors give a rationale for this based on the idea that from an evolutionary perspective in order to survive human beings have to negotiate numerous complex social interactions, for example co-operating in groups, detecting and managing cheating and dealing with intergroup and intragroup rivalries. The necessity of these complex interactions may have led to the development of a specific set of emotions which serve the social goal of promoting behaviours that increase the stability of social hierarchies and affirm social status roles.
In considering shame and embarrassment these emotions may promote appeasement and avoidance behaviours when a social transgression has occurred. Meanwhile guilt may promote apology and making amends after a social transgression and pride promote approach behaviours after an individual succeeds in a domain where this type of success carries social value. These social goals also serve the purpose of facilitating survival and reproduction.
4. Self-conscious emotions do not have discrete, universally recognised facial expressions. Each of the six basic emotions (anger, fear, disgust, sadness, happiness and surprise) have discrete, universally recognised facial expressions. However, this is not the case for self-conscious emotions. Goetz and Keltner (2007) state that whilst there is compelling evidence for universal facial and postural displays of embarrassment, the results for displays of shame are less clear cut and to date no reliable facial display for guilt has been found. Tracy and Robins (2007a) account for this absence of facial expressions by arguing that self-conscious emotions are more frequently conveyed through language and this is because the messages which need to be conveyed by selfconscious emotions are so complex that facial expressions are inadequate for conveying the necessary and intended meaning. The authors also observe that there may be some instances in which expressing self-conscious emotions are unhelpful or maladaptive and therefore from an evolutionary perspective it is advantageous to be able to regulate or hide these. The example the authors cite is pride in that, in some cultures, it is unacceptable to show pride and to do so may reduce likeability (Tracy and Robins, 2007b).
5. Self-conscious emotions are cognitively complex. Whilst a basic emotion such as fear requires only the ability to appraise an event as a threat to survival goals, selfconscious emotions require direct attentional focus on self the person, to develop stable selfrepresentations and to consciously reflect on these. The capacity to do this necessitates a complex range of interlinked self-evaluative processes that elicit selfconscious emotions. Whilst basic emotions can involve such appraisals these appraisals are simpler.
Cognitive-Attributional theories of shame
Tracy and Robins (2007a) argue that self-conscious emotions should be treated as a special class of emotions which they define as ‘cognition-dependent’ emotions. They go on to argue that self-conscious emotions require a distinct theoretical model which articulates the antecedent cognitions that make them distinct from basic emotions and propose an
‘appraisal-based process model of self-conscious emotions’ (Tracy and Robins 2007a; 2006; 2004). A precursor to Tracy and Robins’ model, and one on which they draw to develop their own, is that of Lewis (2000). This model is outlined below.
Lewis’ attributional theory of self-conscious emotions
Lewis (2000) observes that whilst basic emotions such as happiness can be elicited by say the sight of a loved one, self-conscious emotions rather than being triggered by a specific event are likely to require classes of events that can only be readily articulated by the person experiencing the emotion. Thus, Lewis goes on to argue what is required as a precursor to the triggering of self-conscious emotions is an elaborate cognitive process in which selfconstructs play a key role. Therefore, rather than, as in basic emotions, where there are universal trigger (e.g. fear at the approach of a stranger) in the self-conscious emotions it is what we think, and the way we think it, that are the triggers of our self-conscious emotions.
In his cognitive-attributional theory of self-conscious emotions Lewis describes three interconnected cognitive-evaluative processes involved in the elicitation of such emotions.
Each of these is described below.
Standards, Rules and Goals (SRG’s)
The first cognitive-evaluative process identified by Lewis is what he terms Standards, Rules or Goals (SRG’s), which govern our behaviour. These are defined as a personal and idiosyncratic set of beliefs about what is acceptable for self and others as standards for action, thoughts and feelings. These are derived from and prescribed by the environment and culture in which a child is raised, e.g. class, family, gender, religion, political allegiances and the like. The acquisition of these SRG’s is predicated on the child’s learning of and willingness to accept these SRG’s as their own. Lewis posits that the adoption of these SRG’s begins early in development and cites his own research as indicating that by age one a child is beginning to learn the expected action patterns enshrined within SRG’s of their environment and culture and by age two children have some understanding of what their culture and environment deems appropriate or inappropriate behaviour. However, he does concede that SRG’s will develop and adapted throughout a person’s life. Lewis does not define success or failure in his theory, nor does he make suggestions as to the parameters of SRG’S. Rather his theory assumes self-evaluations are internal events residing in a person, whilst SRG’s are taught by others.
Internal versus external evaluations
The second cognitive-evaluative process in Lewis’s theory is that of evaluation of SRG’s in terms of the persons’ own actions, thoughts and feelings. That is, SRG’s become a measure of self-evaluation by which the individual assesses their actions. Lewis posits that this capacity for self-evaluation has two distinct possible outcomes in relation to a person’s actions, namely we can hold ourselves responsible or not responsible. Put in the language of attributional theory the individual can make an internal or external evaluation. Thus, if a person holds themselves not responsible, they stop evaluating themselves as responsible. However, if a person does hold that they are responsible then SRG’s are used as the measure by which the person judges their behaviour as successful or unsuccessful. This measure of success or failure is located in the person themselves depending on their own idiosyncratic SRG’s. For example, if a person has an SRG that getting an A in an exam is the standard to be met and they get a B then this will be viewed by the person as a failure. If, however the standard is to pass the exam then a B will be viewed as a success. In the arena of self-conscious emotions, it is internal attributions that hold significance. Once more Lewis cites his own research to support this view, stating that once a child reaches age three there is evidence that they already have SRG’s and further that they appear to show distress when these are not met. However, people often break their SRG’s but do not always attribute failure to do so to themselves. So, if a person breaks an SRG they may account for this by calling on chance or focusing on the actions of others (an external evaluation). A further consideration for Lewis in the self-evaluation process is the environment and the way in which a person learns their SRG’s. Lewis concedes that once an internal evaluation has been made and responsibility assigned to self, there exists a lack of understanding as to how an individual judges an action, thought or feeling as a success or failure. He puts forward several factors as possibly influencing how a person evaluates an action, thought or feeling as a success or failure. These are an early failure in the self-system leading to the emergence of narcissistic disorders, harsh socialisation experiences and high levels of reward for success or punishment for failure (Lewis 2000 p 626). Finally, Lewis observes that the degree to which a person evaluates an action, thought or feeling as a success or failure will significantly influence future planning and goal aspiration.
Attributions about self: Global versus Specific
The third cognitive-evaluative process identified by Lewis is global versus specific attributions about self. These are defined in line with attributional theory whereby in a global attribution the person’s evaluation of self focuses on the whole self both in terms of subject and object. Meanwhile in a specific attribution self-evaluation is limited to specific actions and behaviours of the person rather than an evaluation of self in its entirety. Lewis next elaborates a further cognitive process related to self-evaluations that of specific attributions where this refers to a specific aspect of or action related to self and global attributions which refer to the whole self.
Lewis expresses his theory in diagrammatic form (see Figure 2) and within this articulates the implications of his theory for the elicitation of self-conscious emotions. His theory focuses on four self-conscious emotions shame, guilt, pride and hubris where the elicitors of the emotions are cognitive in nature. Lewis warns against the misunderstanding and misuse of the term pride and makes a distinction between two forms of pride, namely pride in the traditional sense of the word, taking pride in one’s achievements in relation to a specific goal or activity. This is contrasted with pride that can be indicative of a negative emotional state for which Lewis uses the term hubris. He defines hubris as global pride and relates it to narcissistic characteristics in which the person is ‘puffed up’ with ‘false pride’ (p 628).
FIGURE 2: LEWIS’S COGNITIVE- ATTRIBUTIONAL THEORY OF SELF-CONSCIOUS EMOTIONS (LEWIS 2000 P 628)
3 sets of activities:
1. Establishment of SRG’s
2. Evaluation of one’s success or failure of SRG’s
3. Attribution of self
| SUCCESS | FAILURE | |
| HUBRIS | SHAME | |
| PRIDE | GUILT/REGRET | GLOBAL |
SPECIFIC
The four self-conscious emotions and their concomitant cognitive elicitors are as follows (Lewis 2000 p 628):
Shame: is elicited as a result of a failure evaluation in relation to an SRG’s when the person makes a global evaluation of self
Guilt: is elicited as a result of a failure evaluation relative to the SRG’s when the person makes a specific evaluation of self
Hubris: is elicited as a result of a success evaluation relative to the SRG when the person makes a global evaluation of self
Pride: is elicited as a result of a success evaluation relative to the SRG when the person makes a specific evaluation of self.
For the purpose of defining shame the majority of the discussion of Lewis’s model will be restricted to a focus on his definition of shame. However, as historically definitions of shame and guilt have often been conflated, which researchers observe has hampered the understanding of self-conscious emotions (see Tangney and Dearing 2002 for a discussion) time will be given here to describing how Lewis draws a distinction between shame and guilt.
In addition, some literature links shame and embarrassment (Izard 1977; Tomkins 1963) and Lewis draws out a distinction between these in his model, therefore a brief discussion of these emotions and their differences as elucidated by Lewis will be included.
For Lewis, shame is a complex set of cognitive activities in which the individual evaluates their actions in the light of their SRG’s and a global evaluation of self, the whole self is deemed a failure. Thus, shame is elicited not by a situation in itself but by the person’s interpretation of the meaning of that situation. Importantly here the events which elicit a shame response can be either public or private and can involve moral actions. He observes that shame is a highly aversive emotional experience in which the individual, consumed by a perception that they are under the intense scrutiny of others, experiences a strong desire to hide, disappear or die. He goes on to describe how shame when elicited interrupts current behaviour and is accompanied by a shrinking of the body (to make the self smaller and be less visible), disruption to thought processes and an inability to speak. As the elicitation of shame involves a global attack on self, this Lewis argues makes it an emotion that it is hard to salve and as a consequence it is associated with a range of coping strategies including dissociation and repression.
By contrast Lewis holds that guilt arises when an individual evaluates their behaviour as a failure where the focus is on a specific behaviour or action by the self. Consequently, the individual orientates their behavioural intentions towards actions aimed at the correcting or repairing of damage done, they may or may not carry out these actions, but the intention is towards making amends. In this regard Lewis sees guilt as opening up the opportunity for restoration via a process of rectifying the current wrongdoing and giving an undertaking to strive for future prevention of the same wrong doing. As result he argues that the emotional experience of guilt is not as intense and excruciating as shame and the concomitant interruption to thought and behaviour that occurs when shame is elicited is not present when guilt is elicited. The main behaviour observed in guilt is the individual physically moving in a way that demonstrates their intention to try and repair damage done.
Therefore, because guilt is associated with specific action then feelings of guilt can be salved by the taking of reparative action. Thus, in guilt, self is differentiated from action or behaviour and therefore the emotional experience is less intense and dissipates more readily, because there is not, as in shame, a global attack on self. However, for Lewis, it is important to consider that the nature of the reparative action and ease with which it can be implemented will have an influence on the dissipation of feelings of guilt. Thus, if corrective action does not occur in either thought, word or deed then guilt experiences can be converted into shame experiences. Lewis also observes a further difference between shame and guilt in that an individual has the capacity to feel ashamed of guilty actions but not be guilty over being ashamed. Lewis identifies these behavioural differences between shame and guilt as being central to differentiation between the two emotions and in measuring individual differences. He also argues that as guilt is not as intensely aversive as shame it is not so all consuming and potentially destructive to self. Indeed, he argues guilt serve a positive function in motivating an individual to engage in reparative action.
The distinction Lewis draws between shame and embarrassment is defined in negative terms, i.e. embarrassment is less intense than shame and is not disruptive to thought processes and behaviour in the same way as is shame. He draws on research literature on facial expression and body posture and display of self-conscious emotions which are universal across cultures (Izard 1977) to make a clear distinction between embarrassment and shame in these terms. Thus, he observes that the facial expression and body posture in embarrassment reflects what he terms ambivalent approach and avoidant posture characterised by repeated looking away and accompanied by smiling.
Lewis differentiates between two forms of embarrassment, namely embarrassment as exposure and embarrassment as less intense shame. In his account of embarrassment as exposure Lewis makes the point that in certain situations of public exposure embarrassment is elicited. However, this embarrassment is not related to a negative evaluation of self as in shame. He uses the example of the way in which being paid a compliment can elicit embarrassment. Thus, a speaker at a conference is introduced to the audience and the convener spends a few minutes publicly extolling the virtues and achievements of the speaker and as a result the speaker experiences embarrassment. Thus, rather than displeasure or judgement being the trigger for the feeling of embarrassment it is compliments and praise. Therefore, in line with Lewis’ model, in this example there is no negative evaluation of self in relation to SRG’s and therefore in this context embarrassment cannot be a less intense form of shame but is more to do with exposure than self-evaluation.
In considering embarrassment as a less intense experience of shame Lewis proposes that this is related to negative self-evaluation and he accounts for the variation intensity of the emotion experienced as being a direct product of the degree to which the relevant SRG associated with the triggering of emotion is associated with a core sense of self. Thus, failures associated with lower order SRG’s will elicit embarrassment whereas higher order SRG’s related to core constructs of self will elicit shame. From this Lewis extrapolates his theory to suggest that each of the self-conscious emotions identified in his model will also have less intense forms in accordance with the relevance to core self-constructs of the eliciting SRG’s.
The final step in Lewis’s model is to make links between shame and emotional disorders in the context of children who experience trauma which he defines as sexual and physical abuse and neglect. Lewis is a Professor of Paediatric Psychiatry and Anthropology and his research is entirely in the field of children and self-conscious emotions in child development. He proposes a general model of psychopathology and shame which is diagrammatically represented in figure 3 below.
FIGURE 3: LEWIS’ PROPOSED RELATIONSHIP BETWEEN SHAME AND PSYCHOPATHOLOGY (LEWIS, 2000, P 632)
c
ATTRIBUTION
Thus, in the proposed model trauma (sexual and/or physical abuse and neglect) leads to shame via a process of cognitive mediation of attributions about the abuse (a) and shame (b) which gives rise to poor adjustment (d). Trauma can directly influence shame (c) and adjustment (e). According to Lewis (2000) individuals who are more shame prone are more likely to exhibit poor self-esteem, helplessness, psychological distress, depression and dissociation.
Thus, framed within his cognitive-attributional theory of self-conscious emotions an internalstable-global attributional style for negative events is a risk factor for shame and subsequent poor adjustment. He cites his own research to argue that the experience of shame as a consequence of sexual abuse is a central mechanism associated with subsequent behavioural disturbance in children. Of relevance here are the attributions made concerning the cause of the abuse and how the individual evaluates the sexual abuse events is central to the adjustment process. Thus, if the attribution made is to an internal-global cause, i.e. Selfblame the resulting emotion is shame and argues Lewis shame can then be formulated as an ‘intervening cause of the symptoms of psychological distress and depression’ (p 623). Research evidence examining attributional style and sexual abuse in adults abused as children supports the idea that attributional style marked by a tendency towards internal-global cause, i.e. self-blame mediates the long-term outcome of sexual abuse (Andrews 1998).
As a concluding comment Lewis (2000) calls for a continued development of a more accurate taxonomy for defining and describing self-conscious emotions and the related emotional disorders. In keeping with this call, the last two decades has seen great strides in research, in the field of self-conscious emotions, both in terms of identifying universal facial and postural displays of self-conscious emotions and models for understanding self-conscious emotions. This data, along with the essential tenants of Lewis’s model have been integrated into Tracy and Robins’ (2007a) model of self-conscious emotions, which offers a more comprehensive and cogent account of shame as a self-conscious emotion. This is described below.
Tracy and Robin’s appraisal-based process model of self-conscious emotions
Tracy and Robins’ (2007a; 2006; 2004) model draws on two fields of social-personality psychology, namely, self and emotions, and builds on previous theory and research as follows (summarised from Tracy and Robins 2007a, p: 9):
-
Causal attributions and emotions (Covington and Omelich 1981; Jagancinski and Nicholls 1984; Weiner 1985)
-
Cognitive appraisal and emotions (Lazarus, 1991; Scherer 2001; Roseman 2001; Elsworth and Smith 1988)
-
Cognitive antecedents of shame, guilt and pride (Lewis 2000; H.B. Lewis, 1971; Tangney, 1991)
-
Self-evaluative processes (Carver and Scheier 1998; Cooley 1902; Duval and Wicklund 1972, Higgins, 1987)
As a starting point for their model Tracy and Robins (2007a) state that a complete process model of self-conscious emotions must include all the following evaluative processes:
-
Self-focused attention
-
The activation of stable self-representations
-
Reflection upon discrepancies between a current self-state and some evaluative standard relevant to one’s identity (i.e. an ideal self-representation)
They argue that the inclusion of these facets is the defining feature of differentiating between self-conscious and non-self-conscious emotions. This model is represented in diagrammatic form in appendix IV.
The authors acknowledge that their diagrammatic representation of their model implies a serial step by step sequence of conscious appraisal. However, they concede that in reality the process will involve numerous feedback loops, which may operate bi-directionally and in parallel and that many of the appraisal processes may occur at a tacit level. They defend their decision to represent their model in the way described citing other noted appraisal theorists (e.g. Kappas 2001; Scherer 2001) who have presented their models in this way, arguing that this enables the articulation of appraisal theories of emotion and to quote: ‘elucidate the mental algorithms through which these processes determine which particular self-conscious emotion is produced’ (Tracy and Robins 2007a p16).
The model describes the sequence of appraisals leading to the elicitation of self-conscious emotions as moving through the following steps:
Step 1: Survival-Goal Relevance
This step involves the cognitive process of evaluating whether the eliciting event is relevant to the goals of survival and reproduction (c.f. Lazarus 1991). In line with appraisal and functional theories of basic emotions (see Lazarus 1991; Scherer 2001; Roseman 2001; Nesse 1990), events which are appraised as relevant to survival and reproduction goals will elicit one of the basic emotions. If the event is not appraised as relevant to survival or reproduction goals it will elicit no emotional response unless it is appraised as being relevant to identity goals. The authors note that there are a small class of eliciting events that produce emotions without goal-relevant appraisals. Examples they cite include viewing a work of art or a beautiful landscape, which may elicit joy without any cognitive mediation (Tracy and Robins, 2007a).
Step 2: Attentional Focus on Self and Activation of Self-Representations
This step involves the cognitive process of attentional focus referred to by the authors as the ‘I’ self which is directed towards the persons self-representations defined as the ‘me’ self. This gives rise to a state defined as ‘objective self-awareness’ (Duval and Wicklund 1972) or ‘selffocused attention’ (Carver and Scheier 1998). This state and the concomitant selfrepresentations which are activated lead the individual to make reflexive self-evaluations. The self -representations incorporated into Tracy and Robins model (Tracy and Robins, 2007a) are taken from (Higgins 1987) and are described as:
-
Actual or current self-representations (‘I am successful’)
-
Ideal or hoped for self-representations (‘I want to be successful’)
-
Ought self-representations (‘I should be more successful’)
Drawing on the work of Markus and Nurius (1986); Wilson and Ross (2001) and Robins, Norem and Cheek (1999), Tracy and Robins elaborate the definitions of these self-representations thus:
-
Concern past, present or future selves
-
May refer to private (personal) and public (relational, social, and/or collective) aspects of self.
It is these self-representations that constitute a person’s identity and within Tracy and Robins model these self-representations must be activated at an explicit or implicit level for a selfconscious emotion to be elicited. It is only through the process of self-focused attention they argue that a person can make comparisons between self-representations and the external event which elicits the emotional response. The authors cite work by Phillips and Silvia (2005) which showed that self-focused attention was a necessary prerequisite for the elicitation of a range of emotions in response to self-discrepancies.
Step 3: Identity-Goal Relevance
The third step involves the cognitive process whereby when attentional focus is directed towards self-representations then events can be appraised for relevance to identity-goals. That is to say, ‘does this matter for who I am or who I would like to be?’ Therefore, if an event is appraised as relevant to identity-goals and the next step in the sequence occurs, that of identity-goal congruence then a self-conscious emotion is likely to be triggered. Thus, selfconscious emotions are triggered when a person’s identity is threatened. For them this threat can arise in private or public and in relation to interpersonal situations or task provided the eliciting event is relevant to the aspirations, ideals and fears of the self. In this regard the author’s note that events appraised as relevant to identity-goals can also generate basic emotions, a point which is elaborated in step 5 of the model, internality attributions.
Tracy and Robins, (2007a) develop their discussion of identity-goal relevance by example, arguing that a social evaluation will not elicit self-conscious emotions if the person concerned does not make the corresponding self-evaluative appraisal i.e. public praise will not elicit pride if the person on the receiving end of the praise discounts the public evaluation. Similarly, negative evaluations will not elicit shame if they are related to non-self-relevant domains.
The authors cite a quote from the psychologist William James (1890) to illustrate this last point:
‘I, who for the time have staked my all on being a psychologist, am mortified if others know much more about psychology than I. But I am contented to wallow in the grossest ignorance of Greek’
(Tracy and Robins 2007, p 11)
Therefore, argue Tracy and Robins, it is the self-evaluation processes articulated in their model that act as mediators between social evaluation and self-conscious emotions. Thus, in this model, social evaluation lies at the heart of our self-concept, that is to say, our identities are a product of early socialisation. Of particular merit here is the Tracy and Robins model is the inclusion of private (as well as public) social evaluations within their model, thus providing a theoretical explanation for a commonly observed phenomenon in clinical practice when working with depressed patients, namely, self-conscious emotions (notably shame and guilt) can arise in response to events of which only the self is aware. This model therefore seems of utility in attempting to hone clinical models for understanding and working with selfconscious emotions such as shame and guilt in depression.
This position can be contrasted with researchers such as Kemeny, Gruenewald and Dickerson (2004) and Leary, (2007) who place the emotions triggered by social evaluations at the heart of self-concept arguing that the key goals associated with the elicitation of self-conscious emotions are not (as Tracy and Robins state) identity goals defined in broad terms but a range of identity concerns involving interpersonal, social or public events, which Tracy and Robins (2007a) argue is an inadequate account of the elicitation and experience of self-conscious emotions.
Step 4: Identity-goal congruence
The fourth step involves the cognitive process of appraising whether an event which has been appraised as relevant to identity goals is congruent or non-congruent with these goals. This appraisal determines the valence of the elicited emotion. Thus, positive emotions are elicited by goal congruent events and negative emotions by goal incongruent events (see Lazarus 1991).
The author’s note here, that in their diagrammatic representation of their model, (see appendix IV), they do not illustrate the fact that the pathway of appraisal of goal congruence would lead to two separate paths depending on congruency or incongruency. The subsequent series of appraisals are exactly the same but the outcome i.e. a positive or negative emotion is different. However, in order to simplify the diagram, the author’s combine the two pathways and show the resulting specific positive or negative emotions at the end of the model (see Tracy and Robins, 2007a p 16).
The model next proposes that the way in which an individual decides whether an event is congruent or non-congruent with identity goals is as follows:
Current self-representations are activated by the emotion eliciting event (e.g. failing your driving test) and these are compared with stable, long-standing self-representations including actual self-representations (I am a successful person ) and ideal self-representations (I want to be a successful person). As part of this process the person may identify a discrepancy between current, actual and ideal self-representations and as a result appraise the event as identity goal incongruent. As is illustrated in appendix IV, this would elicit a negative selfconscious emotion such as shame or guilt.
The author’s cite the work of Carver and Scheier, (1998) as the rationale for emphasising the role of discrepancies between current self-representations and more stable selfrepresentations and use this as the means by which to specify the distinct types of negative and positive emotions that are generated by such discrepancies. Carver and Scheier, (1998) propose that positive and negative affect are the output of what is termed a ‘cybernetic selfregulation process’ (Tracy and Robins 2007a, p 11), whereby, an awareness of a discrepancy between current self and some evaluative standard, such as an ideal selfrepresentation, generates negative affect,. Furthermore, if this discrepancy is reduced positive affect is generated.
Step 5: Internality attributions
This step involves the cognitive process that determines the causality of the event. The most important appraisal here is causal locus, namely is the event due to an internal cause? (i.e. residing in the individual themselves) or an event due to an external cause? (i.e. residing outside of the individual). In developing this aspect of their model, Tracy and Robins (2007a) draw on the work of a range of appraisal theorists who have studied attribution of causal locus and note that this is referred to variously in the literature as ‘credit or blame to oneself’ (Lazarus 1991); ‘accountability’ (Smith and Lazarus 1993); ‘agency’ (Ellsworth and Smith 1988; Roseman 1991); ‘responsibility’ (Frijda 1987) and ‘causal attribution check’ (Scherer 2001).
Within their model Tracy and Robins use a broad definition of causal appraisal, defined as: ‘Is it something about me or related to me that is the cause of this event?’ where ‘me’ involves every aspect of self-identity (Tracy and Robins 2007a, p 13). Thus, self-conscious emotions arise when the individual attributes the triggering event to an internal cause (Lewis 2000; Tangney and Dearing 2002; Weiner 1985). Once more when considering the relevance of this model with regard to working psychologically with depressed patient’s then clinical observation attests to this much more broad definition of causal appraisal, this being a common testimony from patients, e.g. a minor daily hassle such as the car breaking down can be attributed as ‘I am cursed’ ‘everything I touch goes wrong’.
The authors argue that this broad way of defining ‘me’ in their model is especially important when considering the self-conscious emotion of embarrassment where internal appraisals are often made about events for which a person has no responsibility or intentionality. They illustrate this with the example of the actor who forgets his lines, that we can have empathy for someone else’s embarrassment, in a vicarious way, without feeling it ourselves. However, if we identify with a person in such a way that their mistake feels as if it is our own, where ‘own’ is defined in a broader collective sense, as in a work colleague making a faux pas in a meeting, then our embarrassment is likely to be direct rather than vicarious (Tracy and Robins, 2007a). In this sense self-conscious emotions may be experienced vicariously, (see Lickel, Schmader and Spanovic 2007) or, more directly if there is a shared identity.
Similarly, this is also important in making sense of situations where a person can feel pride or shame in the actions of others who represents a shared collective identity. For example, if you are a woman who hails from Yorkshire and a Yorkshire woman wins a gold medal at the
Olympics you may feel pride on two counts, the fact she is a woman and that she is from Yorkshire. Similarly, if you are a member of the nursing profession and a colleague from your profession in a multidisciplinary conference arrives drunk to a keynote address and becomes disruptive you may feel ashamed based on a collective identity as a nurse.
Tracy and Robins (2007a) cite research studies to support this aspect of their model, which show that internal attributions for failure tend to result in feelings of guilt and shame and internal attributions for success tend to produce pride (Weiner 1985; Weiner, Graham and Chandler 1982).
Returning to the previous observation at step 3 of their model, that events appraised as relevant to identity-goals can also generate basic emotions, Tracy and Robins (2007a) argue that in modern society these internality-externality attributions may be the most frequent route for the elicitation of basic emotions, given that threats to actual survival are less frequent than threats to identity. Thus, when a person feels anxious or angry these emotions may be more likely to have been triggered by an external attribution for an identity threat such as not being invited to a social gathering, than by a direct threat to survival.
Step 6: Stability, Globality, controllability attributions
The final step in the model involves the cognitive process of three other causal attributions which are key, not only to the elicitation of self-conscious emotions but, also to differentiating between them. These are:
-
Stability
-
Globality
-
Controllability
Research links these attributions to a range of emotional states (see Covington and Omelich 1981; Tangney, Wagner and Gramzow 1992 and Tracy and Robins 2006) and in summary:
-
Stable causes are more likely to be global and uncontrollable
-
Unstable causes are more likely to be specific and controllable.
Once these five steps have been activated this results in the elicitation of Self-conscious emotions. When considering the elicitation of shame and guilt, Tracy and Robins (2007a) cite evidence from research conducted by several emotion theorists that demonstrates, whilst shame involves negative feelings about the stable, global self, guilt involves negative feelings about a specific behaviour or action taken by self, (i.e. H.B. Lewis 1971; Lewis 2000; Tangney and Dearing 2002). Tracy and Robins (2007a) utilise this formulation in their model and specify that:
-
Internal, stable, uncontrollable attributions (‘I am a stupid person that’s why I failed the exam’) lead to shame
-
Internal, unstable, controllable and specific attributions (‘I did not revise hard enough, that’s why I failed the exam’) leads to guilt.
Thus, where poor performance is attributed to ability (an internal, stable and uncontrollable factor) shame will be elicited, whilst if attributed to effort (an internal, unstable, controllable factor) guilt will be elicited (c.f. Brown and Weiner 1984; Covington and Omelich 1981). In addition, individuals who tend to make internal, unstable, controllable attributions tend to be more guilt prone and those who make internal, stable, uncontrollable attributions tend to be more shame prone (Tangney, Wagner and Gramzow 1992; Tracy and Robins 2006).
Similarly, a prerequisite to the elicitation of embarrassment in this model is an appraisal of identity-goal relevance and identity-goal incongruence and attribution to internal causes.
However, embarrassment does not, (as in shame and guilt), require any further attributions and only occurs when attentional focus is directed towards the public self, thus activating concomitant public self-representations. Thus, as Tracy and Robins (2007a) exemplify, an individual can be embarrassed by an event caused by internal, stable, uncontrollable and global aspects of public self for example being publicly exposed as incompetent or by events caused by internal, unstable, controllable and specific aspects of public self, such as spilling a cup of coffee on your boss. Importantly in this model, the authors observe that activation of the public self does not require a public context, but rather the public self is always present because it reflects the way we see ourselves through real or imagined eyes of others (Tracy and Robins 2007a p 14). Thus, when considering embarrassment as an emotion, what is important is not whether the action eliciting the emotion occurred in public but rather whether the public self has been activated. In this account of embarrassment, the emotion is viewed as being less cognition-dependent (when compared to shame and guilt) as it does not require the additional appraisal dimensions of stability, controllability and globality which shame and guilt require.
Tracy and Robins (2007a) conclude their model with a discussion of two facets of pride which they label as authentic and hubristic pride and which parallel shame and guilt as follows:
-
Global pride in self (‘I am proud of who I am’). This is akin to Lewis’ (2000) description of hubris and Tangney, Wagner and Gramzow’s (1992) description of ‘alpha pride’ and arises in the context of attributions to internal, stable, uncontrollable and global causes.
-
Authentic pride (‘I am proud of what I did’) arising in the context of specific attributions to internal, unstable, controllable and specific causes based on specific achievements.
There is some empirical support for this distinction (Tracy and Robins (2007b).
Applying appraisal-based process models of self-conscious emotions in research
Van Vilet (2009) conducted a qualitative study exploring how adults recover from specific shame events. She interviewed members of the general public recruited via an advert in a local newspaper (N = 13). Her research is grounded in attribution theory and her explanatory model utilises the appraisal-based process models described previously (Lewis 2000; Tangney 1995). She formulates shame as arising in response to threatened attachment ties in which the constructs of powerlessness and self-blame are key factors. Van Vilet (2009) assigns the experiences of the participants to four categories as follows:
-
Social and moral transgressions (n=6)
-
Personal failure (n=2)
-
Ostracism and social rejection (n=3)
-
Trauma (n=1)
In this small sample most participants associated shame with internal attributions of causality and self-blame for having caused the event. Shame also involved negative self-judgements that related to a core sense of self (i.e. self-disgust or defectiveness) and participants described a sense of powerlessness in changing perceived defects. Several facets related to the experience of shame are identified by Van Vilet’s participants as follows:
-
Self-judgments were global and entire self was judged
-
Damage to self-concept due to a perception of having fallen short of their own internal standards and ideals
-
Perception they had not lived up to the expectation of others
-
Perception of feeling exposed, lowered and unattractive in the eyes of others
-
Perception they were powerless to escape an unwanted social identity
The emotion of anger was frequently reported by participants and this took two forms. Anger and aggression directed at self, however, in cases of humiliation and ostracism (n=2) participants felt they had been unjustly humiliated or ostracised by others and anger was directed at others. In this latter context shame was seen to emerge not from internal causal attributions but from having an unwanted identity or damaged social image.
Van Vilet, (2009) also explored with the participants attributional pathways to recovery and identified three key processes:
-
Identifying external causes and processes and extenuating circumstances that were beyond the persons control
-
Reducing global self-judgements
-
Believing in the possibility of change
Within these themes’ participants gave examples of how they have worked to overcome feelings of shame. These included:
-
Acceptance of mistakes and trying to move towards more realistic self-ideals which were not governed by absolute standards.
-
Separating self from behaviour
-
Focus on what action the person could take to change, thus increasing the person sense of agency (i.e. controllability)
-
Focusing on the needs that might have led the person to engage in a certain behaviour and focus on more healthy motivations
-
Acceptance of personal responsibility and redress the harm caused to others
In reflecting on these examples of attributional pathways to recovery most of them seem to more readily meet Lewis (2000) and Tracy and Robins (2007a) criteria for addressing guilt related attributions rather than shame. This highlights the point that is observed frequently in the self-conscious emotion literature, that the relationship between guilt and shame is much debated and the two often conflated, not perhaps only in academic literature but every day in human experience (Blum 2008). As Tracy and Robins (2007a) observe their model is a simplification of what are likely to be complex processes. In many instances it is likely that shame and guilt will co-occur, and it would seem important not only to discriminate between these two emotions but to also consider their interplay. Van Vilet’s (2009) participants accounts of what is labelled as shame are detailed, nuanced and highly idiosyncratic. Whilst this may lend some validity to the ideas posited by Lewis (2000) and Tracy and Robins (2007a), that self-conscious emotions involve complex cognitive attributions, it raises the question of how do individuals experience, describe and label self-conscious emotions. Can we easily identify when we feel shame and when we feel guilt? A flaw in Van Vilet’s study is she only examined shame experiences and yet, reflecting on the examples offered by participant’s, the clinical experience of the author of this thesis would suggest feelings of guilt may also arise in the context of these events. In addition, in seeking to work clinically with shame and guilt it seems much easier to assuage guilt (internal-unstable, controllable and specific attributions about behaviour) by addressing the errant behaviour, allow for mitigating circumstances and make reparation (as is attested by the examples given by Van Vilet’s participants) than to condemn the whole self (internal-stable-uncontrollable attributions) and then seek to alleviate the self-loathing that is inherent to such global condemnation.
Tangney, Wagner, and Gramzow (1992) examined the relationship between shame, attributional style and depression in 1,254 undergraduate students and found shameproneness not only to be linked to attributional style (i.e. a tendency to make internal, stable, global attributions) but that this link could not be accounted for by attributional factors alone. In conducting multiple regression analysis on the Beck Depression Inventory-I (BDI-I) (Beck, Ward, Mendelson, Mock and Erbaugh, 1961) and Symptom Checklist-90 (SCL90) (Derogatis, Lipman, and Covi, 1973) to predict depression scores from the attributional style variable, the researchers found that attributional style accounted for 9% of the variance in depression for the BDI-I and 7% for the SCL-90. Further, internal attributions for negative events was a significant predictor of both BDI-I and SCL-90 scores and unstable attributions for positive events was also a significant predictor of BDI scores. The researchers conclude that the link between shame and depression is not purely a facet of attributional style and once the affective component of shame is included, whilst controlling for attributional style, the proportion of variance predicted in depression is doubled (Tangney, Wagner, and Gramzow 1992 p 477).
The evolutionary and biopsychosoical psychology model of shame
The overall aim of this PhD study is to examine the role of shame, self-criticism and selfcompassion in a cohort of patients diagnosed with persistent, treatment resistant depression. The theory which underpins the study and the psychometric measures being tested is that of Gilbert (2017a; 2017b; 2009; 2007a; 2005a; 2005b; 2000; 1998; 1995; 1992) who proposes an evolutionary and biopsychosocial model of shame. This model is illustrated in figure 4.
FIGURE 4: AN EVOLUTIONARY AND BIOPSYCHOSOCIAL MODEL OF SHAME (GILBERT 2007A P.301)
Innate motives for attachment and group belonging; needs to stimulate positive affect in minds of others; unfolding cognitive
competencies for self-evaluations
Social-cultural contexts relating to economic opportunities, group
conflicts, political structures, cultural rules for honour/pride/shame
PERSONAL EXPEREINCES OF SHAMING-STIGMA
Family: criticism, high expressed emotion, negative labelling, abuse
Social group: bullying, discrimination, prejudice, stigma
Gilbert (2007a) begins with the premise that as human beings we have evolved to be social and as a result we possess a set of, what he terms, social motivational systems which are intrinsic and necessary to our survival. Gilbert identifies two key social motivational systems (Gilbert 2007a):
-
The capacity to seek out and respond to carers and our wider social group
-
Our concern with our relative social place i.e. being treated by others as inferior, equal or superior.
Further, Gilbert (2007a) posits humans have evolved specific cognitive, metacognitive and symbolic skills in order to facilitate social understanding. These include:
-
Theory of mind (the capacity to think about someone else, their motives, what they value, what we can do to manipulate them to like us or be wary of us).
-
Self-conscious awareness (the capacity to have a sense of self-who we are and for selffocused feeling).
-
Metacognition (the capacity to think about our thoughts, feelings and behaviour and to evaluate their implications and consequences and to pass judgement as to their merits or otherwise).
As a result of these evolved processes humans are especially sensitive to what others think and feel about them and have developed both conscious and non-conscious processes which constantly monitor what Gilbert terms, ‘self-in-relation to other’ (Gilbert 2007a). These processes guide both how we interact with others and how we evaluate ourselves.
Importantly in Gilbert’s theory, humans are so dependent on social relationships to survive that our interactions with others shape how our brains develop from birth. The mechanism for attachment in humans between parents and infants serves an important evolutionary goal, that of reducing threat. Thus, parental care provides not only protection but parental engagement and interaction enabling the capacity to soothe and to feel calm, secure and safe. As a result, Gilbert argues, humans have developed what he terms a ‘social safeness system’ (Gilbert 2007a p 286) that is highly sensitive to certain social cues including touch, voice tone, facial expressions and access to care provided by others. This system is associated with the release of certain neuro-hormones such as oxytocin and endorphins which provided the neural basis for soothing and feeling soothed. Further, these cues do not simply indicate an absence of threat but are associated with a range of positive affect systems, specifically what Gilbert terms the ‘affiliative and affectionate behaviour systems’ (Gilbert, 2007a p 286).
Thus, from the first days of life it is not just an absence of threat that is vital to the development of these systems it is also what is given by the caregiver. Specific signals from the caregiver stimulate the ‘social safeness system’ through touch, voice tone, facial expressions, feeding and mutually rewarding engagement. It is these that form the foundation of the attachment bond and signal a sense of support, safety and friendliness (as opposed to hostility). Therefore, what is going on in the mind of the mother is translated into a range of behaviours in which the mother is able to influence the mind of her baby through a process of what is termed ‘empathic resonance’ known as inter-subjectivity (see Knox, 2013 for a description of this process). This inter-subjectivity represents:
‘moment to moment co-regulation of participants as they experience the feelings of others
directed at them’
(Gilbert 2007a p 289).
These co-regulated interactions between mother and baby shapes how the infants brain/mind develops as neural connections are made in the brain. As the child continues to develop they interact with others and how these people, particularly primary care givers, understand and empathise with the child’s emotions and behaviour significantly influences the child’s capacity to understand and regulate their own emotions, behaviours and personal attributes, which in turn are integrated into the child’s self-processing and self-defining systems. This inter-subjectivity remains important throughout life and in Gilbert’s model is a key process in the emergence of shame.
The absence or withdrawal of these positive stimuli such as might be observed in a depressed mother, (e.g. not giving eye contact; not smiling at, holding or talking to her baby) exerts an adverse effect on the development of the baby through an absence of interactions that create, in the baby, experiences of safeness and soothing. Thus, the quality of the care and affection humans receive in their early years of life has consequences for how able or otherwise humans are to develop a sense of self in which they can regulate their affect and feel sufficiently safe in the world to develop supportive and cooperative relationships ( Raby, Lawler, Shlafer, Hesemeyer, Collins Sroufe, 2015; Sroufe, 2005; Claesson and Sohlberg, 2002; Baumeister and Leary, 1995; Bowlby 1973; 1969).
Thus, in Gilbert’s model the ability to experience self as ‘positive in the mind of the other’ has three important anticipatory consequences (Gilbert, 2007a p 289):
-
The other is safe and therefore one can relax in their presence
-
The other will be positively disposed to help and soothe the self if needed
-
The other will co-operate in the development of relevant social roles and activities in a mutually beneficial way
Thus, a sense of safeness and acceptance is key to human survival through a process of experiencing ourselves as existing positively in the minds of others. Gilbert’s model posits that shame as an affect serves as a warning that we are in danger of or have lost this sense of being valued and accepted by others and this is directly linked to humans evolved safenessthreat processing mechanism.
For Gilbert shame is a result of our evolved abilities to be aware of how others might think and feel about us. Gilbert (2007a) cites several shame theorists (Lewis 2000; Nathanson 1987; Tracy and Robins 2007; 2006; 2004) and observes they define shame as an experience in which the individual perceives failures and flaws are exposed thus giving rise to a sense of self as unattractive or unwanted. Gilbert defines this as as internal shame. For Gilbert, internal shame is linked to our memory systems which include previous experiences of being shamed and self-evaluation’s where attention is focused on self-feelings and self-judgement (Tracy and Robins, 2007a; 2004).
However, Gilbert (2007a; 1998; 1995), argues that what is of central importance in the onset and maintenance of emotional disorders is external shame. Here, external shame is defined in terms of an individual’s monitoring systems becoming externally directed toward what is going on in the mind of the other. Thus, a person’s feelings and actions are attuned and coordinated to track the actions, signals and intentions of others, mediated by the cognitive competencies described earlier. External shame is central to Gilbert’s theory because, he argues, humans have evolved to compete for their place in a social rank by creating positive images of self in the minds of others. This is advantageous to survival as it increases our chances of belonging to a chosen group, feeling wanted and to be chosen as a romantic partner, friend or team member.
Further, Gilbert formulates internal shame as a manifestation of external shame. He defines this as a process of internal shaming, a form of self-attack, that is self-denigratory. This concept of internal shame is discussed more fully in the section of this chapter which examines self-criticism within an evolutionary frame.
Therefore, according to Gilbert’s model, emotional disorders will arise when there is disruption in social relationships and where interactions with others convey that self is in some way unattractive or unwanted by others. The resultant emotion being shame when that which is deemed unattractive by others is exposed. Thus, the maintenance of emotional disorders is a product of three interconnected processes (summarised from Gilbert, 2007a, p 294–296):
-
External shame, which arises in disruption in social relationships where interactions with others convey a negative sense of self in the mind of the other, where self is experienced as unattractive, undesirable, or unwanted. In this context the world and interactions with others are experienced as threatening and hostile with the concomitant fear of rejection, criticism, ridicule or abandonment.
-
Internal shame, manifest in self-attack in the form of high self-criticism (see below for a full discussion of this aspect of Gilbert’s model).
-
The inability to access and activate self-soothing systems and generate positive images and feelings towards self, which is described in terms of low levels or an absence of self-compassion (see below for a full account of this construct).
The definition of self-criticism
The research literature over the last fifty years reveals a range of descriptors which have been used to define and investigate the construct of self-criticism (Aronfreed, 1964). In addition to this latter phrase, others include lowered self-concept (Laxter, 1964a); low self-acceptance (Grusec, 1966); self-blame (Janoff-Bulman, 1979; Abramson and Sackheim, 1977; Beck, 1967); self-loathing, self-hate, self-persecution (Gilbert, 2017a; 2007a; 1995); Selfattack/selfdevaluation/self-condemnation/self-denigration (Gilbert, Clarke, Hempel, Miles and Irons 2004) and self-contempt/disgust (Green, Moll, Deakin, Hulleman and Zahn, 2013). These descriptors are not well delineated in definitional terms in the research literature and in the clinical literature are often used interchangeably. The author of this thesis would make an argument for a clear distinction needing to be made between self-criticism and self-blame.
This is delineated further, later in this chapter.
Louis Paul (1970) in his paper, ‘The Cruel Inner Critic’ elegantly captures the clinical manifestation of self-criticism, defining the cruel inner critic as:
‘that person-in-the-person who is hostilely monitoring and directing the person to fail’
(Paul, 19 p 178).
Paul provides an experiential psychotherapy perspective on working psychologically with what he terms the ‘inner critic’ (Paul, 1970, p 178) which is articulated in the form of a clinical polemic delineating the observed features of the inner critic in action and the proposed experiential interventions.
Attempts to develop more precise definitions of self-criticism as a psychological construct are also represented in the literature. Carver and Ganellen (1983) examine depression in the context of behavioural self-regulation and the tendency towards self-punishment and identify self-criticism as an aspect of self-punishment. The authors define self-criticism as: ‘making harsh judgements of oneself having failed to attain a predetermined standard’
(Carver and Ganellen, 1983, p 330).
More recent definitions of self-criticism have encapsulated more than one dimension. Thompson and Zuroff (2004) formulated what they considered to be two independent types of self-criticism termed ‘comparative self-criticism’ and ‘internalised self-criticism’. The former is associated with negative perceptions of self in comparison to others and the latter, negative perceptions of self with regard to certain personal standards. Similarly, Gilbert, Clarke, Hempel, Miles and Irons (2004) demonstrated that two forms of self-criticism could be delineated, feeling inadequate and inferior and feeling hatred for the self. Further, Gilbert and colleagues (Gilbert, Clarke, Hempel, Miles and Irons, 2004) in examining the function of self-criticism identified two factors; a desire to improve the self and avoid making mistakes and a drive to take revenge on the self, which is labelled as self-persecution.
Drawing on this latter work Ehret, Joorman and Berking, (2015) define self-criticism as:
‘a response style to a perceived failure that is characterised by negative self-judgment and
self-evaluation’
(Ehret, Joorman and Berking, 2015, p 1496).
As the proceeding discussion of the distinct theoretical models of self-criticism reveals, this definition represents an integration of these perspectives enshrining elements from the depressive rumination literature (i.e. ‘response style’ Nolen-Hoeksema, 2000), cognitive theory, (i.e. ‘perceived failure’ Beck, 1983; 1967), attribution theory (i.e. ‘negative selfevaluation’ Lewis, 2007; Tracy and Robins, 2006; Abramson, Seligman and Teasdale, 1978) and evolutionary psychology (i.e. ‘negative self-judgment’ Sturman and Mongrain, 2005; Gilbert, Clarke, Hempel, Miles, and Irons, 2004).
Unsurprisingly, theoretically discreet models aimed at delineating the concept of self-criticism as a psychological construct parallel the emergence of each of the major Twentieth century psychotherapy traditions and the social and cultural zeitgeist in which they developed. A brief summary of these will follow.
The psychoanalytic Formulation of Self-criticism
The Freudian psychoanalytic formulation (Aronfreed, 1964; Laxter 1964a; 1964b; Grusec 1966) views self-criticism (defined as low self-concept or low self-acceptance in this early literature) as a behavioural manifestation of guilt and posits that a person experiences depression as a result of anger turned inwards against the self. Thus, in depression selfacceptance will be lowered as a result of the aggression which will result from frustration or failure turned inwards against the ego. Conversely, people who turn their anger outwards by projection can more successfully protect their self-concept and therefore will hold a greater level of self-acceptance (Laxter, 1964a, p 538). Grayson (1983) using an Adlerian formulation of self-criticism and self-blame, defines these processes as unconscious and tactic, aimed at protecting self- esteem. Thus, he argues people who denigrate themselves as bad, incompetent, inadequate or worthless do so with a hidden motive of self-enhancement, i.e. ‘they condemn themselves the better to exalt themselves’ (Grayson, 1983, p 17). These early publications are discussion papers which theorize regarding the origins and maintenance of self-criticism.
Also, within a psychoanalytic frame, Blatt (1974), developed a model which proposed two personality factors which underlie both clinical and non-clinical depression, termed ‘anaclitic’ and ‘introjective configurations’, which he argued gave rise to two distinct forms of depression. Klein, Harding, Taylor and Dickstein (1988) define these as follows. The ‘anaclitic depressive state’ is manifest in dependency, helplessness, tearfulness, somatisation and sensitivity to events in the environment, emptiness, lability of affect, impulsivity and selfharm. Meanwhile, the ‘introjective depressive state’ is associated with anhedonia, lack of reactivity, social withdrawal and intense feelings of guilt and worthlessness. Blatt developed the Depressive Experience Questionnaire (DEQ) (Blatt, D’Afflitti and Quinlan, 1976), a psychometric measure to investigate these two forms of depression. The scale has two major sub-scales, dependency, which measures the ‘anaclitic state’ and self-criticism which measures the ‘introjective state’.
These two personality configurations have been systematically investigated over the decades
(e.g. Klein, Harding, Taylor, and Dickstein, 1988; Blatt, Quinlan, Chevron, McDonald, and Zuroff, 1982; Sturman and Mongrain 2005) and as the literature has developed these configurations have been relabelled the ‘dependent’ and the ‘self-critical’ personality styles (Blatt and Zuroff, 1992; Sturman and Mongrain 2005).
The Behavioural Formulation of Self-criticism
In contrast, behavioural formulations (Grusec, 1966, Aronfreed 1964, Maccoby, 1959; Mowrer, 1950) describes the origin of self-criticism in a behavioural paradigm, framed within social learning theory (Bandura, 1977), in which self-criticism is conceptualised as learned in childhood. This occurs via a process of internalisation in which the child replicates certain components of reward and/or punishment to which they have been exposed whilst growing up. This is achieved by the process of reinforcement in which self-criticism serves the function of either lowering anxiety or receiving praise. Within behavioural formulations the antecedents and consequences of self-criticism are considered to be independent of the cognitive content that defines self-criticism.
The cognitive formulation of self-criticism
Self-blame is a key construct in Beck’s original formulation of depression (Beck, 1983; Beck, 1967) where he observes the person experiencing depression as more readily taking responsibility for events with a negative outcome which in turn activates feelings of guilt. Beck (1967) uses the descriptors ‘’self-blame’, ‘self-criticism’ and ‘low self-evaluation’ in his early work, when defining the parameters of depression based on his own clinical observations.
Beck (1983), also proposed a model (sociotropy-autonomy) delineating specific personality types susceptible to depression. In this model the autonomous personality type is associated with high levels of self-criticism focused around achievement of internalised standards and goals. Research focusing on this construct has demonstrated a state rather than trait vulnerability to depression (e.g. Coyne and Whiffen, 1995).
The Attributional Theory formulation of self-blame
The 1970’s saw the emergence of cognitive and attributional models of self-blame. Attribution theory holds that depressed individuals make internal, stable, global attributions for negative events and external, unstable, specific attributions for positive events. This attributional style represents a vulnerability to MDD resulting from overgeneralised selfblame manifest in a sense of worthlessness and hopelessness (Abramson, Seligman and Teasdale, 1978). Attributional formulations of self-blame seek to identify a causal relationship between action and outcome in the context of controllability of an event. Thus, for personal responsibility for an outcome to be attributed to a person, that person must, when deciding on a course of action, have had the option of following an alternative course of action other than that chosen. There is an assumption therefore that the original act and its outcome stand in a relationship to controllability i.e. act-outcome dependence.
Abramson and Sackheim, (1977) identified what they referred to as, the ‘paradox of depression’ in which they proposed an intrinsic incompatibility between two prominent theories of depression which had as their basis the constructs of hopelessness and self-blame, namely the learned helplessness model of depression (Seligman, 1975) and Beck’s cognitive model of depression (Beck, 1967). The authors argued that the learned helplessness model of depression holds that the individual experiencing depression perceives that outcomes are largely uncontrollable. Meanwhile, Beck’ s theory of depression identifies self-blame as a key clinical feature of the disorder. For Abramson and Sackheim, (1977), the idea that the person with depression could simultaneously view events as uncontrollable and yet blame themselves for the outcome of those same events was paradoxical. At the time they proposed a range of hypotheses as to how the paradox might be resolved and made suggestions for the future focus of research in this area.
In this vein, Janoff-Bulman (1979) demonstrated this paradox existed in a cohort of college students and proposed two forms of self-blame, ‘behavioural’ and ‘characterological’. Behavioural self-blame is related to control and attributions associated with this are connected to a person’s behaviour. As such, these attributions are open to change and are associated with a perception that in the future, negative outcomes associated with the event, that led to the behavioural self-blame can be avoided. Meanwhile, characterological selfblame is, according to Janoff-Bulman, related to self-esteem and refers to attributions regarding one’s character, which are not readily amenable to change. Further, characterological self-blame is associated with a perception that past negative outcomes are deserved. Janoff-Bulman (1979) studied rape victims and found that depressed female college students engaged in a greater degree of characterological self-blame than their nondepressed counterparts. On this basis Janoff-Bulman proposes the distinction between behavioural and characterological self-blame as a solution to the ‘paradox in depression’ (Abramson and Sackeim, 1977).
The work of Blatt, (1974) and Blatt, D’Afflitti and Quinlan, (1976) cited above was also tested in relation to attributional style. Brown and Silberschatz, (1989), studying a cohort of psychiatric out patients meeting a range of diagnostic categories (60% diagnosed with depression) found that those high in both dependency and self-criticism were more likely to hold themselves responsible for negative events, which in attribution terms is a marker for internal causal attribution.
Tanganey and Dearing (2002) attribute what is seen in the literature as this important distinction between characterological and behavioural self-blame to Helen Block Lewis and give an account of the phenomenological differences between shame and guilt as described by her (H.B. Lewis (1971). Thus, shame is described as an excruciating emotion accompanied by a sense of shrinking or ‘being small’ and exposed, with a desire to escape, hide or disappear. This sense of exposure does not necessarily require an audience to bear witness to the focus of the shame and often the feeling of shame is elicited by a picture in the mind’s eye of how self would appear to others. Alongside these experiences is a sense of self as worthless and powerlessness in which:
‘the observing self witnesses and denigrates the focal self as unworthy and reprehensible’
(Tangney and Dearing, 2002, p 18).
In contrast H.B. Lewis describes guilt as a less intense emotion where the focus is on behaviour and as such is partially removed from self and therefore does not impact on the core sense of self. Guilt is thus associated with a sense of remorse and regret, alongside a preoccupation with the behaviours associated with the feelings of guilt and the ‘why’ and ‘if only’ of wishing they the transgressor had behaved differently.
Tangney and Dearing (2002) cite research literature from the field of both quantitative and qualitative research supporting this distinction between characterological and behavioural self-blame and their concomitant associations with the experience of, respectively, the emotions of shame and guilt (Tangney and Dearing, 2002). For example, Peterson, Schwartz and Seligman (1981), studying a cohort of undergraduate students found that internal, characterological attributions were associated with depressive symptoms, whilst the same did not hold true for both internally and externally attributed behavioural attributions. In addition, Tangney and Dearing themselves have conducted a range of studies which support this distinction (see Tangney and Dearing 2002 for a comprehensive account of this research).
This distinction between characterological and behavioural self-blame forms the basis of the attributional models of self-conscious emotions described above (Lewis, 2000, 2007; Tracy and Robins, 2007a) and as such each represents the cognitive correlate to the emotions of guilt (behavioural self-blame) and shame (characterological self-blame). The distinction is also utilised in Gilbert’s evolutionary, psychobiosocial model of shame (Gilbert, 2007a).
Tangney and colleagues have conducted extensive research in the field of shame and guilt
(Tangney and Dearing, 2002; Tangney, 1995; Tangney, 1991; Tangney, 1990; Tangney, Wagner, and Gramzow, 1992) and have observed that among shame-prone individuals, as well as making the expected internal, global, stable shame based attributional responses, there is an absence of empathy for others and a tendency to externalise cause or blame. This seeming contradiction (in attributional terms) is accounted for by formulating this externalisation of blame as a defensive strategy to protect the individual from being overwhelmed by the excruciating pain of the shame experience (Tangney, 1991). Overall Tangney concludes that, whilst in the short term this strategy may have a useful function of reducing the individuals excruciating feelings of shame, in the medium- and long-term shame is a far more toxic emotion than guilt. The former may exert a significant detrimental effect on interpersonal functioning whilst the latter may serve a useful function in facilitating reparative action by eliciting an empathic response for the distress of the other. This is observed by other researchers in the field of self-conscious emotions and is referred to as ‘humiliated fury’ (Tangney, Wagner, Hill-Barlow, Marschall and Gramzow, 1996) Tangney, Wagner, Fletcher and Gramzow 1992; Lewis, H.B. 1971) and is an aspect of Gilbert’s shame theory (Gilbert, 2007a; Gilbert, 1998).
The evolutionary formulation of self-criticism
According to Gilbert’s shame theory described above (Gilbert, 2017a; 2007a), self-criticism is an aspect of internal shame. He defines internal shame as a process of internal shaming of self where a person is self-critical, self-attacking and self-persecutory and which carries a harsh self-denigratory tone. Importantly in Gilbert’s model this process goes beyond the cognitive attributions of self-blame described in attributional models of shame (Tracy and Robins, 2007a; Tangney and Dearing, 2002) and in addition involves intense feelings of anger, loathing and contempt towards self (Gilbert and Irons 2005). From an evolutionary perspective this process of self-attack represents a form of submissive behaviour and is a defensive strategy for coping with hostile aggression from a dominant other, in whose eyes one sees oneself as unattractive or unwanted (Gilbert, 2007a; Gilbert, Cheung, Grandfield, Campey and Irons 2003; Gilbert 1998). Thus, according to Gilbert, to some extent selfcriticism may be driven by what he describes as non-conscious submissive strategies aimed a coping with hostile and rejecting others (Gilbert and McGuire, 1998). The aim being to maintain attachment by blaming self and directing anger at self as to direct this at the dominant, hostile other risks rejection, criticism, ridicule, abandonment of harm.
Gilbert (2000), observes a relationship between self-criticism and entrapment in the context of this process of internal shaming, in which the subjective report of self-critical individuals is imbued with a sense of internal entrapment, which is defined as being unable to escape from their own negative thoughts and feelings. Gilbert hypothesises a link between this internal entrapment and depressive experiences via the process of arrested flight (Gilbert and Allan, 1994). Gilbert terms this as ‘internal dominant’ in relation to self (c.f. Sturman and Mongrain, 2005).
This concept of ‘internal dominant’ is borne out by the clinical experience of the author of this PhD thesis whereby, the person with depression is paralysed by such self-attack and exhibit both hopelessness and helplessness in relation to trying to use standard cognitive therapy interventions to lessen its impact. This in turn gives rise to a generalised sense of powerlessness and defeat (arrested flight) leading to behavioural withdrawal and/or avoidance which ultimately generates further intensified self-attack. This experience is dominated by anger towards self, culminating intensification and persistence of depressed mood.
Sturman and Mongrain, (2005), in the context of an evolutionary model of depression investigated the self-critical personality style (Blatt and Zurfoff, 1992, Blatt, 1974) and the relationship between the evolutionary variables of social comparison and entrapment and depressive symptomatology. These researchers defined the self-critical personality style as ‘an unforgiving performance standard coupled with self-loathing and guilt’ (Sturman and Mongrain, (2005), p 507) citing literature that associates it with depressive symptomatology
(Blatt and Zuroff 1992; Nietzel and Harris, 1990). In their study, which used a cohort of 835 undergraduate students who had experienced at least one prior episode of major depressive disorder (of which 122 were not currently experiencing a depressive episode) they found that self-criticism predicted internal entrapment (see below for a summary of this concept) and social comparison when controlling for dependency and depression. Further, the authors examined the mediational role of the evolutionary constructs under investigation and found self-criticism was associated with a greater number of depressive episodes leading the authors to designate self-criticism as a marker for vulnerability to depression (Sturman and Mongrain, 2005).
Theories of the nature and origins of self-criticism and self-blame
As with shame, (as highlighted earlier in this chapter), traditionally psychiatry defines selfcriticism as a symptom of depression (Blatt, Quinlan, Chevron, McDonald and Zuroff, 1982; Paykel, 1971; Beck, 1967). There is debate in the research literature as to whether or not, selfcriticism can be formulated as a vulnerability factor in depression, given there is a strong body of evidence from a range of disciplines that the presence and intensity of selfcriticism can vary according to severity of depressed mood (Coyne and Whiffen, 1995; Brewin and Furnham, 1987).
As stated previously, the manifestation of self-criticism is ubiquitous in depression and as is described in chapter one of this thesis, the current cognitive science of depression literature holds that the frequency and intensity of the negative content of thought processes in depression (including self-critical and self-blaming thoughts) will vary according to the severity of depressed mood (see Schwarz and Clore, 2003 for a summary). This observation is found in the research literature as far back as Laxter (1964a), who investigated the relationship between severity of depression and self-blame within the framework of psychoanalytic theory of depression. Klein, Harding, Taylor and Dickstein (1988), carried out the first study to test Blatt’s hypothesised ‘anaclitic’ and ‘introjective’ personality styles (Blatt, 1974). Their study used a diagnostically heterogeneous clinical sample of participants (as opposed to college students) diagnosed with depression. Whilst the cohort scored significantly higher on both dependency and self-criticism than non-depressed controls, the results of their study did not support Blatt’s original hypothesis that these two forms of depressive presentation represent stable personality traits, but rather represent a statedependent phenomenon. The authors also found a strong relationship between selfcriticism and severity of depression.
Attributional theories also report depressed mood is associated with greater self-criticism (Zahn, Lythe, Gethin, Green, Deakin, Young and Moll 2015; Brewin and Furnham 1987). Metaanalyses demonstrated a moderate relationship between of attributional style and current depressive symptoms, with participants reporting more internal, stable, global attributions for hypothetical negative events (Huang, 2015; Hu, Zhang and Yang, 2015; Sweeney, Anderson and Bailey, 1986).
However, some researchers argue that self-criticism has been shown to be both a prospective (Brewin and Firth-Cozens, 1997; Zuroff, Igreja and Mongrain, 1990) and concurrent vulnerability factor in depression (Hartlage, Arduino and Alloy, 1998). There is also evidence from the attachment literature that the origins of self-criticism lie in childhood and is particularly associated with maternal coldness and insecure attachment (Thompson and Zuroff, 1999) and that children who experience their parents as very restrictive and rejecting are more prone to being self-critical (Koestner, Zuroff and Powers, 1991).
Within the evolutionary perspective the origins of self-criticism are formulated in the context of social rank theory (Gilbert, 1992) in which parent and child interactions are viewed as hierarchical power relations. In this context specific attention is paid to a person’s early experiences of threat and subordination within the family. Thus, a child who fears their own parents, is driven to deescalate the aggression and hostility of the dominant parent(s) and is therefore forced into an involuntary subordinate role within the family. Often in this context the standard defensive strategies of fighting or fleeing are impossible and therefore the child, in the face of repeated criticism or threat, develops submissive behaviours as a defensive strategy (Irons, Gilbert, Baldwin, Baccus and Palmer, 2006). Such behaviours include, inhibited assertive behaviour, appeasement of others, avoidance, passivity, desire to escape, reluctance to initiate and lower positive affect and are strongly associated with depression (Gilbert and irons, 2005; Gilbert, Allan and Goss, 1996).
Defining compassion and self-compassion
In this section of the literature review there will first be a summary of the literature on defining compassion followed by a discussion of the definition of self-compassion.
The concept of compassion is most widely associated with Buddhism and Gu, Cavanagh, Baer and Strauss, (2017) cite the Buddhist definition of compassion as:
‘the heart that trembles in the face of suffering’
(Gu, Cavanagh, Baer and Strauss, 2017 p 2).
Further, Strauss, Lever-Taylor, Gu, Kuyken, Baer, Jones and Cavanagh, (2016) observe that all major world religions hold the concept of compassion as a central tenant of faith. There is much debate and even controversy in the literature over the definition of compassion and since the commencement of this PhD study in 2012 the field of compassion research has burgeoned (Gilbert, 2017a; Gilbert, 2017b, Strauss, Lever-Taylor, Gu, Kuyken, et al 2016; Catarino, Gilbert, McEwan, and Baiao, 2014;). Traditionally the academic literature has explored and studied the concept of compassion for others and it is only in the last eighteen years that attention has turned towards the study of self-compassion (Gilbert, 2017a; Muris and Petrocchi, 2017; Neff and Germer, 2013; MacBeth, and Gumley, 2012; Gilbert, McEwan,
Matos and Rivis, 2011; Goetz, Keltner and Simon-Thomas, 2010; Germer, 2009; Neff, 2003a).
Researchers seeking to define compassion across history tend to begin with ancient Greek philosophy, notably Aristotle and Darwin and examine the constructs of empathy, sympathy, pity, love and kindness as studied in the emotion research, as well as social and evolutionary psychology literature. There is a paucity of research literature regarding compassion prior to the new millennium and most studies are theoretical accounts that are not supported by robust research evidence. The relative merits of these constructs are both debated and contested (see Gilbert, 2017a; Strauss, Lever-Taylor, Gu, Kuyken, Baer et al 2016; Goetz, Keltner and Simon-Thomas, 2010 for further discussion of the constructs of empathy, sympathy, pity, love and kindness with regard to attempts to define compassion). Whilst some researchers would argue compassion is a blend of all these constructs (i.e. Sprecher and Fehr, 2005), others hold that compassion is simultaneously associated and yet different to each alone (Davis, 1983) and in combination (Neff 2003a). This debate continues (Gilbert, 2017b; Strauss, Lever-Taylor, Gu, Kuyken, Baer et al 2016).
A useful historical summary of definitions of compassion is provided by Strauss, Lever-Taylor, Gu, Kuyken, Baer et al, (2016). These are:
From the emotion literature: Lazarus (1991):
‘being moved by another’s suffering and wanting to help’
(Strauss, Lever-Taylor, Gu, Kuyken, Baer et al 2016 p 16)
Dali Lama (1995):
‘an openness to the suffering of others with a commitment to relive it’ (Strauss, Lever-Taylor, Gu, Kuyken, Baer et al 2016 p 17)
Wispe (1991):
‘being aware of and moved by suffering and wanting to help, with the ability to adopt a nonjudgemental stance towards others and to tolerate ones’ own distress when faced with other
people’s suffering’
Strauss, Lever-Taylor, Gu, Kuyken, Baer et al 2016 p 17).
Feldman and Kuyken (2011):
‘an orientation of mind that recognises pain and the universality of pain in human experience and the capacity to meet that pain with kindness, empathy, equanimity and
patience’
Strauss, Lever-Taylor, Gu, Kuyken, Baer et al 2016 p 17).
As can be observed from all these definitions suffering and its alleviation is a common thread. This is unsurprising given the concept of compassion arises from the Buddhist tradition which embodies the principle of the alleviation of suffering, with compassion as the vehicle for this.
Gilbert (2017a) continues explicating the controversy by observing that definitions of compassion are embedded in a cultural context and as a result the Eastern definition of compassion differs markedly from those used in Western culture (Gilbert, 2017a). Compassion in Eastern cultures originates from the Buddhist tradition and is associated with the concept of loving kindness (termed ‘metta’ in the Buddhism). Compassion is an aspect of loving kindness which, as Gilbert (2017a; 2005a; Gilbert and Choden 2013) define it involves:
‘being sensitive to suffering in self and others with commitment to try and alleviate and
prevent it’
(Gilbert and Choden, 2013 p. xviii)
This asks the individual to be open to, and to seek to alleviate, the suffering of self and others in a non-defensive, non-judgmental way (Gilbert, 2005a).
Gilbert (2017a) observes that in this Eastern tradition ‘metta’ refers to a disposition of open heartedness or friendliness whereas in Western definitions of compassion ‘metta’ is frequently translated as ‘love’ which, in the West, is conceptualised in terms of ‘liking, trust and affection’ (Gilbert, 2017a p 9). Gilbert (2017a) continues by noting that this Western interpretation of ‘metta’ fails to capture the essential essence of compassion within the Eastern definition, namely the necessity to have the courage to hold compassion for people we do not know or like or trust. Strauss, Lever-Taylor, Gu, Kuyken, et al (2016) add to this distinction by observing that in the Buddhist tradition compassion is not solely defined as an emotional response but as a disposition which conveys reason and wisdom and which is founded in an ethical system which embodies ‘the selfless intention of freeing others from suffering’ (Strauss, Lever-Taylor, Gu, Kuyken, et al 2016 p 17.)
Kirkby, (2017) cites the definition of compassion proposed by Geshe Thupten Jinpa who devised the Stanford Compassion Cultivation Training programme. Firmly founded in Buddhist philosophy and practices he defines compassion as a complex, multidimensional construct consisting of four components, as follows:
-
A cognitive component -awareness of suffering
-
An affective component – sympathetic concern related to being moved by suffering
-
An intentional component -a desire to see the relief of suffering
-
A motivational component -a responsiveness or readiness to help alleviate suffering
(Kirby, 2017, p 433).
Strauss, Lever-Taylor, Gu, Kuyken, et al (2016 p 19) propose a five-element definition of compassion as follows:
1. Recognition of suffering
2. Understanding the universality of suffering in human experience
3. Feeling empathy for the person suffering and connecting with the distress (emotional resonance)
4. Tolerating uncomfortable feelings aroused in response to the suffering person (e.g.
distress, anger, fear) and so remaining open to and accepting of the person suffering
5. Motivation to act/acting to alleviate suffering.
This is an atheoretical definition which seeks to build bridges between differing compassion theories. The motivation behind their work being a call for a consensus to be arrived at regarding the definition of compassion, in order to achieve their stated aim, to develop valid and reliable psychometric measures to further advance the conceptual and clinical understanding of compassion.
An evolutionary formulation of compassion
In the last ten years evolutionary formulations of compassion have emerged, based on Darwinian principles (Gilbert, 2017b; Gu, Cavanagh, Baer and Strauss, 2017; Goetz, Keltner and Simon-Thomas 2010) in which compassion is conceptualised as an innate human capacity which serves the purpose of enabling a reproductive advantage because of the role it plays in the care giving system (Gu, Cavanagh, Baer and Strauss, 2017). However, even within this evolutionary frame compassion is conceptualised in differing ways. These are summarised below.
Compassion as an appraisal elicited emotion
Goetz, Keltner and Simon-Thomas (2010) in their comprehensive empirical review define compassion as an emotion as follows:
‘the feeling that arises in witnessing another’s suffering and that motivates a subsequent
desire to help’
(Goetz, Keltner and Simon-Thomas 2010 p. 351)
They delineate three forms of compassion as an emotion, which, when studied, can be categorised according to the different levels of analysis used in emotion research. Firstly, compassion as a distinct emotion, which is defined as being ‘brief, context specific responses focused on a clear cause’. Secondly, compassion as ‘an analysis of moods or sentiments’ which are considered to be longer lasting, less focused on a specific cause and less context dependent. Finally, compassion as ‘emotional traits’ which are defined as ‘general styles of emotional responses that persist across context and time’ (Goetz, Keltner and Simon-Thomas, 2010, p 353).
As illustrated in the definition of shame section of this literature review, in the emotion literature individual emotions are studied and delineated by defining the following components; antecedent appraisal processes, nonverbal display signals, the description of the experience of the emotion itself and its associated physiological responses. In their account of compassion as a distinct emotion, Goetz, Keltner and Simon-Thomas, (2010) draw on a vast array of research from anthropology and evolutionary and social psychology to support the presence of these components as part of an evolutionary formulation of compassion as an emotion in its own right. The authors cite three reasons why compassion would emerge as part of a survival strategy. These are: the capacity for compassion to enhance the welfare of vulnerable offspring, to assist in mate selection and to facilitate cooperation with non-kin, all of which increase the likelihood of genes being replicated. This perspective can be briefly summarised as follows.
At birth humans are extremely vulnerable and survival requires intensive and sustained nurture and care in order to reach an age where a child is not only able to survive independently but reproduce. The evolutionary literature cites several adaptations which serve the function of maximising parental engagement in this care giving activity so essential to survival. These include distress vocalisation, skin-to-skin contact, attachment related behaviours and the emotion of compassion, which involves reciprocal attunement between care giver and offspring aimed at reducing harm and suffering in the vulnerable offspring. These care giving behaviours are universally observed across both preindustrial and industrial societies and different cultures and among primates most closely related to humans, chimpanzees and bonobos (Goetz, Keltner and Simon-Thomas 2010). These adaptations are articulated more fully in Gilberts’ evolutionary accounts of shame (Gilbert, 2007a) (as discussed in the shame section of this chapter) and compassion (Gilbert, 2017b) which is discussed more fully below. For Gilbert, the elicitation of care (and not just protection) as part of these adaptations is central to his theories of shame and compassion and their interrelationship.
In the evolutionary model sexual selection theory holds that processes exist in humans whereby certain traits are selected for as indicated by the preferences males and females show in mate selection. In this context, Goetz and colleagues (2010) argue that compassion needs to be considered in terms of a trait like phenomenon in which humans experience the emotion of compassion which enables secure attachment, creates strong intimate bonds and enhances altruistic behaviour. The survival advantage of selecting a mate who displays high levels of compassion includes, an increased access to resources for vulnerable offspring, the provision of a greater degree of physical care i.e. protection, affection and touch and the creation of more co-operative and affiliative communities.
Finally, in considering in evolutionary terms, the concept that compassion promotes cooperation between non kin, it is posited that compassion evolved as part of a system of emotions that facilitate non kin cooperation in order to develop, maintain and regulate mutual and reciprocally beneficial altruistic relationship. This in turn promotes altruism in a societal context in the form of cultural norms, values and behaviours that reward altruism and punish selfishness. Thus, compassion serves the function of an internal motivation and reward for following norms which establish cooperation. Therefore, individuals will prefer long-term relationships with more compassionate others because (when considering compassion as an emotional trait) this will increase cooperation and engender greater degrees of trust, which in turn, will facilitate mutually beneficial interactions between people where there is no kin bond (Goetz, Keltner and Simon-Thomas 2010).
Goetz and colleagues elaborate their model of compassion as an emotion in the three forms described above by stating a perquisite to the elicitation of the emotion of compassion are specific appraisals unique to compassion and distinct from distress, sadness or love. This is summarised in appendix V. Whilst conceding no single research study to date has delineated the entire appraisal pattern associated with compassion, they draw together research from evolutionary and social psychology to make a case for compassion related appraisals. In summary the authors propose that a specific compassion related appraisal pattern can be identified, triggered by witnessing the suffering of others, which they argue is a powerful elicitor of the emotion of compassion. This elicitation is, they suggest, mediated by appraisals related to self-relevance, goal congruence, blame and coping ability, which they integrate with the evolutionary concept of cost-benefit analyses which may enhance or inhibit the elicitation of compassion.(Goetz, Keltner and Simon-Thomas, 2010).
Compassion as a motivational system
In his definition of compassion Gilbert (2017a; 2005b) draws on the same evolutionary principles as Goetz and her colleagues (Goetz, Keltner and Simon-Thomas 2010) but argues strongly that compassion is more than an affective state. Rather, Gilbert argues, compassion has emerged as an evolved motive within the care giving social mentality, as part of human social intelligence. This care giving social mentality is explicated more fully in the shame section in this chapter. In summary Gilbert (2017a) attests that innate to humans are the evolved competencies for what he terms ‘knowing awareness and deliberation’ (his italics), that is, as humans we have the capacity not only to feel, but to know we are feeling and what we are feeling. Similarly, we have the capacity not simply to act but to know what we are doing and why we are doing it i.e. we act with intentions (Gilbert, 2017b p 32). Thus, we have the capacity to plan and reason, to focus our attention and to be aware of our own cognitive and emotional reactions. Humans have, as part of the caring social mentality, also evolved the capacity to have empathy for others and to understand that others have emotions, beliefs, intentions and knowledge and to hold a sense of self in the mind of the other (theory of mind) and a capacity for shared experience and understanding (intersubjectivity) (Gilbert, 2017b p 33). Consequently, humans possess the capacity to be aware of suffering in the world and an innate drive to meet needs in self and others and to work to prevent and alleviate suffering and not to be a cause of suffering. Importantly however, for Gilbert these capacities can be deployed for good or ill and thus all humans possess a capacity to deliberately inflict cruelty and suffering as well as to show kindness and offer help not only to others, but to self.
Thus, for Gilbert compassion arises from the caring social mentality and involves both motives and intentions. For Gilbert, evolved motives have a very specific definition. They actively direct behaviour by triggering physiological processes that focus attention, generate emotion and activate cognitive processes with the aim of stimulating motive appropriate behaviour. The aim being to meet biosocial goals that include not only survival and reproduction but where to focus attention, what to be emotionally attuned to and aroused by and what is referred to in animal biology as choregraphed behaviour (Gilbert, 2017b p 39). In animal biology choregraphed behaviour refers to the pairing of specific bodily gestures and vocalisations which creates a signal to another that is more complex than each element alone. The purpose of this being not just communication but the eliciting of a response that creates an interaction (i.e. sexual displays leading to procreation). Gilbert extrapolates from this and articulates the idea that our evolved motives direct our behaviour in terms of how we think and organise our lives and what gives us a sense of meaning and purpose and identity. Importantly, for Gilbert these innate motives take primacy over emotions. Thus, compassion as a motive guides us to understand what to care about, when this care needs to be demonstrated and what action we need to take to demonstrate not only the behavioural act of care giving but, conveying through intersubjectivity, the fact we care. Crucially these social mentalities influence not only our own minds, but function to influence the minds of others.
To quote Gilbert:
‘social mentalities are working to create conditions in the minds of others conducive to their
own strategic functioning and survival’
(Gilbert 2017b p 41).
Further, these motives, embedded in an evolved brain which utilises these socially intelligent competencies will give rise to choreographed behavioural responses (Gilbert terms these interpersonal dances, Gilbert, 2017b; 2005b) not just at an individual but at the level of group (i.e. family, profession, religion, creed and the like), culture and sub-culture, society and nation. Social mentalities have, what Gilbert terms, ‘a flow’ by which he means our social behaviour is enacted through these interpersonal dances (choregraphed behaviour). Thus, individuals, using their social intelligence competencies, send and respond to each other’s signals in line with the social roles being co-created. These serve the function of promoting survival by reducing harm, enabling in-group-out group identities and sense of belonging and influencing access to resources and their allocation.
Gilbert terms this process ‘compassion flow’ (Gilbert, 2017a) and describes this in terms of the compassion we feel for others, our responsiveness to compassion from others and our capacity to be self-compassionate, mediated by any given social context which may enable, enhance or block this flow (Gilbert, 2017b p 44). Of fundamental importance here is the reciprocal nature of this relationship in that the social mentality of compassion requires both competencies for giving and receiving compassion.
As stated earlier in this chapter Gilbert’s purpose in his work is to design psychotherapies that cultivate and use compassion motives to alleviate suffering (i.e. emotional distress) in the fields of both physical and mental health. Thus, Gilbert has over the last decade developed and honed his Compassion Focused Therapy (CFT) (Gilbert and Choden, 2013; Gilbert, 2010a; Gilbert, 2009; Gilbert, 2007b; Gilbert and Procter, 2006; Gilbert and Irons, 2005) underpinned by this comprehensive theoretical model derived from evolutionary and social psychology. Therefore, in summary, all evolved motives have two elements, stimulus detection and appropriate action. In Gilbert’s CFT model these are: motivated sensitivity to, appraisal of and engagement with signals of suffering in self and others and motivated action to try and alleviate and prevent it and the motivation to acquire wisdom for skilled action. Whilst observing there is no agreement regarding which social competencies are enshrined within the compassion motivational system and that competencies may be shared across different motivational systems, in the CFT model Gilbert posits six competencies for engagement with suffering and six competencies for alleviation and prevention of suffering, from which arises compassion for others and self-compassion. These are in terms of engagement with suffering: sensitivity, sympathy, empathy, distress tolerance, non-judgement and care for wellbeing and for the alleviation and prevention of suffering attention, feeling, imagery, sensory, reasoning and behaviour (Gilbert, 2017a p 52).
In presenting an integrated account of compassion in the context of his evolutionary biopsychosocial model of shame Gilbert offers an account of compassion motivations and makes a distinction between submissive shame and genuine shame, arguing that submissive shame is associated with depression, anxiety and stress (Catarino, Gilbert, McEwan and Baiao (2014). Drawing on the evolutionary theory of compassion described above, the authors elaborate this distinction between genuine compassion, where the motives driving the behaviour is to support the wellbeing of others and submissive compassion, which is more linked to being liked, pleasing others, a desire to be seen as good in the eyes of others and avoidance of rejection. They continue by observing, through the evolutionary lens, that whilst people may consciously use caring behaviours to gain support from others, some individuals, (i.e. those concerned with a fear of rejection or with childhoods in which they prioritised the needs of others over their own) may consciously engage in submissive and appeasing behaviour. In this evolutionary frame submissive behaviours are associated with lower social rank and involve inhibition of the individuals own hostile feelings, difficulty asserting or in some instances recognising one’s own and needs, rights and preferences and a drive to appease others in order to reduce threat from them (Catarino, Gilbert, McEwan and Baiao 2014; Gilbert and Allan, 1994).Gilbert’s earlier research, (Gilbert, 2000) offers evidence to support links between social rank, shame and depression and this can be contrasted with research evidence that compassion and compassion training may enhance wellbeing, coping and social connectedness (Catarino, Gilbert, McEwan and Baiao 2014; MacBeth and Gumley, 2012).
This distinction between genuine and submissive compassion carries clinical cogency. The clinical experience of the author of this PhD thesis echoes this view. People experiencing persistent, treatment resistant depression not only see themselves as of lower status to others, but often display in therapy the submissive behaviours as observed by Catarino and colleagues (Catarino, Gilbert, McEwan and Baiao 2014). These include avoidance of eye contact, not starting a discussion, not expressing feelings of anger, not expressing views or opinions, often having no real sense of what their own rights, needs and wants are and always agreeing with the clinician. In addition, this submissive behaviour usually generalises to all their relationships and interactions with others and is often amplified in a social context that may be even more threat focused than a therapy session.
Definition of self-compassion
The leading exponent of self-compassion is Neff (Neff and Vonk, 2009; Neff, Kirkpatrick and Rude, 2007; Neff, 2004; Neff, 2003a) and it is a psychometric measure the Self Compassion Scale (SCS) developed by her (Neff, Whitaker and Karl, 2017; Neff, 2016a; Neff, 2003b) that is tested as part of this PhD study.
As Neff has developed her self-compassion theory, she has offered varying definitions of selfcompassion as follows:
‘being touched by and open to one’s own suffering, not avoiding or disconnecting from it, generating the desire to alleviate one’s suffering and to heal oneself with kindness. Self-
compassion also involves offering non-judgmental understanding to one’s pain, inadequacies and failures, so that one’s experience is seen as part of the larger human experience’.
(Neff, 2003a p.87)
“involves being caring and compassionate toward oneself in the face of hardship or perceived inadequacy ... having the right amount of distance from one’s emotions so that they are fully experienced while being approached with mindful objectivity”
(Neff, Kirkpatrick, & Rude, 2007, p. 140).
Leary, Tate, Adams, Batts-Allen and Hancock (2007) hypothesise that individuals with high levels of self-compassion view their weaknesses and shortcomings accurately but interact with these with kindness and compassion as opposed to self-criticism and harshness. Thus, they argue the capacity for self-compassion may offer protection from negative life events and activate positive feelings in the face of things going wrong.
Neff (2003a) identifies self-compassion as having three interrelated paired facets that can be exhibited at times of emotional distress or failure. Each set of paired facets is defined as dichotomous, whereby, the presence of one element, by definition, leads to the absence of the other.
These three facets are:
1. Being kind and understanding towards self rather than self-critical
2. Seeing one’s own fallibility as part of the human condition rather than as something that marks one as ‘the only one’ and therefore isolating.
3. Having the capacity to hold one’s painful thoughts and feelings in mindful awareness rather than either over identifying with them or avoiding them.
Barnard and Curry (2011) elaborate each of these facets with reference to relevant research literature using three categorisations:
-
Self-kindness versus self-judgement
-
Common humanity versus isolation
-
Mindfulness versus over identification or avoidance
Further consideration will now be given to each of these in turn.
Self-kindness versus self-judgment
Barnard and Curry (2011) draw on the work of Neff (2004; 2003a) and Gilbert and Irons (2005) to define self-kindness as:
‘Self-kindness involves extending forgiveness, empathy, sensitivity, warmth and patience to all aspects of oneself, including all of ones’ actions, feelings, thoughts and impulses’
(Barnard and Curry, 2011, p 290).
They continue by identifying an important corollary to this self-view namely, that the individual perceives themselves to have worth per se, that this is unconditional and that intrinsically one deserves love, happiness and affection, even in the face of failure.
They contrast this definition with what is described as self-judgement in which one is hostile, demeaning, and critical of self and/or aspects of self. As such people who are self-judgmental tend to reject their own, thoughts, feelings, impulses, actions and there is conditionality attached to worth. They observe that self-judgement may be so intrinsic to the individual that it is beyond the scope of their awareness and the person concerned may not realise the deleterious effect it has on their health and well-being.
Thus, Gilbert and Irons (2005) argue becoming aware of one’s self-judgement (which Gilbert usually labels as self-criticism or self-attack) is necessary in order to develop self-kindness.
Common humanity versus isolation
A key principle within Buddhism is that all living creatures are intimately connected. Further it is argued all humans long for connectedness and to see oneself as separate from others is a falsehood. As described earlier in this chapter, this concept of the evolutionary drive for connectedness among humans is a central tenant of Gilbert’s psychobiosocial model of shame and his Compassion Focused Therapy. Gilbert (2017a; 2007a; 2005; Gilbert and Choden, 2013; Gilbert and Proctor 2006) draws on extensive research from biology, anthropology and evolutionary psychology to support his theory that humans are genetically predisposed to operate and co-operate in affiliative groups and that our attachments are a necessity not only to ensure survival but to give us a sense of well-being and belonging.
In this context common humanity involves acknowledging our ongoing connection to others and the recognition that our sadness and suffering, hopes and wishes, faults and weaknesses are part of a shared experience of being humans. Thus, common humanity involves selfforgiveness for being human i.e. as Neff observes ‘being limited and imperfect’ (Neff, 2003a p 87).
The dichotomous position in this construct is isolation, defined in terms of the idea that at times of sorrow and failure the person feels cut off from others. Further, at such times, if sense of self is experienced as failing and emotions as weak then the individual may withdraw from others and feel alone and left to struggle with their distress. As Gilbert’s clinical observation encapsulates the person in a state of arrested flight (defeat and depression) has a sense of self and self-in-relation to others as ‘alone, abandoned and no one cares’ (Gilbert, 2010a).
Mindfulness versus over identification or avoidance
Mindfulness involves awareness of, attention to and acceptance of the present moment.
Kabat-Zinn (2003) describes two components to mindfulness:
1. Cognitive attention to and affectionate, friendly interest in one’s present experience
2. The capacity to observe and label thoughts and feelings rather than reacting to them and to do so without self-judgement
Barnard and Curry (2011) observe two factors which it is believed impede the taking of a mindful position, namely over identification and avoidance.
Over identification refers to a tendency to ruminate on one’s limitations and failings.
Cognitive science identifies rumination as a maintenance factor in depression (Spasojevic, and Alloy, 2001; Nolen- Hoeksema, 2000) and Mindfulness Based Cognitive Therapy (MBCT)
(Kuyken, Byford, Taylor, Watkins, Holden, White, Barrett, Byng, Evans, Mullan, and Teasdale,2008; Ma and Teasdale,2004; Teasdale, Moore, Hayhurst, Pope, Williams and Segal, 2002) aims to actively interrupt rumination as a means of seeking to alleviate depressed mood by promoting a mindful position towards painful thoughts and feelings.
In summarising their assessment of Neff’s proposed model of self-compassion Barnard and Curry (2011) observed that self-compassion was a relatively new field and there was very little research investigating the inter-relationship between these three facets of self-compassion as defined by Neff (Neff, 2003a, 2003b). Barnard and Curry (2011) hypothesised that each facet needs to be present for self-compassion to emerge and that each facet both fosters and strengthens the others, to lead to a position where the whole is greater than the sum of its parts. Barnard and Curry (2011) called for further empirical research and intervention studies to examine the dichotomous relationship between the paired facets operate as proposed by Neff (Neff, 2003a; 2003b) and to test whether an increase one component i.e. self-kindness leads to a concomitant decrease in the other i.e. self-judgement and so with the other pairings (common humanity vs. isolation and mindfulness vs. overidentification).
Since the commencement of this PhD study, research literature has emerged which has critiqued both Neff’s theory of self-compassion (Neff, 2003a) and the Self Compassion Scale (SCS) (Neff, 2003b) on several fronts. Neff developed the scale using two student samples (Neff, 2003b) and much of this criticism has emerged from research that has used the measure on clinical samples. This body of research has questioned the factor structure of the scale (Costa, Marôco, Pinto-Gouveia, Ferreira, and Castilho, 2016; Williams, Dalgleish, Karl and Kuyken, 2014); whether self-compassion as defined by Neff as six factors can be assessed using its overall score (Kumlander, Lahtinen, Turunen and Salmivalli, 2018; Pfattheicher, Geiger, Hartung, Weiss and Schlinder 2017; Brenner, Heath, Vogel, and Credé, 2017; López, Sanderman, Smink, Zhang, van Sonderen, Ranchor, and Schroevers 2015) and whether negative items on the scale should be excluded as they in fact measure the personality trait of neuroticism (Geiger, Pfattheicher, Hartung, Weiss, Schindler and Wilhem, 2018; Pfattheicher, Geiger, Hartung, Weiss and Schlinder 2017) Neff has robustly defended this criticism (Neff, Toth-Kiraly and Colosimo, 2018; Neff, Whitaker and Karl 2017; Neff, 2016a; 2016b).This critique will be analysed and pursued in greater depth in the discussion chapter of this thesis.
There is debate in the literature as to whether parallels can be drawn between compassion and self-compassion. Studies examining the correlation between self-compassion and compassion for others found no correlation in a cohort of undergraduates and only weak correlation in a community sample and sample of meditation practitioners (Neff and Pommier 2013).
Buddhists argue that making a distinction between compassion and self-compassion is not only false, but that, in order to have compassion for others the individual must first have selfcompassion (Strauss, Lever-Taylor, Gu, Kuyken, et al 2016). Gilbert (2017a) explicates this point in more depth, makes a distinction between the compassionate self in comparison to self-compassion. He describes the compassionate self as being an aspect of self-identity which is rooted in intention and motivation which organises the mind with the aim of developing what he terms ‘wisdom and insights.’ (Gilbert, 2017a p 46). He explicates this further by defining wisdom and insights in the context of the principles of his CFT model and describes this mind state as ‘integrated’ in contrast to the threat-based processing which he describes as ‘disintegrated or segregated’ (Gilbert, 2017a p 46). Thus, the ‘integrated mind state’ of the compassionate self is associated with organisation of the frontal cortex of the brain to promote caring behaviours and empathy-based insights and inhibit impulsivity. Gilbert argues that only when we develop the competencies associated with the compassionate self can we be open to compassion for others, to receive compassion and develop the wisdom for selfcompassion (Gilbert, 2017a).
Overall, as several authors observe, further study is required regarding the association between compassion and self-compassion. As yet, it is unclear whether this seeming lack of association is due to real independence between the two constructs (Strauss, Lever-Taylor, Gu, Kuyken, et al 2016). Other explanations could be poor definition of the constructs, the weakness of correlational study design or limitations of measures of compassion and selfcompassion (Williams, Dalgleish, Karl and Kuyken, 2014).
Examining the Practicality of these theories of shame using Brawley’s criteria
A theory that is not testable is of limited utility in addressing health problems. Equally until a theory has been tested and its strengths and weaknesses examined it remains just that, a theory, and its Practicality to shape clinical practice remains unknown. The shame literature is diverse and emotion theorists (e.g. Tracy and Robins 2007a) observe that the study of selfconscious emotions is still in its infancy. Appendices VI presents an assessment of the shame theories reviewed here, measured against Brawley’s six criteria, that for him define the Practicality of a theory. In reviewing this literature, it seems apparent that there is a lack of theoretical consensus regarding the definition of shame, self-criticism and self-compassion and there is only limited evidence that these theories have been tested on clinical populations or translated into clinical interventions that have been tested for their effectiveness.
The first three shame theories reviewed (Tangney 1995; Tangney and Dearing 2002; Lewis 2000; 2007; Tracy and Robins 2007a; 2006; 2004) are all interconnected in that, taken chronologically, in accordance with their emergence in the literature, each is a revision or refinement of the previous theory. They all share the premise that shame as an emotion is elicited by cognitive processes, each theory in turn articulating an ever increasingly complex explanatory model. Tangney and colleagues, (Tangney, Dearing, Wagner and Gramzow, (2000); Tangney, (1990)) have developed the Test of Self-conscious Affect-3 (TOSCA-3) as a psychometric measure, aimed at testing their theory and this measure is now in its third revision. This has also been used in studies conducted by Tracy and Robins (2006). All of these studies have been carried out on student populations and there are no data sets where it has been tested on clinical populations.
Lewis’s theory is the only shame theory directly derived from clinical observation specifically with children who have experienced sexual and/or physical abuse and/or neglect. Tangney and Dearing (2002) attempt to make clinical recommendations and whilst their formulation is primarily psychoanalytic in orientation, they do make reference to Beckian cognitive therapy (Beck, Rush, Shaw et al 1979) and a Rogerian person-centred approach (Rogers, 1979). However, their recommendations are somewhat broad brushstroke and lack any case examples to support their claims that utilising their theory of shame within any of these therapeutic methods will ameliorate the effects of shame. The authors observe:
‘as clients translate into words their preverbal, global shame reaction, they bring to bear a more logical, differentiated thought process that may compel them to spontaneously re-evaluate the global nature of the shame-eliciting episode’
(Tangney and Dearing, 2002, p 175)
In the same vein they suggest cognitive re-evaluations within a Beckian framework may be useful for addressing shame-inducing cognitions. In the clinical experience of the author of this thesis, when working with client’s who experience persistent, treatment resistant depression shame-based cognitive processes are extremely difficult to influence using standard Beckian cognitive interventions. Similarly, the spontaneous realignment of shamebased processing described in the above quote from Tangney and Dearing (2002) is a nonexistent phenomenon in the diagnostic group studied in this PhD thesis. Indeed, what has led the author to test Gilbert’s formulation of shame in a cohort of patients diagnosed with persistent, treatment resistant depression is, the clinical observation that, shame is an extremely painful and debilitating emotion and where shame is present psychotherapy is challenging for both patient and clinician. Indeed, Gilbert developed his theory of shame and its attendant clinical interventions in part from making the same clinical observation, that not only can Beckian interventions be of limited impact in ameliorating the effects of shame but their very use in therapy and the clients difficulty in utilising them can, in itself, induce shame.
In terms of assessing these three theories against Brawley’s criteria they are reasonably strong in relation to criteria 1, 2, and 5. In terms of criterion 3 there is a reliance on the TOSCA (Tangney, Dearing, Wagner and Gramzow, 2000), which is a psychometric measure of selfconscious emotions (this measure and its parameters are discussed more fully in chapter3 of this thesis). In terms of criterion 4 each theory draws on basic research from evolutionary biology, psychology and anthropology. This is especially the case in drawing the distinction between basic and self-conscious emotions. Lewis (2007; 2000) and Tracy and Robins (2007a; 2006) draw extensively on attributional theory and in addition, the latter utilise research from social-personality psychology in the study of self and emotions. In this regard these models draw extensively on existing related research data which furnishes the theories with some validity. The weakness in these theories is the lack of evidence for criterion 6. None of these theories have been tested on a clinical population in order to examine if they predict why an intervention might fail to produce change. The properties of the TOSCA have been tested in this way on a large body of student populations but not on a cohort of patients diagnosed with depression. (see Kim, Thibodeau and Dickerson, 2011 for a review of studies which have tested shame measures on a clinical population).
In contrast to these cognitive-attributional theories of emotion Gilbert 2007a; 2005) proposes an evolutionary and biopsychosocial theory of shame. For Gilbert Shame is a phylogenetic mechanism developed to regulate social rank. As such it operates as an involuntary submissive response triggered by social threat which functions to de-escalate conflict (Gilbert and McGuire 1998). Thus, importantly in contrast to previous theories, shame for Gilbert is not a product of cognitive attributional processes. However, Gilbert’s model does draw on the same evolutionary literature as Tangney and Dearing (2002); Lewis (2000) and Tracy and
Robins (2007; 2006; 2004). In addition, his theory also draws on theory of mind, self-conscious awareness and metacognition literature (see Gilbert, 2017a for the most comprehensive account to date of his theory of shame).
With regard to assessing Gilbert’s theory of shame against Brawley’s criteria it has strength in the fact that it has some validity across all six criteria. In particular the theory is robust in terms of criteria 1–4. The theory has been developed over more than two decades and is in a constant process of refinement. In reviewing the literature, it is possible to observe the various iterations of Gilberts, evolutionary psychobiosocial theory of shame (Gilbert, 2017a; 2016; 2010; 2007a; 2005a; 2005b; 2003; 2001; 1998) as clinicians, evolutionary psychologists and biologists and neuroscientists have collaborated in research with a range of foci (Gilbert and Choden, 2013; Gilbert, McEwan, Matos and Rivis, 2011; Gilbert and Procter, 2006; Lieberman, Gaunt, Gilbert and Trope, 2002; Gilbert and Allan, 1994; Gilbert and McGuire, 1998). There is a clearly articulated set of interconnected variables in Gilbert’s theory of shame (see Appendix VI) and the theory draws on a wealth of basic and applied research data from evolutionary biology (see Vrticka, Favre and Singer, 2017; Conway and Slavich, 2017; Gilbert, 2005b; Gilbert and McGuire, 1998 for useful summaries), psychology (Tracy and Robins, 2007a; Bierhoff, 2005; Tangney and Dearing, 2002; Kaufman, 1989; Nathanson, 1987) and anthropology (see Spikins, 2017; Greenwald and Harder, 1998; Lindisfarne, 1998 for informative perspectives).
Gilbert and colleagues have developed an interconnected set of psychometric measures aimed at measuring and testing the theoretical tenants of the model, two of which are tested in this PhD thesis. Are reviewed further in chapter 3).
In contrast to the other shame theories outlined here, Gilbert’s testing of his theory is in keeping with the Scientist-Practitioner model. Gilbert has a central aim of trying to make theory practice links and to use his proposed theory of shame to develop clinical interventions aimed at ameliorating the impact of shame in emotional disorders. A serious weakness the author would observe is that whilst Gilbert’s theory of shame is comprehensive and cogent in theoretical terms when this is translated into clinical practice there is a disconnect between the theory and the clinical interventions proposed by his theory. The clinical interventions have a degree of eclecticism that draws on psychoanalysis (specifically Jungian formulations); behaviour therapy, Gestalt therapy (the two and three chair technique is a key clinical intervention) and cognitive therapy (compassionate thought challenging) and Mindfulness. However, the theoretical principles underlying these individual interventions are not only diverse but are not readily identifiable in his overall theory of shame. To date only one small pilot study trial has been conducted (Gilbert and Procter 2006) to test the components of the theory and its attendant interventions. This was reported as promising results, but the cohort, who did not have a depression related diagnosis, was small (n=6).
A critique of Gilbert’s theory of shame
The clinical experience of the author of this PhD thesis would suggest Gilbert’s theory has face validity and is of relevance when seeking to formulate the role of shame, self-criticism and self-compassion in patients diagnosed with persistent, treatment resistant depression. However, this has never been tested in an RCT, on a large clinical sample of patients meeting these diagnostic criteria. Gilbert’s distinction between internal shame and external shame is a point of clinical interest. Gilbert is unique in his conceptualisation of a theory of shame that attributes emotional disorders as being linked only to external shame, viewing internal shame (which is formulated as self-criticism or self-attack) as a by-product of external shame in the form of a defensive submissive strategy, aimed at appeasing a dominant other and keeping oneself safe. The definitions and parameters of the internal shame are less well defined in Gilbert’s theory. Gilbert, Clarke, Hempel, Miles and Irons (2004) explored forms, styles and reasons for self-criticism using a cohort of 246 female undergraduate psychology students with a mean age of 27.7. In their conclusions the authors identify two forms of self-criticism, one they term ‘self-correction’ and a second ‘self-hating’ and hypothesise potential relationships between these, suggesting self-hating based self-criticism may be more strongly associated with depression. However, they acknowledge at the time the paper was written more research was required to understand the form and functions of self-criticism in depression. A further study, (Gilbert, Durrant and McKewan, 2006).
In the intervening time period (2006 to date) Gilbert has turned his research attention towards self-kindness and self-compassion and has investigated its utility in generating selfwarmth (Gilbert, Baldwin, Irons, Baccus, Jodene and Palmer 2006; Gilbert, McEwan, Mitra, Franks, Richter and Rockliff, 2008) as a means of counteracting the effects of self-criticism and therefore depression and anxiety. Once more these studies have been conducted on student samples.
Since the commencement of this PhD study the clinical interventions which emerged from Gilberts theory CFT (Gilbert, 2014; 2010b) have been tested on a range of clinical and nonclinical groups. A systematic review conducted by Leaviss and Uttley, (2015) identified 3 studies which had evaluated CFT and 2 a combination of CFT and CBT, (out of a total of 14 studies). These were uncontrolled studies conducted in clinical services and none were conducted on a patient cohort diagnosed with persistent, treatment resistant depression. In a second systematic review, Kirby, (2017) cites four RCT’s of CFT, one in the treatment of schizophrenia and one in smoking cessation, one in binge eating disorder and one on a community sample. It is unclear from this literature how much fidelity to the CFT intervention protocol designed by Gilbert and colleagues (Gilbert, 2014; 2010a; Gilbert and Choden, 2013) and its underlying treatment rationale these studies demonstrate. Thus, the literature review undertaken as part of this PhD thesis has not identified any studies which specifically examine Gilbert’s theory of shame and the relationship between shame and self-criticism and selfcompassion in a cohort of patients diagnosed with persistent, treatment resistant depression.
Kim, Thibodeau and Jorgensen (2011) conducted a meta-analytic review with the aim of providing the first quantitative summary of the magnitude of association of shame and guilt with depressive symptom severity. In their summary of findings, they concluded that virtually all of the 101 studies and seven sets of unpublished data they included in the review, used unselected samples of participants whose depressive symptoms were at worst rated at a moderate level of depression. The authors included in their meta-analytic review four studies that recruited a clinical example but the primary focus of investigation in these studies was guilt not shame.
These limitations highlighted by Kim, Thibodeau and Jorgensen (2011) are exemplified by two of Gilberts studies, Cheung, Gilbert and Irons (2002) and Gilbert (2000). Cheung, Gilbert and Irons (2002) examined the associations between social rank (defined in terms of submissive behaviour and social comparison) and shame, rumination and depression. The study findings found that social rank and shame and depression are highly related. However, the study sample was 125 undergraduate students which limits the generalisability of these results to a clinical population. A further area of concern is the epidemiology of the sample. This sample, using university undergraduates is biased in favour of a demographic of young, white, middle class females. In the Cheung, Gilbert and Irons (2002) 69 females with a mean age 0f 21.6 were recruited and 56 males with a mean age of 23.59. In the Gilbert (2000), two samples were recruited, a student sample and a clinical sample. The student sample consisted of 96 females and 13 males with a mean age of 25. There is no reference in either paper to the ethnic breakdown of the cohorts or the socioeconomic status of the participants. Once more this type of bias in sampling limits the conclusions that can be drawn from the research and its generalisability to a clinical setting.
In addition, in the study published in 2000, Gilbert (Gilbert, 2000) explored the relationship between shame, depression and social anxiety from the perspective of social rank theory. Social rank theory argues that mood states are significantly influenced by where one perceives oneself to be in a social rank i.e. the extent to which a person feels inferior to and looked down on by others. As a result, behaviour becomes submissive. Gilbert formulates shame, social anxiety and depression as defensive submissive strategies when a person finds themselves in a position of low rank which is unwanted. In this study Gilbert recruited two participant groups, 109 undergraduate psychology students and 50 depressed in-patients with a mean BDI score (Beck, Ward, Mendelsohn, Mock and Erbaugh 1961) score of 28.5, indicative of a severe level of depression within the parameters of this measure. Each group completed a battery of measures relevant to the constructs under investigation. In terms of the outcome of the study Gilbert reports that shame, social anxiety and depression (but not guilt) are highly related to feeling inferior and submissive behaviour.
Gilbert’s research highlights several challenges in the study of shame, (and to a lesser extent self-criticism and self-compassion) in relation to depression. Firstly, there is a lack of consensus over the definition of shame and as a result how shame is formulated varies between researchers. Indeed, some contributors to the literature use ill-defined definitions of shame that do not have a theoretically informed conceptualisation. For example, one of the measures used by Gilbert in his 2000 study, the PFQ-2 (Harder and Zalma 1990) does not utilise any theoretically derived definitions of shame. Kim, Thibodeau and Jorgensen (2011) in their meta-analytic review argue that using scales such as the PFQ-2, which are conceptually ambiguous, may lead to a blurring of the distinction of associations between shame and depressive symptoms leading to the generation of research data of questionable quality.
In reviewing the literature some researchers formulate shame and guilt as different sides of the same coin (Tracy and Robins 2004); others related but distinct constructs (Tangney and
Dearing 2002) and uniquely to Gilbert (2017a; 2007a; 2005b) as unrelated constructs. As Kim, Thibodeau and Jorgensen (2011) identify, there is a wealth of theory describing the strength of association between shame and its relationship to other constructs such as depression but a lack of empirical data to support the theory.
This lack of consensus over the definition of shame is reflected in the range of psychometric measures purporting to measure shame as a construct. Kim, Thibodeau and Jorgensen (2011) observe that several of the most commonly used measures of shame measure the construct in a generalised way. This is highlighted by the three measures of shame used in the Gilbert
(2000) study. The measures were: the Test of Self-conscious Affect (TOSCA) (Tangney,
Dearing, Wagner and Gramzow 2000); The Personal Feelings Questionnaire 2 (PFQ-2) (Harder
and Zalma, 1990) and the Others as Shamer Scale (OAS) Allan, Gilbert and Goss 1994; Goss, Gilbert and Allan 1994).
The TOSCA is a contextual measure of internal shame and guilt (as well as two forms of pride) and views shame and guilt as two sides of the same coin. Here the term contextualised as defined by Kim, Thibodeau and Jorgensen (2011) means the scale aims to tap specific phenomenological aspects of shame experiences and embed them in a specific context by using scenarios to anchor the respondents’ answers. The PFQ-2 is a generalised measure of internal shame and guilt and has no theoretical model from which it is derived. Here the term generalised is defined by Kim, Thibodeau and Jorgensen (2011) as referring to the fact that the items in the scale make no reference to the phenomenology and behaviours that would characterise the construct of shame. The OAS measures external shame as uniquely defined in Gilbert’s model. In addition, each of these measures were developed using student cohorts and have not been tested on large clinical samples. This raises the question of the validity of the scales themselves and whether the measures would perform with the same statistical rigour on a clinical sample.
A further issue to consider, which is also raised by Kim, Thibodeau and Jorgensen (2011) is that several commonly used self-report measures of depression, notably the BDI (Beck, Ward, Mendelson, Mock, J.E. and Erbaugh, 1961) include questions that aim to assess the respondent’s sense of self-worth. Given self-worth is a key element of shame definitions this raises the possibility that self-report measures of depressive symptoms which contain items that aim to tap self-worth may lead to an inflation of the links between depression and shame and conflation of the two constructs. Thus, during statistical analysis this may adversely influence the effect size calculations for the relationship between shame and depression thus detracting from the robustness of the statistical data.
Why is the proposed study needed?
In conducting a literature search of the psychometric measures used in this PhD study it was established that these measures had never been tested on a clinical population diagnosed with persistent, treatment resistant depression. This was the population recruited to the CLAHRC-NDL Mood Disorder Study (Morriss, 2012) (n=187), which formed the sample for this PhD study. The following databases were searched between the years 1975 to 2018: Psycinfo; Medline; Embase; Pais; CINAHL which include articles for a range of health professional interests and areas, such as nursing, psychology and general medicine. The date parameters were chosen as it is across this time period that a clinical interest in shame, selfcriticism and self-compassion has emerged in the psychotherapy and emotion literature and the chosen end date marks the commencement of the thesis pending period for this PhD candidate. In addition, most of the existing literature related to shame, self-criticism and selfcompassion is written from a theoretical perspective (Tracy and Robins 2007a; Gilbert 2017a; 2007a). Testing these measures on a clinical population had potential to increase understanding of shame, self-criticism and self-compassion in a clinical population which in turn would enable more targeted treatment interventions to be developed.
The question of whether high levels of shame and self-criticism in a clinical population, do, as Gilbert (2017a; 2007a; 2005a; 2005b) argues, represent psychological constructs that from a vulnerability and maintenance factor in depression had never been addressed. Similarly, whether patients who exhibit higher levels of self-compassion experience lower levels of depression (see Barnard and Curry 2011; Neff 2003a) had never been tested on a clinical population. The modelling of variance of shame, self-criticism and self-compassion with depression proposed in this PhD study aimed to address these questions and represented a new contribution to the field.
Further there were no studies in this area which utilised a mixed methods design where the findings from quantitative and qualitative data sets are integrated. Within this methodology, which is increasingly used in healthcare settings where complex interventions are being evaluated, there is recognition that collecting both types of data has potential to yield findings which are of more practical application in the development of treatments. Such methodologies also give greater voice to participants, which potentially is more empowering to service users in influencing which research questions are investigated and how services are developed than the collection of quantitative data alone.
Chapter 3 Methods
Introduction
This chapter will begin with the statement of the PhD study research aims and objectives and an overview of mixed methods research design used. This is followed by an articulation of the ontological and epistemological position of this thesis, namely, what Biesta (2010) describes as Philosophical Pragmatism and the ‘primacy of praxis’. The chapter then moves into an indepth description of the research design and the methods. The chapter concludes with a description of the process of obtaining ethical approval to conduct this research.
Research aims and objectives
The aim of this study was to examine shame, self-criticism and self-compassion in persistent, treatment resistant depression using the frame of Gilbert’s (Gilbert, 2017a; 2016; 2007a) evolutionary psychobiosocial formulation of emotional disorders.
The PhD had three research objectives as follows:
1. To test the psychometric properties of three measures of shame, self-criticism and self-compassion in a cohort of participants diagnosed with persistent, treatment resistant depression.
2. To establish how much variance in scores on depression measures taken at baseline can be accounted for by variance in levels of shame, self-criticism and self-compassion in a cohort of patients diagnosed with persistent, treatment resistant depression.
3. To explore how patients diagnosed with persistent, treatment resistant depression experience shame, self-criticism and self-compassion.
Study Design
This study uses a Mixed Methods research design (Biesta, 2010; Teddlie and Tashakkori, 2010; Cresswell and Plano-Clark 2007; Doyle, Brady and Byrne 2009). This design was chosen because it is well suited to address the research questions posed and due to its utility in healthcare research. This is especially the case regarding the current Department of Health policy where the patient and their experience in NHS services has been placed at the heart of not only healthcare, (Institute for Public Policy Research (IPPR), 2018; Berwick 2013; Darzi, 2008;) but research (National Institute for Health Research (NIHR), 2019; Simpson, Jones, Barlow, Cox and Service User and Carer Group Advising on Research (SUGAR) 2014). The research environment has responded to these policy drivers by utilising integrated research methodologies which collect and interpret both quantitative and qualitative data sources. As Dolye, Brady and Byrne, (2009) observes this approach requires the researcher to articulate their ‘foundation of inquiry’ (p 176) that underpins the research being conducted.
Biesta (2010) offers a cogent argument for the use of Pragmatism as a philosophical foundation for mixed methods research. He offers a critique of the ongoing debate in the literature regarding the way key concepts are articulated in social and behavioural science research which, he argues, is inherently unhelpful because these concepts are applied in an imprecise way. The first is the use of the terms quantitative and qualitative research. He observes that research itself can be neither quantitative nor qualitative but rather only research data itself can be categorised in this way. Thus, data can be quantities (expressed in numbers) and qualities (expressed in words). However, he argues, much of the debate regarding quantitative and qualitative research encapsulates much more than defining types of data. Such debates range across methods and designs, as well as epistemological and ontological premises. Biesta (2010) argues that using the terms quantitative and qualitative to refer to these domains is both inaccurate and unhelpful. Specifically, it is unhelpful because the focus of the debate is not the nature of data but, views regarding the nature of reality, what constitutes knowledge and the politics of research.
The second problem he observes, (which Biesta argues is the cause of the first) is the unhelpful way in which the concept of paradigms is used in research. Thus, he argues, some research scholars use a silo mentality in which ideas that do not necessarily belong together are clustered in a particular domain under labels such as ‘positivism’ or ‘post-modernist’ and are labelled as paradigms. Inherent to this conceptualisation of paradigms is the notion that these ideas need to be fully embraced or rejected outright. Biesta (2010) argues that the researcher who conceptualises paradigms in this way abdicates their scholarly responsibility to consider the individual elements of ontology, epistemology, methodological position and assumptions within the research endeavour. Biesta (2010), critiques the work of Creswell and Plano-Clark (2011) claiming, whilst they have advanced researchers’ understanding of mixed methods research, they have maintained a clear distinction between quantitative and qualitative research. In so doing, they do not offer an integrated philosophical position that underpins the research typologies they propose. This, he argues, leads to an eclectic approach to the researcher’s ontological and epistemological position.
To advance further the endeavour of mixed methods research and develop a cogent epistemological position Biesta (2010) proposes seven levels to consider as part of this process.
Level 1: Definition of data
In a mixed methods approach data consist of both numbers and words or text. These are viewed as two forms of information and two modes of representations and therefore do not give rise to philosophical or practical dilemmas.
Level 2: Methods of data collection and analysis
In a mixed method approach a combination of questionnaires and interviews is used to collect data and as this is an extension of the numbers and words or texts definition of data, once more does not prove problematic. A combination of statistical and interpretative methods is used to analyse data. Biesta formulates this process as combining measurement and interpretation, each of which require a process of data analysis suitable to the type of data. Biesta argues that measurement in itself constitutes a form of interpretation and as such when it comes to data analysis this eradicates any distinction between the two types of data.
Level 3: Research design
In seeking to address the issue of epistemology and research design Biesta makes a distinction between interventionalist and non-interventionalist design (his italics). Thus, experimental design is classed as interventionalist and naturalistic design as non-interventionalist. He argues combining these in a single study is not problematic in itself. It is only when both strategies must be epistemologically accounted for via one knowledge claim, do problems arise. This is because knowing something through intervention, which is about the relationship between the intervention and the consequences of that intervention on a particular phenomenon is different from, knowing something through observation, which is knowledge about the phenomenon observed. At a practical level resolution of this lies in the process of triangulation in order to channel the two approaches into one knowledge claim by using a sequential or concurrent design. Biesta raises a more fundamental question as to whether it is possible to make a distinction between interventionalist and noninterventionalist ways of knowing, or whether the act of knowing always constitutes an intervention of some kind. As is discussed more fully in this chapter, Pragmatism argues that the only way we can make knowledge claims is by intervention.
Level 4: epistemology
The epistemological assumptions of mixed methods research is a point of much debate (see Cresswell, 2010; Johnson and Gray, 2010; Greene, 2008, for constructive debates), in which, according to Biesta, two questions need addressing:
-
What ideas do I hold about what I can know?
-
What does it mean to know something?
Given it is not possible to combine epistemological assumptions, Biesta (2010) urges the researcher to articulate the epistemological beliefs the researcher is using for the research design. It is here Biesta argues against the use of paradigms (as critiqued previously) to address this fundamental issue and encourages the researcher to consider each element of the research process separately i.e. epistemology, method, methodology, data etc. Importantly, this decision should be guided by the research question under investigation and not on personal conviction or choice.
Level 5: Ontology
Ontology refers to the assumptions we hold about the nature of reality and the reality that is the focus of our research. It is necessary to articulate the ontological assumptions we bring to our research as this will influence the type of knowledge we look for.
Level 6: purpose of the research
What is important here for Biesta is that the purpose of the research should be the guide to developing the research question and he makes a distinction between research that seeks to explain i.e. identify causes, factors, correlations and through this generate knowledge that can influence future courses of action and research that seeks to interpret, i.e. generate understanding by a process of identifying intention and reasons for action.
Level 7: practical roles
Here Biesta considers the interface between research and practice. Much of healthcare research is aimed at being of practical use and therefore it is important to describe how this intention towards practice is understood. Biesta (2007) identifies two ways in which research can connect to practice. Firstly, in a technical capacity by developing new techniques that a practitioner can use and culturally to provide clinicians with new ways of understanding their practice. These two distinct purposes require different kinds of research knowledge which can be usefully integrated. Biesta’s seven levels have shaped the foundation of inquiry in this thesis, which is presented in the following section.
Philosophical Pragmatism as an epistemological foundation
The theoretical foundations of this mixed methods thesis are what Biesta (2010) defines as Philosophical Pragmatism (his italics). In offering this definition Biesta is making a distinction between an epistemological position that draws on the philosophy of Pragmatism as posited by Dewey (1938) and what he terms everyday pragmatism (his italics), which refers to how the word pragmatism is used or indeed misused in everyday language. Biesta (2010 p. 96) observes that one of the difficulties in the mixed methods research literature is that some authors, (e.g. Onwuegbuzie and Johnson, (2006)) use this everyday definition of pragmatism to justify mixed methods design. Thus, researchers select the combination of methods which best suits the research questions posed, whilst claiming such a process is founded in Philosophical Pragmatism. In contrast, Philosophical Pragmatism, for Biesta is defined as ‘a set of philosophical tools that can be used to address a problem’ (Biesta 2010, p. 97). Thus, for Pragmatism the rasion d’etre for engaging in philosophical activity is to solve problems and as a school of thought it shuns the idea of building philosophical systems. This next section will briefly examine how Philosophical Pragmatism offers a unique epistemological and ontological position of what constitutes knowledge and how this is derived and verified. This refers to Biesta’s levels 4 and 5 described above.
Epistemology is concerned with the criteria we use to make claims about truth, knowledge and justification of beliefs. Hetherington (2006) observes that traditionally epistemology conceptualises knowledge as a state in which the epistemic subject has, via the formation of beliefs, a cognitive relationship to a true proposition. Hetherington disputes this traditional view by calling upon the epistemological thinking of Ryle (1971), who makes a distinction between knowing-that and knowing how. The former is defined as propositional or factual knowledge and the latter as practical knowledge, knowing how to do something. Thus, according to Hetherington (2006), knowledge is not a state such as a belief i.e. knowledgethat but can be classified as an ability i.e. knowledge-how and as such the knower is an agent not a subject. Thus, knowledge is conceptualised in terms of the ability to perform certain actions, namely, to represent or respond to reason. This argues Hetherington (2006) is a process of acting (agency) upon the world and not being acted upon by the world (subject). The latter being the more traditional epistemological definition of knowledge.
Pragmatism as a philosophy of science was first proposed by Charles Sanders Pierce (see Hookway, 2002 for an in-depth account). The work of Pierce was further developed by Dewey, who in 1938 published his ‘The theory of Inquiry’ (Dewey, 1938). It is here that the concept of the ‘primacy of praxis (or practice)’ that lies at the heart of Pragmatism as an epistemological position has its origins, as articulated in Biesta’s (2010) exposition of the Philosophy of Pragmatism.
This epistemological definition of knowledge is also expounded by Hookway (2006), who argues that epistemology is about assessing agency and that its purpose is to assess modes of inquiry rather than the traditional perspective of assessing the veracity of the resulting beliefs. For Hookway knowing is only relevant in terms of the role it plays in the process of purposeful inquiry and the epistemological position he expounds is one of ‘epistemology as a theory of inquiry’ (Hookway, 2006, p 98). It is this definition of epistemology, predicated on the Philosophy of Pragmatism, that underpins this PhD thesis.
Thus, successful inquiry commences when we encounter a problem and it is complete when we have a solution to that problem. It is argued that the pragmatist epistemology attempts to reconcile the dichotomy between the theoretical and the practical by placing at the heart of the epistemological process what is termed ‘the primacy of praxis’. Thus, reasoning is a goal-directed activity (my italics) and epistemology is about assessing agency, where the purpose is to assess modes of inquiry rather than the traditional perspective of assessing the veracity of the resulting beliefs. In this regard primacy is given to what is referred to in Pragmatism as ‘the norms of practical reason’, that is, strategies for problem-solving and the effectiveness of agents in implementing these strategies. Grice (1989), observes that in conceptualising rationality philosophy frequently neglects to consider the fact that reasoning is in itself an activity with both purpose and goal. In Hookway’s thesis he is concerned with how can we succeed in our inquiries about what to believe and how can we adopt sound strategies for inquiry and be disciplined in our execution of these strategies? Thus, he poses the question:
‘How is it possible to be good at inquiry, rather than, more simply, what is it to have justified
beliefs or knowledge? How can we obtain knowledge in practice?
(Hookway, 2006, p 101).
It is from this position of epistemology as a method of inquiry and the primacy of praxis that a mixed methods research design was chosen for this thesis. The long-term aim of the researcher is to hone CBT treatment interventions and improve patient outcomes in depression. Deploying a mixed method research design this holds the possibility of a bridge between the potential ubiquity of quantitative measurement of, what the quantitative paradigm would label as symptoms (depression) or psychological constructs (shame, selfcriticism and self-compassion) and the idiosyncratic lived experience of people who describe such symptoms and psychological phenomena as might be investigated using qualitative research methods. This also seeks to work towards the goal described in Biesta’s
(2010) level 6 and 7 criteria, namely the purpose and practical role of research in practice. This epistemology, research design, data collection and analyses methods are underpinned by the ‘primacy of praxis’ principles in several ways, which will be outlined below.
Convergent Parallel Mixed Methods
The quantitative arm of this PhD study deployed a set of measures purporting to measure shame, self-criticism and self-compassion with the aim of testing whether they have validity as measures of these constructs, expressed as psychological symptoms, in a cohort of participants diagnosed with persistent, treatment resistant depression. Each measure renders an overall score with a cut-off point, aimed at describing the level of symptomatology that defines the constructs being measured. As such, measures validly help us to measure the what i.e. the symptoms which are grouped within a diagnostic classification system and a categorised definition of what the overall score signifies e.g. high levels of shame and selfcriticism, low levels of self-compassion. This is valid and has purpose, but also has limitations; specifically, it can be argued it lacks clinical meaning. The overall scores help us to define the problem and measure its severity (the what), providing a baseline by which change can be measured. However, measures do not help us with the how. Measures do not shed any light on how to treat the symptoms the scales measure or indeed whether the interventions we use to target these symptoms are efficacious and effective and acceptable to and useable by patients. Thus, a further hypothesis might be usefully tested using a different data collection method to explore the same constructs.
On this basis in this PhD study a decision was taken to include qualitative data collection as a means to examine more closely how depression, shame, self-criticism and self-compassion are described and experienced by a cohort of participants diagnosed with persistent, treatment resistant depression. The purpose of this inquiry is to collect data that may either contradict or complement that which is collected in the quantitative phase of the study and in the long term to use this to inform the further development and refinement of CBT interventions for persistent, treatment resistant depression.
The Research method used in this PhD study was a convergent parallel mixed methods design. Cresswell and Plano-Clark (2011, p 73) describe six core mixed methods research designs of which one is the Convergent Parallel Design used in this study, this will be described in detail below. The other mixed methods designs can be summarised as follows:
Explanatory Design: This design is useful when the researcher needs to explain quantitative results. In this design methods are implemented sequentially beginning with quantitative data collection and analysis in phase I followed by qualitative data collection and analysis in phase II which builds on phase I.
Exploratory Design: This design is useful when the researcher needs to test or measure qualitative exploratory findings. In this design the research methods are implemented sequentially beginning with qualitative data collection and analysis in phase I of the study. In phase II quantitative data collection and analysis is implemented building on phase I.
Embedded Design: This design is useful when the researcher needs to conduct some preliminary exploration before conducting and experimental trial (either prior or sequentially) or where the researcher requires a more complete understanding of an experimental trial i.e. process and outcomes concurrent or during the trial or there is a need to follow-up explanations after an experimental trial (either sequentially or following the trial). In this design there is either, concurrent or sequential collection of supporting data with separate data analysis and the use of supporting data before, during or after the major data collection procedures.
Transformative Design: This design is specifically used in a context where there is a need to conduct research that identifies and challenges social injustice. In this design the concurrent or sequential collection of data and the analysis of quantitative and qualitative data sets is framed within a transformative theoretical framework that guides the decision-making regarding methods used.
Multiphase Design: This design is used where the researcher needs to implement multiple phases to address a programme objective such as programme development and evaluation. In this design concurrent and/or sequential collection of quantitative and qualitative data sets are combined over multiple phases of a programme of study.
The Convergent Parallel Design used in this study and the data collection method is summarised in Figure 2 below. This diagram is taken from Creswell and Plano-Clark (2011, p
69).
FIGURE 5: CONVERGENT PARALLEL MIXED METHODS DESIGN (CRESWELL AND PLANO-CLARK (2011, P 69)
As the diagram above indicates quantitative (numbers) and qualitative data (words/text) were collected in parallel. This process followed the research design principles described by Creswell and Plano-Clark (2011), underpinned by epistemological and ontological position founded in the Philosophy of Pragmatism (Biesta 2010). The two research strands were distinct and the quantitative and qualitative research questions, data collection and data analysis were kept separate. The two strands were only integrated when conclusions were drawn during the phase of overall interpretation when the study had been completed. However, the quantitative and qualitative strands had equal priority, whereby, each was seen to play an equal role in addressing the research aims. Morse (1991, p 122), states the purpose of the convergent parallel design is ‘to obtain different but complementary data on the same topic’. In this methodology triangulation was used to directly compare and contrast quantitative statistical results with qualitative findings in order to address the research aim via a process of validating and corroborating findings.
As a clinician delivering evidence based psychological treatment (CBT) to patients diagnosed with persistent, treatment depression, it is easy to observe discrepancies between the theory which underpins CBT for depression and the implementation of that theory via its treatment interventions. To some extent theories are ubiquitous whilst patients, as human beings, are idiosyncratic. This raises the question of how the theories that inform CBT interventions are developed and the interventions themselves tailored to engage the individual and target the proposed maintenance factors in the depressive presentation. This mixed methods approach enables the researcher to develop a more complete understanding of a phenomenon, in this case the role of shame, self-criticism and self-compassion in persistent, treatment resistant depression and to explore that phenomenon from different methodological perspectives. In keeping with Biesta’s (2010) formulation of the purpose and practical utility of research
(level’s 6 and 7), this was an important driver in using a mixed methods approach in this study. The first question addressed in this study aimed to validate a set of quantitative measures related to a specific theory of shame (Gilbert 2007a) that had never been tested on a clinical population of patients diagnosed with persistent, treatment resistant depression. The second question sought to address the question of whether shame, self-criticism and selfcompassion are psychological constructs which play a role in the maintenance of depression or whether they are mood dependent phenomena that vary according to severity of depressed mood. The final question in this study sought to examine patients lived experience of persistent, treatment resistant depression, shame, self-criticism and self-compassion by collecting qualitative data using a semi-structured interview. The aim being to try and capture a more complete understanding of these constructs. This was considered useful on two counts. Firstly, in terms of corroborating (or otherwise) the data derived from quantitative component of the study, but also to shed light on how clients make sense of and engage with constructs of depression, shame, self-criticism and self-compassion which may be of use in the future in terms of honing CBT treatments for persistent, treatment resistant depression. The convergent parallel design was chosen as it best suited the research questions under investigation and the wider research context in which the PhD study was conducted (see Biesta (2010) level 3 discussed earlier in this chapter).
PhD Study Context
This PhD study was conducted within a 5-year RCT National Institute for Health Research (NIHR) funded programme grant within the CLAHRC-NDL Mood Disorder Study (trial registration number: NCT01047124) (Morriss, Martunnen, Garland, Nixon, McDonald,
Sweeney, Flambert, Fox, Kaylor-Hughes, James, and Yang, (2010). The trial compared a Specialist Depression Service (SDS) offering National Institute of Clinical Excellence (NICE) recommended pharmacological and psychological treatments (NICE CG90, 2009) for patients diagnosed with persistent, treatment resistant depression with Treatment As Usual (TAU), where TAU meant any intervention (pharmacological and/or psychological) offered in secondary care mental health services. The RCT had three sites: the primary site Nottinghamshire Healthcare NHS Trust and two secondary sites, Cambridge and Peterborough NHS Foundation Trust and Derby NHS Foundation Trust.
The PhD candidate was one of two grant holders for this trial, the clinical lead for the SDS in Nottingham and the primary clinician delivering CBT in the research trial in Nottingham. The quantitative data collection was not conducted by the PhD candidate but by the study research associates. The PhD candidate did select the theory to be tested in this PhD, set the aims and objectives for the PhD study and selected the measures that were to be tested. The data entry and analysis for the measures tested in this PhD thesis was completed by the PhD candidate. The qualitative data collection and analysis was conducted by the PhD candidate.
The Study Sample
The flow of participants into the RCT in which this PhD thesis is based is shown in appendix
VII. This can be summarised as follows. In total 310 participants were referred to the study. Of this original cohort 86 either withdrew following referral or were deemed not to meet the study intake criteria on assessment of the referral i.e. the primary element of the clinical presentation was not recurrent depression. 224 participants went on to complete a baseline face to face interview to assess if their clinical presentation met the study intake criteria. Of these 37 either withdrew from the study or did not meet the study intake criteria (see below for a description of these). The final study sample thus consisted of 187 participants across the three NHS Trusts, Nottingham (137), Cambridge (29) and Derby (21). The psychometric measures tested in this thesis were administered to this cohort. The Cambridge site failed to administer one of the measures used in this PhD study to their cohort of 21 participants.
Sampling
Sampling refers to the process by which the researcher identifies a representative sample of the population under study. It is important to reduce to a minimum, sampling errors. A sampling error is the difference between the sample recruited in the research study and the population under study i.e. the error has arisen because the data collected is from one part rather than the whole of the population under study. The sample size refers to the number of participants or observations included in a study and the sample size has two statistical properties:
-
Precision of the estimate
-
Power of the study to draw conclusions
It is vital from the outset of a research study to consider the possibility of sampling error. In any research study the researcher cannot be absolutely precise about the relationship between the factors under study because it is impossible to study every instance under which the factors coincide. This is a further example of a sampling error and whilst it cannot be eliminated it can be reduced by sample size. Thus, a larger sample size is associated with a smaller margin of error. Therefore, to maximise the researcher’s chances of obtaining an accurate picture as possible of the area under study a large number of examples are useful in order to observe and compare. However, there is a point at which increasing the sample size no longer influences sampling error. On this basis power calculations are used, and this is known as probability sampling. A power calculation refers to the probability of finding a statistically significant result and is calculated by specifying both the null hypothesis and the alternative hypothesis (often the predicted outcome of the study) in statistical terms. These two alternatives are then used in the power equation calculation in order to answer the research questions posed.
The power calculation in this PhD study
For this PhD study an a priori power calculation was undertaken as part of the CLAHRC-NDL RCT (Morriss, Martunnen, Garland, Nixon, et al, 2010). Thus, the research team calculated the necessary sample size to generate the required statistical power (Morriss 2012). The sample size calculation is described below and is précised from Morris, Marttunnen, Garland, Nixon, et al, 2010). The calculation was based on improvement in global assessment of severity in a study using a similar design only which recruited a mixed diagnostic group (Guthrie, Moorey, Margison, Barker, Plamer, McGrath, Tomenson and Creed (1999), rather than, (as in the RCT in which this PhD study was conducted), a group meeting diagnostic criteria for a moderate to severe primary depressive disorder. This calculation was estimated as follows: 90% power, with 2 tailed differences at 5% significance and a 20% loss to follow up required 52 per treatment group (104 participants in total). However, the Guthrie, Moorey, Margison, Barker, et al (1999) study did not use an intention to treat analysis and there was a 30% loss to follow up. As a result, the sample size for the RCT where this PhD study was conducted was increased by a further 43% to 74 participants per group (a total of 148 participants). A further correction was made for the variability in the individual treatment delivered by the Specialist Depression Service and TAU. Thus a multiplicative correction factor to the sample size estimate of 1.18 was calculated from [1 +rho*/(1-rho)] (Gulliford, Adams, Ukoumunne, Latinovic, Chinn, Campbell (2005) where rho is the intraclass correlation of 0.051 (Goldstein 2003) and r is the number of patients recruited from each community mental health team per treatment arm (3–4). As a result, the sample size was increased to 87 per treatment group (174 participants in total). These sample size calculations were checked against a study of evaluating combined psychotherapy and pharmacotherapy versus treatment as usual delivered in an inpatient setting for participants with a chronic depressive disorder (Schramm, Schneider and Zobel, Van Klaker, Dykierek, Kech, Harter, and Berger,
2008).
Sample size
To establish reliability and validity of a psychometric measure it is advised that a large sample representative of the population under study be recruited (Kline 2000). It is possible that random errors may be a problematic feature of using these measures with a depressed sample which may adversely affect their validity. This is due to the number of measures being completed and the nature of the material with which the participants are engaging, interacting with depressive symptomatology such as, poor concentration and memory deficits which may impact on their responses. Therefore, the Standard Error of Measurement (SEM) for the measures tested in this thesis (see below for a full description of these) was calculated using the STATA Statistical software package (StataCorp, 2013). Completion of these measures with both the clinical and healthy control group allowed the SEM to be calculated and taken into consideration when totalling scores on the measures tested for the participant sample.
Participants for the qualitative arm of the study were purposively sampled from the TAU group within the RCT clinical sample. This process is known as non-probability sampling, the rationale for which was as follows. Firstly, the PhD candidate was the primary therapist in the RCT. As such, to conduct interviews with participants already known to the interviewer would not only have introduced bias, but also raised ethical concerns regarding the potential for coercion. Participants already known to the interviewer may on the one hand have been more willing to disclose the type of highly personal and sensitive information the interviewer would be focusing on. However, equally the participant, if he/she had already established a therapeutic relationship with the interviewer may feel unable to decline a request to participate for fear of the implications of this for their future treatment. Equally they may feel it is important to ‘please’ the interviewer/therapist or ‘offer something in return for help’ and therefore feel obligated to take part. The participants, if known to the interviewer in this way may also have felt compelled to answer questions in a way that ‘pleases’ the researcher rather than from their own perspective and experience.
A maximum variance sample was selected in order to capture at least one member of any group whose perspective may affect their experience of shame, self-criticism and selfcompassion for example:
-
Men versus women
-
Age range i.e. 18–30 versus 31–50 versus 51–70 versus 70–100
-
Educational level
-
Socio-economic status
-
ethnicity
-
Practising a specific religion versus agnosticism versus atheist
-
Past trauma and/or abuse versus no past trauma and abuse
The number of interviews conducted was governed by the point at which the themes become saturated, that is the interviews were covering the same ground. At this point the maximum variance sample has been collected. In this study 10 interviews were conducted.
In addition to the above, a sample of 33 healthy controls was recruited from the general public in Nottingham City and County. This sample was used as a control group against the clinical sample when testing the reliability and validity of the three psychometric measures under investigation in this PhD study. This sample was matched against the clinical sample for demographic data including age, gender, marital status, occupation and level of education. The sample was recruited by placing adverts to participate in the study both electronically on the CLAHRC-NDL website and with posters placed in public places in the hospital Trust where the candidate works and the University of Nottingham which was a CLAHRC-NDL collaborator. In the interests of limitations on word count a decision has been taken not to include the advert in the appendices.
The criteria for defining a healthy control was determined through a process of discussion among a triad of appropriately qualified mental health professionals. This included the PhD candidate and two supervisors, a professor of mental health nursing and a professor of psychiatry. Through this process it was agreed to grant healthy control status to potential participants who had no current or past history of psychiatric or mental health problems. It was noted as part of the screening process attention needed to be paid for current or past indicators of generalised anxiety, specific phobias and episodes of mental ill-health that may have been sub-threshold and/or present but for which treatment was not sought i.e. depressed mood and anxiety as a consequence of a life event such as bereavement, divorce, redundancy.
Potential healthy control participants responding to the advertisement to participate in the research were asked to contact the PhD candidate via email. Their email was responded to with an email invitation (see appendix VIII) from the PhD candidate to participate in a short, ten minute telephone interview to ascertain that potential healthy control participants met the predefined criteria for healthy control status if the person met the healthy control criteria.
The process by which it was determined that healthy control participants met these predefined criteria was established via a short ten-minute telephone interview with each participant. During this interview a series of questions (see appendix IX) was asked to establish:
-
Demographic details of the participant
-
Past history and current experience of mental health problems including depression and anxiety
If participants met the inclusion criteria for healthy control, then they were invited to attend a face-to-face interview in which the same battery of measures given to participants in the RCT and relevant to this PhD study were administered. The healthy controls participant information sheet was adapted from the qualitative data collection study participant information sheet which can be seen in appendix X. Also, the healthy controls participant consent form was adapted from the RCT participants consent form and can be seen in in appendix XI). The measures administered are described later in this chapter.
Recruitment Process
This information is précised from the RCT study protocol version 9 (Morriss, 2012).
Participants were recruited from community mental health teams, mental health out-patient clinics, self-help groups and general practitioners via presentations (conducted by various members of the research team) and a poster. In the interests of limitations on word count a decision has been taken not to include the advert in the appendices.
The initial approach regarding participating in the RCT was made by a member of the patient’s usual care team. Information about the RCT was also on display in relevant clinical areas (i.e. psychiatric out-patient clinics) as well as self-help groups, drop-in, day care, inclusion and homeless centres. Participants could directly contact the research team to enrol in the study, but the appropriateness of their participation was checked with their care coordinator prior to acceptance. Once the usual care team had given permission for a potential participant to be approached by the research team then the participant was contacted and given a patient information sheet (see appendix X for a version of the participant information sheet). After at least 24 hours the participant was then contacted to enquire if they wished to participate in the RCT. If so, then both oral and written consent was obtained and eligibility for the study formally assessed. Participants were not randomised if they did not meet eligibility criteria at baseline assessment.
Inclusion and exclusion criteria for the RCT
As described previously, the participant sample investigated in this PhD study were recruited as part of an RCT. The inclusion and exclusion criteria for the RCT are summarised here to provide a descriptive indicator of the sample population on which this PhD study was conducted. These criteria are taken from the RCT study protocol version 9 (Morriss, 2012).
Participants included in the study met diagnostic criteria for clinical depression of at least moderate severity as defined by the Structured Clinical Interview for DSM-IV Axis 1 Disorders (SCID) (First, Spitzer, Gibbon and Endicott, 1997). As it was a pragmatic RCT the inclusion/exclusion criteria reflected the day-to-day clinical criteria used in NHS clinical practice within a specialist mood disorders team (Tansella, Thornicroft, Barbui, Cipriani and Saraceno, 2006).
The inclusion criteria were as follows:
-
The responsible medical officer or care-coordinator deemed the participant to be suffering from primary unipolar depression which was not a consequence of having another axis I or Axis II psychiatric disorder
-
Aged over 18 years
-
Able and willing to give oral and written consent to participate in the RCT
-
From the date of first assessment by a health professional working within the index mental health Trust, primary care Trust or third sector, the participant had to have been offered or received direct and continuous care from one or more health professionals in the preceding 6 months within a secondary care mental health team • Met NICE criteria for moderate depression (five out of nine symptoms of depression
(NICE, CG23, 2004); had a Hamilton Depression Rating Scale-17 (HDRS-17, Hamilton, 1960) score of at least 16 (indicative of a mild level of depression); and scored 60 or less on the Global Assessment of Functioning (GAF) Scale (American Psychiatric Association, 1994) which represents what is considered a typical score for a person receiving help in a psychiatric out-patient clinic.
-
Patients with other co-morbid psychiatric or medical disorders were included provided these conditions were not the primary diagnosis or the depression was best understood as a complication of the primary psychiatric or medical disorder.
The exclusion criteria were as follows:
-
The participant was receiving emergency care for suicidal risk, risk of severe neglect or homicide risk. However, participants were not excluded because of such risk provided the risk was adequately managed within their usual care setting and the primary medical responsibility for care remained within the referring team.
-
The participant did not speak fluent English
-
The participant was pregnant
-
Participants with a diagnosis of bi-polar disorder which had not been diagnosed by the primary care team, but which was identified at baseline assessment and in the course of the research were not excluded. This is because in NHS clinical practice such presentations would be managed within a specialist mood disorders service and usual care teams.
Once recruited and assessed at baseline participants were randomised to either the active treatment arm of the study the SDS or TAU where they received 12 months treatment. Followup appointments for all willing participants were conducted at 18 and 24 months respectively to describe the long-term efficacy of the intervention.
Data Collection Methods
This section will describe the data collection methods for the quantitative and qualitative components of the study. An overview of these can be seen in Table 4.
TABLE 4: SUMMARY OF DATA COLLECTION AND ANALYSIS METHODS
| Objectives | Data Collection Method | Data Analysis | Outcome |
| To test the psychometric properties |
-
Others as Shamer Scale
(OAS)
-
The Forms of Self-
Criticising/Attacking and Self-reassuring Scale (FSCRS)
-
Self-Compassion Scale
(SCS) | Measures administered to a clinical sample of 157 patients diagnosed with persistent, treatment resistant depression enrolled in an RCT and 33 healthy controls. | Quantitative data analysis
Statistical tests:
Reliability
-
Internal
Consistency
-
Test-retest Parallel Form
Validity
-
Face Validity
-
Content Validity
-
Construct Validity
| - Factor Analysis | Establish the psychometric properties of the chosen scales |
| To test variance in scores on depression measures at baseline against variance in levels of shame, self-criticism and selfcompassion on the following measures: |
-
Hamilton Rating Scale for Depression (HRSD)
-
Beck Depression
Inventory (BDI)
-
Patient Health
Questionnaire-9 (PHQ-
9)
-
Others as Shamer Scale
(OAS)
-
The Forms of Self-
Criticising/Attacking and Self-reassuring Scale (FSCRS)
-
Self-Compassion Scale
(SCS) | Measures
administered to a clinical sample of 157 patients diagnosed with persistent, treatment resistant depression enrolled in an RCT and 33 healthy controls. | Quantitative data analysis:
Statistical tests:
Correlation and multiple Regression Analysis to measure variance between shame, self-criticism and selfcompassion and level of depression within the clinical sample comparing the active treatment group with the treatment as usual group. | To determine how levels of shame, self-criticism and selfcompassion correlate with level of depression
To determine the Construct Validity of Gilbert’s shame theory |
| To explore how patients with persistent, treatment resistant depression experience shame, self-criticism and self-compassion | Semi-structured interview with 10 participants from TAU arm of the study | Qualitative data analysis |
Interpretative
Phenomenological Approach
(IPA) | Describe and discuss how patients diagnosed with persistent, treatment resistant depression construct meaning in relation to shame, self-criticism and self-compassion
To test the construct validity of Gilbert’s theory of the role of shame, self-criticism and self-compassion in patients diagnosed with chronic
depression | Detailed Description of Quantitative Data Collection Method
Step 1: Testing the psychometric status of OAS; FSCR and SCS
A set of psychometric measures were specifically chosen to test Gilbert’s shame theory, these were:
-
Others as Shamer Scale (OAS) (Allan, Gilbert and Goss 1994; Goss, Gilbert and Allan, 1994)
-
The Forms of Self-criticising/attacking and Self-reassuring Scale (FSCSR) (Gilbert, Clarke, Kempel, Miles, and Irons, 2004)
-
The Self Compassion Scale (SCS) (Neff 2003a; 2003b)
Rationale for chosen measures of shame, self-criticism and self-compassion
Kim, Thibodeau and Jorgensen, (2011) urge researchers as a matter of priority to adopt:
‘sharp conceptual definitions of shame and guilt or their various sub-types and to select or
construct measurement tools that clearly map these definitions’
(Kim, Thibodeau and Jorgensen, 2011, p 88).
This PhD study used Gilbert’s (2017a; 2014; 2007a; 2005b; 2003; 2000) conceptual definitions of shame, self-criticism and self-compassion and deployed three measures, the OAS (Allan, Gilbert and Goss 1994), FSCRS (Gilbert, Clarke, Kempel, Miles, and Irons 2004) specifically designed and tested by Gilbert and his colleagues based on his conceptual definitions of shame and self-criticism. The third measure used was the Self-Compassion Scale (SCS, Neff, 2003a; 2003b).
The OAS is a measure of external shame. Gilbert’s theory is unique among shame theories in making a distinction between internal and external shame. In addition, in Gilbert’s theory external shame is the form of shame linked to psychopathology i.e. depression and anxiety. This is the only shame scale which attempts to assess this concept of external shame. All other shame measures focus on an individual’s internal experience of shame or a person’s response to potentially shaming events.
The FSCRS (Gilbert, Clarke, Kempel, Miles, and Irons 2004) was chosen as it is concordant with Gilbert’s shame theory. This is the only self-criticism measure that is underpinned by this theory. In Gilbert’s theory, self-criticism is a marker for internal shame which is conceptualised as a by-product of external shame.
At the commencement of this PhD study the literature reported four other scale purporting to measure self-criticism. These are summarised briefly here. Carver and Ganellen, (1983), devised the Attitudes Towards Self Scale (ATSS) which measures three constructs, high standards, overgeneralisation and self-criticism using a numerical Likert Scale. Self-criticism is defined as making harsh judgements of self as a result of failing to meet standards. The item wording does not explicitly state ‘self-criticism’ as part of content. A revised version of this scale was developed by Carver, La Voie, Kuhl, and Ganellen, (1988).
Ishiyama and Munson, (1993) developed the Self-Critical Cognitions Scale, which aims to measure what the authors refer to as a ‘dispositional tendency to process self-referent information in a self-critical way’ (Ishiyama and Munson, 1993, P 148). The Measure has two sub-scales, one measuring ‘negative self-processing’ and another measuring ‘failure in positive self-processing’. The item content focuses on the tendency towards self-criticism, making a negative social comparison, difficulty in maintaining a balanced perspective about self and exaggeration of negative aspects of self, using a six point agree-disagree Likert scale.
Thompson and Zuroff (2004), formulating self-criticism as a personality construct, devised the Levels of Self-Criticism scale (LOSC). This measures comparative self-criticism, which is defined as: ‘a negative view of self in comparison to others’ and internalised self-criticism which is defined as ‘a negative view of self in comparison with internal personal standards’
(Thompson and Zuroff, 2004, p 420). Item content makes no explicit reference to selfcriticism.
Parker, Manicavasagar, Crawford, Tully, and Gladstone, (2006), also formulate self-criticism as an aspect of personality and which predisposes the individual to depression, developed the
Temperament and Personality Questionnaire. Here, self-criticism is defined as a tendency to be extremely hard on self, with items focusing on self-criticism, being hard on self, high personal standards and sense of satisfaction with self, using a Likert scale response method.
Since the completion of the data collection period of this PhD study the Self-Critical Rumination Scale (Smart, Peters and Baer, (2015) has been devised. This formulates selfcriticism as a ruminative process with the purpose of devaluing self. Item content, which is rated on a Likert scale, focuses on the frequency and repetitive nature of rumination and the content of self-criticism, including aspects of self which are shame related.
The self-compassion measure used in this PhD study, the Self-Compassion Scale (SCS) (Neff 2003b) was not developed by Gilbert. At the time of commencing this PhD study Gilbert had not developed a scale for measuring self-compassion. In 2011 he published three self-report measures rating fear of self-compassion (Gilbert, McEwan, Gibbons, Chotai, Duarte and Matos, 2011; Gilbert, McEwan, Matos and Rivis, 2011). This fear of self-compassion is a further development of his theory and does not measure the construct of compassion per se but, has been developed in response to the clinical observation that patients with mental health problems are resistant to the idea of self-compassion. In the absence of a selfcompassion scale devised by Gilbert the scale developed by Neff was chosen as the most appropriate available scale purporting to measure self-compassion. This scale is consonant with the conceptual definition of self-compassion in Gilbert’s theory, given there is a strong consensus within the research literature regarding conceptual definitions of self-compassion (Leary, Tate, Adams, Batts-Allen and Hancock, 2007; Neff 2003a; 2003b) as they are derived from Buddhist conceptual definitions of compassion. There is one other scale designed to measure what is termed compassionate love which is the Compassionate Love Scale (Sprecher and Fehr 2005). There are three versions of this scale, compassionate love for self, for others and for strangers. Neff’s measure has been chosen as it specifically focuses on selfcompassion. As this study is testing Gilbert’s formulation of shame, self-criticism and selfcompassion, in which the capacity for self-soothing via self-compassion is seen as key to the amelioration of depression then Neff’s measure is seen as more directly tapping into the constructs under investigation in this study.
An overview of each measure
The next section will provide an overview of each measures used in this PhD study. This will include a description of the origin of each scale, the content, the scoring and interpretation of the scoring. There will be a brief description of the psychometric properties of each scale as assessed in the design and validation of each scale.
Other as Shamer Scale (OAS)
The Other as Shamer Scale (OAS) (see appendix XII) (Allan, Gilbert and Goss 1994; Goss, Gilbert and Allan 1994) is an 18 item self-rated scale measuring external shame which Gilbert defines as ‘an individual’s global judgments about how people think others view them’ (Cheung, Gilbert and Irons 2004). The measure uses a 5-point Likert scale (0–4) to indicate the frequency of their feelings and experiences (0= never, 1=seldom, 2= sometimes, 3= frequently, 4=almost always) on a range of items.
The scale items comprise three components:
1. Inferior (e.g. ‘other people see me as not measuring up to them’ items 1, 2, 4, 5, 6,7,8)
2. Emptiness (e.g. ‘others see me as fragile’ items 15,16, 17, 18)
3. How others behave when they see me make a mistake (e.g. ‘other people always remember my mistakes’ items: 3, 9, 10, 11, 12, 13, 14)
A total OAS score is calculated by adding up the individual numerical score for each item as assigned by the respondent. There is no reverse scoring of items. There is no cut off points defined in this measure.
The authors tested the scale on a sample of 156 university students, 118 females and 38 males. In the Goss, Gilbert and Allan (1994), study the scale showed high internal consistency with a Cronbach’s alpha coefficient of 0.92 and a principal component analysis revealed 3 factors which accounted of 60.4% of variance. The authors note that the results obtained are concordant with evolutionary theory, that shame is related to subordinate-dominant and inferior-superior judgements with the factor ‘Inferior’ accounting for the largest proportion of variance (44%).
The forms of self-criticising/attacking and self-reassuring scale (FSCRS)
The forms of self-criticising/attacking and self-reassuring scale (see appendix XIII) (Gilbert, Clarke, Kempel, Miles, and Irons 2004) is a 24 item self-rated scale which examine how critical/self-attacking versus supportive and reassuring people are towards themselves when things go wrong for them. In completing the measure participants rate using a first probe statement ‘when things go wrong for me…‘on a five point Likert scale (ranging from 0=’not at all like me’ to 4=’extremely like me’) on a series of questions, for example, ‘I am easily disappointed in myself’, ‘I find it easy to forgive myself’.
The scale items comprise three components as follows:
1. Inadequate self (focusing on a sense of self as personally inadequate e.g. ‘I am easily disappointed in myself’ items 1, 2, 4, 6, 7, 14, 17, 18, 20)
2. Hated self (focusing on a desire to hurt or persecute self-e.g. ’I have become so angry at myself that I want to hurt or injure myself’ items 9, 10, 12, 15, 22)
3. Reassuring self (focusing on self-reassurance e.g. ‘I am able to remind myself about positive things about myself’ items 3, 5, 8, 11, 13, 16, 19, 21)
A total FSCRS score is calculated by adding up the individual numerical score for each item as assigned by the respondent. There is no reverse scoring of items. There are no cut off scores for this measure.
Gilbert, Clarke, Kempel et al (2004) tested the measure on a sample of 246 undergraduate female psychology students. Cronbach Alpha’s coefficients were 0.90 for inadequate self and 0.86 for hated self and reassuring self. Self-reassuring was negatively correlated with depression and other forms of self-criticism/attacking. The authors note that the sample is not representative of a typical clinical population and urge the testing of the measure on a clinical population.
Self Compassion Scale (SCS)
The Self-Compassion Scale (SCS) (see appendix XIV) (Neff 2003b) is a 26 item self-rated scale that purports to measure three facets of self-compassion:
-
Self-kindness (being kind and understanding towards self as opposed to harshly selfcritical e.g. ‘I try to be loving towards myself when I’m feeling emotional pain’)
-
Common Humanity (viewing negative experiences as a normal part of the human condition rather than as being the only person who experiences such difficulties e.g. ‘When I am down and out, I remind myself that there are lots of other people in the world feeling like me’)
-
Mindful Acceptance (holding painful thoughts and feelings in mindful awareness rather than over-identifying with them e.g. ‘When something upsets me, I try to keep my emotions in balance’)
The measures categorise items into sub-scales as follows:
Self-kindness (items 5, 12, 19, 23, 26) versus Self-judgement (items 1, 8, 11, 16, 21)
Common Humanity (items 3, 7, 10, 15) versus Isolation (items 4, 13, 18, 25)
Mindfulness (items 9, 14, 17, 22) versus Over-identified (items 2, 6, 20, 24)
The measure uses a five-point Likert scale (1–5) with two anchor points at either end of the scale (1=almost never and 5 = almost always). Sub-scale scores are computed by calculating the mean of sub-scale item responses. An overall total self-compassion score can be calculated. This is done by reverse scoring the negative sub-scale items for self-judgement, isolation and over-identification (i.e. 1=5, 2=4, 3=3, 4=2, 5=1) before calculating the sub-scale means, then calculating a total mean of all six-subscale means. Neff asserts that using the mean of each sub-scale to calculate the total score makes the data easier to interpret. Data analysis can use individual sub-scale scores or a total score which reflects a global measure of self-compassion. In this PhD total scores were used.
Neff (2003b) tested the measure on 232 undergraduate students, 87 male and 145 females randomly selected from a pool of students studying educational psychology. The ethnic breakdown of the sample was 58% white, 22% Asian, 14% Hispanic, 3% black and 3% other. Neff reported a Cronbach’s alpha coefficient of for a total self-compassion score as 0.92.
Leary, Tate, Adams, Batts-Allen and Hancock (2007), also tested Neff’s self-compassion measure in five linked studies investigating self-compassion and reactions to unpleasant, selfrelevant events. Once more the participants were drawn from university undergraduate students. The first study recruited 59 male and 58 female participants age 17–21 and the reported Cronbach’s alpha coefficient on this sample was 0.91.
In a meta-analysis examining the link between self-compassion and psychopathology, (MacBeth and Gumley 2012), the authors identify Neff’s measure as the most frequently used self-compassion scale in the research literature. They identified a total of fourteen publications which met their criteria for being included in the meta-analysis. Of these fourteen studies seven used a community clinical sample. Of these seven only one, (Kuyken, Watkins, Holden, White, Taylor, Byford, Evans, Radford, Teasdale and Dalgleish 2010), recruited a primary care, participant sample who met diagnostic criteria for depression. It is therefore reasonable to state that Neff’s measure has rarely been tested on a sample of participants meeting diagnostic criteria for depression and never on a sample from secondary care mental health services with the degree of recurrence severity recruited in the RCT where the measure is being tested.
It is common practice when testing concurrent validity of a measure to test the measure(s) under study against a previously validated measure of each specific construct. This method was not chosen for this study. The rationale for this was that the study aimed to test Gilberts; formulation of shame in a cohort of participants diagnosed with persistent, treatment resistant, depression (Gilbert 2017a; 2016; 2014; 2007a; 1992). Whilst the literature search revealed fifteen measures of shame that could have been deployed to this end in this study, each measure is underpinned by a different shame theory and in this respect there are no definitive alternative measures of shame, self-criticism and self-compassion against which to compare the OAS; FSCRS and SCS items and responses. These differences in underlying theoretical assumptions regarding shame, on which the constructs in each measure are based would make comparison difficult and may generate misleading results. The OAS, FSCRS have only been tested on students (Gilbert, Clarke, Kempel et al 1994; Cheung, Gilbert and Irons 2002) and patients engaging in self-harm (Gilbert, McEwan, Irons, Bhundia, Christie, Broomhead, Rockcliff, (2010)). Both Gilbert’s and Neff’s measures have never been tested on a clinical population of patients experiencing persistent treatment resistant depression and thus it is unknown whether these measures perform well in this clinical population.
In addition, there is variation in the degree of established validity and reliability amongst the shame measures cited in the literature, the majority of which have only been tested on student populations. Whilst three shame measures stand out as contradicting this last statement, (The Test of Self-Conscious Affect-3 (TOSCA-3) (Tangney, Dearing, Wagner and Gramzow 2000); Internalised Shame Scale (ISS) (Cook 1996) and The Experience of Shame Scale (ESS) (Andrews, Qian and Valentine 2002) which have been tested on a clinical population, each of these are underpinned by a different shame theory to the one being tested in this study. Therefore, concurrent validity was not tested by comparing the study measures (OAS; FSCRS and SCS) to any other measures as no equivalent measures have to date been developed.
Step 2: Modelling variance in depressive symptoms against shame, self-criticism and selfcompassion
Researchers in the field of Self-conscious emotions (Gilbert, 2017a; 2007a; Tracy and Robins 2007; Neff, 2003a) argue that shame and self-criticism and low self-compassion are trait psychological constructs that may contribute to the maintenance of emotional disorders. However, it is possible to argue that rather than these representing trait psychological constructs that contribute to such a maintenance process, shame and self-criticism and low self-compassion are, in fact, nothing more than symptoms of severe and persistent low mood which will remit in line with improvement in severity of depression.
In considering these two hypotheses this PhD study used the data collected from the OAS, FSCSR and SCS, correlated with measures of depression, to model variance in depression in a clinical population of participants experiencing persistent, treatment resistant depression. This data was used to test the construct validity of Gilbert’s model of shame, self-criticism and self-compassion in depression.
The questionnaires used to measure levels of depression were:
-
The 17 item Hamilton Depression Rating Scale (HDRS-17) (Hamilton, 1960).
-
Beck Depression Inventory-I (BDI-I) (Beck, Ward, Mendelson, Mock and Erbaugh 1961).
-
Patient Health Questionnaire-9 (PHQ-9) (Kroenke, Spitzer and Williams, 2001).
Rationale for chosen measures of depression
The BDI-I, PHQ-9 and HDRS-17 have been chosen due to their well-established reliability and validity as measures of depressive symptomatology (Williams, Kobak, Bech, Engelhardt, Evans, Lipsitz, Olin, Pearson and Kalali, 2008; Lowe, Spitzer, Grafe, Kroenke, Quenter, Zipfel, Buchholz, Witte and Herzog, 2004; Beck, Steer and Garbin 1998). The BDI-I and PHQ-9 are self-report measures, whilst the HDRS-17 is an interviewer rated measure. Using both types of measure will help mitigate the weaknesses of both forms of measurement (self-report and interviewer rated) and will allow comparison of the parameters of the severity of depression in the study sample as defined by these measures. In addition, the PHQ-9 and HDRS-17 each measure slightly different depression related phenomenon in comparison to the BDI-I, with the BDI measuring more cognitive symptoms and the HDRS-17 and PHQ-9 more somatic symptoms. The use of each of these measures enabled comparison of the modelling of variance taking into consideration cognitive symptoms and somatic symptoms.
As outlined earlier, Kim, Thibodeau and Jorgensen (2011) highlight the issue that measures of depressive symptoms which include questions which may tap feelings of shame i.e. worthlessness may inflate the association between shame and depression resulting in a conflation of the two constructs. Both the HDRS-17 and BDI-I refer to the construct of shame. In the HDRS-17 item 2 ‘Guilt’ prompts the interviewer administering the scale to probe for feelings of shame. In the BDI-I item 7 asks the respondent to rate:
0 = I don’t feel disappointed in myself; 1 = I am disappointed in myself; 2 = I am disgusted with myself; 3 = I hate myself. The themes of self-disgust and self-hatred are central to definitions of shame (e.g. Gilbert 2010b; Tangney and Dearing 2002).
The BDI-I also includes a question on self-criticism and self-blame (item 8) and once more the same issue regarding inflation of association between shame and depression may arise. Kim, Thibodeau and Jorgensen (2011), encourage the researcher to address the potential issue of inflated effect size by using depressive symptom scales that eliminate the overlap with selfevaluative processes thought to characterise shame. Taking this issue into consideration the inclusion of the PHQ- 9 offers potential for some mitigation against this potential for inflation of association between shame and depression.
The PHQ-9 has one item (item 6) which appears self-evaluative and asks the respondent to rate the degree to which they ‘feel bad about themselves, are a failure, or have let themselves or others down’. This item is seeking to tap into feelings of guilt. The other eight questions all clearly relate to somatic symptoms of depression. Both the PHQ-9 and HRSD-17 are constructed as a measure of somatic symptoms of depression and their conceptual foundations are the diagnostic criteria for major depressive disorder (i.e. American Psychiatric Association (APA, 1994). In this respect (as with item 2 on the HDRS-17) item 6, which refers to feelings of guilt, is conceptualised not as a self-evaluative psychological construct, but within the frame of diagnosis, as a somatic symptom related to mood. Kim, Thibodeau and Jorgensen (2011) in their meta-analytic review argue that whilst it is important to be mindful of the possibility of inflated effect sizes, they do not believe the issue detracted significantly from their findings as the items represent only a small part of the entire item set in the questionnaires they reviewed and therefore this is unlikely to inflate effect sizes to any great extent.
An overview of each depression measure
Hamilton Depression Rating Scale-17 (HDRS-17)
The HDRS-17 (Hamilton 1960) (see appendix XV) is, in its original form, a 21-item clinician rated questionnaire that measures severity of depression. Cusin, Yang, Yeung and Fava (2010) note that in developing the scale, Hamilton indicated that the last four items on the scale (diurnal variation, depersonalisation/derealisation, symptoms of paranoia and obsessivecompulsive symptoms) should not be included in the total score as these symptoms are either uncommon or, are not usually a reflection of depressive severity. As a result, it is standard practice in clinical trials to use the 17-item version of the questionnaire. This scale is one of the most widely used depression severity measures in clinical trials (Williams, Kobak, Bech, Engelhardt et al, 2008). There is a guide to administering the scale (Williams 1988), developed in order to improve inter-rater reliability and which is widely considered the best resource for training purposes in clinical trials. Bagby, Ryder, Schuller and Marshall (2004) reviewed 70 studies published since 1979 examining the psychometric properties of the HRSD-17 and concluded that most items on the scale show adequate reliability. Cusin, Yang,
Yeung and Fava (2010) report that inter-rater reliability is very high for total scores (0.800.98). They observe inter-rater reliability on some items is poor but, when used in conjunction with the interview guidelines all items demonstrated adequate reliability. In addition, the
HDRS-17 shows high test-re-test reliability when used with the structured interview guide (Williams, 1988) and validity has been shown to range from 0.65–0.90 with global measures of severity of depression (Bagby, Ryder, Schuller and Marshall, (2004)).
Each of the 17 items is scored on a Likert scale of severity with anchors for symptom absent, through to mild, moderate and severe. The total score is obtained by adding together the score for each item and on the 17 item version scores can range from 0–54. The accepted cut off scores are as follows:
0–6: no depression present
7–17: indicative of mild depression
18–24: indicative of moderate depression
24 and over: indicative of severe depression
A total score of 7 or less is usually the accepted indicator of remission of depressive symptoms and a reduction from baseline score of 50% or more during treatment is considered indicative of a clinical response to treatment (Cusin, Yang, Yeung and Fava (2010).
Beck Depression Inventory-I (BDI-I)
This study used the Beck Depression Inventory version I (BDI-I) (Beck, Ward, Mendelson, Mock and Erbaugh 1961) (see appendix XVI). The BDI-I is a 21 item self-report measure of the severity of depressive symptoms as judged by the respondent at the point at which they are completing the questionnaire. Beck, Steer and Garbin, (1988), reporting on the psychometric properties of the BDI-I conducted a meta-analysis of all psychometric studies conducted on the BDI-I between 1961–1986 and reported a mean coefficient alpha score of 0.86 for participants with a psychiatric diagnosis. Further, in the same meta-analysis it is reported that in a group of psychiatric patients the mean correlations with the HRSD-17 were 0.73 (Beck, Steer and Garbin, (1988)).
Each item is rated on a 4-point Likert scale of 0–3 from absence of symptoms, through to mild, moderate and severe levels of depression. The total score is obtained by adding together the score for each item and on the BDI-I scores can range from 0–63. The accepted cut off scores for the BDI-I are as follows:
0–9 absence of depressive symptoms
10-19-mild level of depressive symptoms
20-25-moderate level of depressive symptoms
25 and above severe level of depressive symptoms
A total score of 8 or less is considered indicative of remission of depression.
The Patient Health Questionnaire (PHQ-9)
The Patient Health Questionnaire (PHQ-9) (Kroenke, Spitzer and Williams, 2001) (see appendix XVII) is 9 item self-report measure of the severity of depressive symptoms as judged by the respondent at the point at which they are completing the questionnaire.
Each item is rated on a 4-point (0–3) Likert scale from absence of symptoms, through to mild, moderate and severe levels of depression. This is defined in terms of the number of days each symptom has been present for the last week from, ‘Not at all to several days, more than half the days or nearly every day’. The total score is obtained by adding together the score for each item and the overall score can range from 0–27. The accepted cut-off scores for the PHQ-9 are:
0–4 minimal depression
5–9 mild depression
10–14 moderate depression
15–19 moderately severe depression
20–27 severe depression
Step 3: Exploring patients lived experience of shame, Self-criticism and self-compassion Procedure for quantitative data collection
The six measures described above were administered as part of a battery of measures used within the RCT. These were administered to all 187 participants recruited to the trial at baseline on entering the trial, then at 6, 12 months, 18 months and 24 months. In the Cambridge site the OAS was not administered. As stated previously, the measures were administered by the trial research associates and in the Cambridge site the OAS was inadvertently omitted from the battery of measures administered.
To establish the reliability and validity of the OAS; FSCRS and SCS the data collected at baseline were used alongside the data from the healthy control sample.
To model variance in depressive symptoms participant baseline total scores on the HRSD-17; BDI-I and PHQ-9 and the OAS; FSCRS and SCS were used.
As the PhD candidate was the clinical lead for the service being evaluated in the RCT and a treating clinician within the service this data was collected by the trial research associates and not the PhD candidate. This strategy was a prerequisite of the trial requirements as the treating clinicians needed to be blind to the scores on the psychometric measures of participants randomised to the treatment arm of the study as this may have influenced how treatment was delivered. In addition, a proportion of the participants randomised to the treatment arm had the PhD candidate allocated as their trial CBT therapist. Once a sustained therapeutic relationship forms between participant and therapist (the PhD candidate) asking participants to complete study measures may introduce bias in terms of how the participant completes the questionnaire. For example, the participant may feel it is important to please the therapist and demonstrate that therapy is leading to improvement (even when it is not) and therefore lower their endorsements on the measure as a reflection of this need to please and not as a result of genuine symptom improvement. See Burman (1994) for a full discussion of the research dilemmas posed by these issues.
Description of Qualitative Data Collection Method
The qualitative component of the study aimed to obtain first-hand accounts of participants lived experience of depression. This data was collected by the PhD candidate, via a 90-minute semi-structured interview. The content of the semi-structured interview explored:
-
Participants’ lived experience of depression, shame, self-criticism and self-compassion
-
Whether participant’s descriptions of depression, shame, self-criticism and selfcompassion resonated with Gilbert’s theoretical definitions of these trait psychological constructs.
A pre-prepared interview guide was developed to maintain consistency across interviews as to the structure and focus of questions asked to each participant (see appendix XVIII). The semi-structured interview was grounded in the theoretical principles of qualitative data analysis method used in this PhD thesis, Interpretative Phenomenological Analysis (IPA) (Smith, Flowers and Larkin, (2009)), who argue that IPA is especially well suited to exploring psychological constructs (Smith, 1996). In this regard questions were structured using the format proposed by (Smith, Flowers and Larkin, (2009) in order to maximise opportunities for accessing in rich, detailed and nuanced testimonies of participants lived experience of depression, shame, self-criticism and self-compassion. This structure adapted from Smith, Flowers and Larkin (2009), p 60) is reproduced in table 5 below. The aim is to develop an interview process that moves through a sequence starting with narrative and descriptive questions, then moving through analytic and evaluative questions. An overview of this process with exemplar questions is shown in Table 5. Unsurprisingly, given IPA is derived from the discipline of clinical psychology, this process mirrors the questioning style used in psychological therapies, notably CBT (see Kinsella and Garland, 2008). Questioning style should focus on asking open questions that do not make assumptions about the respondent’s experiences and do not lead them towards certain answers.
TABLE 5: TYPES OF QUESTIONS FOR IN-DEPTH INTERVIEWS
| — | Descriptive – Please can you tell me your first experience of depression? |
| • | Narrative — Please can you tell me how depression affects you on a day to day basis? |
| • | Structural- So what do you say to yourself when you make a mistake? |
| • | Contrast -What is the differences between compassion for others and compassion for Yourself? |
| • | Evaluative- How do you feel when you recall your childhood? |
| • | Circular- How do you think others view you when your mood is depressed? |
| • | Comparative- How do you think you might feel if you were kinder to yourself? |
| • | Prompts- Can you tell me a bit more about that? |
| • | Probes-what do you mean by ‘idiot’? |
Quantitative data analysis
The demographic characteristics of the sample are reported using descriptive statistics. This includes frequencies, proportions, means, medians and 95% confidence intervals. The sample who consented to participate in the RCT (n=187) did not represent the whole sample recruited to the study as some participants who were recruited did not go on to consent to take part in the study as they chose to withdraw prior to giving consent (see appendix VII for a consort diagram of participant flow through the RCT). Therefore, differences in the characteristics between those who consented to participate and those who did not was examined using chi-square statistics.
The psychometric evaluation of reliability and validity of the chosen measures was tested by conducting the following statistical analyses in the order stated:
-
Test-retest Reliability
-
Internal Consistency
-
Factor Analysis
Establishing reliability and validity of the OAS, FSCR and SCS
The first step in the data analysis was to establish the reliability and validity of the OAS, FSCRS and SCS.
Defining reliability
Reliability in relation to questionnaires has two facets:
-
Whether or not a specific measure obtains similar results when it is repeated using the same sample.
-
Whether or not there is consistency among the questions posed because all the questions relate to the construct under investigation and therefore it is reasonable to expect the answers to have consistency.
Defining validity
Assessing the validity of a given measure aims to determine whether the measures under investigation measure what they were designed to measure. Haynes, Richard and Kubany (1995) observe that the purpose of validating measures is to:
‘gather evidence about the utility, domain, facets, boundaries and predictive efficacy of a
construct’
(Haynes, Richard and Kubany, 1995, p 240).
Testing reliability
In order to test the reliability for the OAS, FSCRS and SCS the statistical analysis test-retest reliability was calculated using the correlation coefficient Cronbach’s alpha on data collected at the baseline and 6 months data collection points. A high correlation coefficient indicates high reliability. Statistical analysis recommends the minimum sample size required for establishing test-retest reliability is 100 participants (Kline, 2000) and in this PhD study the sample size was 187 for each measure except the OAS for which there was a sample size of 158.
There is no agreed standard time interval advocated between the two testing points, although there is some consensus in the literature (Maltby, Williams, McGarry and Day, 2010) that a period of 2–3 months is optimum. The issue of relevance in considering the time interval is gaining a balance between the test-retest period being too short and the possible introduction of practice effects in which the participants may remember responses previously given and the time interval being too long leading to skewed results. In considering the latter, if the time interval is too long changes in the Cronbach’s alpha scores may be accounted for by other factors such as participant maturation rather than, as test-retest aims to establish, instability of the measures being administered.
In this PhD study the test-retest period was 6 months. The reason for this is that the PhD is part of a larger RCT and this was the subsequent data collection point following baseline assessment as agreed within the trial. Whilst this may seem to introduce a flaw in the PhD study design, two points can be made to counter this. Firstly, in testing Gilbert’s formulation, he conceptualises shame, self-criticism and self-compassion as trait rather than state phenomenon (Gilbert, 2017a; 2007a) and the OAS and FSCRS as tapping trait psychological constructs. In considering Gilbert’s model that high levels of shame, self-criticism and low levels of self-compassion are implicated in the persistence of depression and that he conceptualises these factors as trait phenomena then in this regard it would be anticipated these traits would be stable over an extended time period and are unlikely to change significantly over a 6-month period. Even allowing for the fact that shame, self-criticism and self-compassion may be targets for treatment as part of the interventions offered in the Specialist Depression Service (the active treatment arm of the RCT) over the 12-month period the interventions were delivered the first six months of treatment was focused on engagement and amelioration of somatic symptoms of depression. Therefore, no direct psychotherapeutic intervention would have been made in the first 6 months of treatment to target the psychological constructs of shame, self-criticism and self-compassion. On this basis it can be argued the 6-month test retest time period has cogency in this context as a test of the reliability and stability of the measures over time.
Testing validity
In order to establish the validity of a psychometric measure it is first necessary to establish the level of internal consistency of each measure.
Internal consistency
Internal consistency seeks to establish the degree to which the scores given by participants are consistent throughout a whole test. This is considered an essential component in determining the strength of the psychometric properties of a measure. The internal consistency of the OAS, FSCRS and SCS was investigated by calculating Cronbach’s alpha coefficient scores of the items in each individual scale in relation to each other. Once more the recommended sample size is 100 and a correlation of 0.7 or more is considered reliable and acceptable (Kline 2000).
The following tests of validity were carried out:
Face validity: Establishing face validity is the process by which the individual items on a specific measure are examined to assess whether the tool is measuring what it aims to measure. High face validity can influence participants’ willingness and interest in completing the measure. However, some measures deliberately incorporate low face validity into their design in order to disguise the true nature of the test.
Content validity: Haynes, Richard and Kubany (1995) state that determining content validity is an important component of establishing construct validity as it provides information about the degree to which the factors in the measure are relevant to and representative of the construct under investigation. In this definition the authors define the factors in the measure as encompassing all aspects of the measurement process including the individual factors themselves, the response format and the instructions given. Further they define the relevance of a measure as the appropriateness of its constituent factors for the construct being measured. Meanwhile the representativeness of a measure refers to the degree to which the factors are proportional to the facets of the construct being measured. An important consideration in the area of content validity is how precisely the construct is defined and the degree to which experts in the area under investigation (i.e. shame, selfcriticism and selfcompassion) agree about the domain and the facets of the construct.
Construct validity: Construct validity is always theory dependent and is a necessary condition for theory development and testing (Peter, 1981). Cronbach and Meehl (1955) define constructs as non-observable, non-real entities and constructs along with their theories are viewed as tools of scientific enquiry, the adequacy of which is judged based on their usefulness in making observable predictions. Kaplan (1964), (cited by Maltby, Williams, McGarry and Day (2010)), states that constructs have two forms of meaning:
Systemic: referring to the interpretation of what a construct represents depends on the theory in which the construct is embedded
Observational: referring to the idea that a construct must be capable of being directly or indirectly operationalised if it is to be used to give explanatory power. A measure represents the operationalisation of the construct under study.
Westen and Rosenthal (2003) observe that construct validity refers to the extent to which a measure adequately assesses the construct it claims to assess. According to Peter (1981) a measure has construct validity based on two criteria:
1. The degree to which the measure assesses the magnitude and direction of a representative sample of the characteristics of the construct
2. The degree to which the measure is not contaminated with elements from other constructs or error
In this regard construct validity cannot be directly measured but rather only inferred when the measure scores (variance) perform as psychometric theory states they should perform. Thus, if a construct was deemed to possess three dimensions then a factor analysis of a measure purporting to measure that construct which produces three meaningful factors could be used as evidence of the measure possessing construct validity.
Finally, Confirmatory Factor Analysis (CFA) was conducted to establish the psychometric properties of the OAS, FSCRS and SCS tested on a cohort of participants diagnosed with persistent, treatment resistant depression.
Modelling variance of depression in relation to shame, self-criticism and self-compassion
Step 2 of this PhD study aimed to model variance between level of depression and shame, self-criticism and self-compassion. The statistical method that was used to model variance was univariate and multivariate regression analysis. Regression analysis is used to observe trends in relationships between two variables a dependent and an independent variable.
Multiple regression analysis is used where there is more than one independent variable. In this instance depression is the dependent variable and shame, self-criticism and selfcompassion are the independent variables. In this PhD study multiple regression analysis was deployed in order to model variance at baseline, between shame, self-criticism and selfcompassion and level of depression within the study cohort. This analysis of variance will test the construct validity of Gilbert’s theory of the role of shame, self-criticism and selfcompassion against the notion that high levels of shame and self-criticism and low levels of self-compassion are symptoms of depression which fluctuate according to level of depression.
Qualitative data analysis
The method used to analyse the qualitative data was Interpretative Phenomenological Analysis (IPA) (Smith, Flowers and Larkin 2009; Biggerstaff and Thompson 2008). This methodology was chosen over grounded theory (Glaser and Strauss 1967) as IPA is best suited to test a construct that has already been established, whereas grounded theory is better suited to the process of defining a new construct. The constructs being investigated in this PhD study (shame, self-criticism and self-compassion) have already been established and defined by Gilbert’s theory (Gilbert 2017a; 2016; 2007a).
The steps in the qualitative data analysis were: (see Smith, Flowers and Larkin (2009)):
-
Transcribing the interviews.
-
Round 1 analysis of each individual transcript adding initial comments.
-
Round 2 analysis identification of themes and categories within each individual transcript using a mind map format.
-
Round 3 analysis identification similarities and differences in themes and categories across all 10 transcripts.
-
Checking these themes with others.
-
Generating a small set of generalized themes.
-
Identifying where these themes are convergent and/or divergent with Gilbert’s theory.
The data from the quantitative and qualitative arms of the study was compared to observe similarities, differences and identify emerging themes. These were then interpreted as a whole to address the research questions posed at the outset of the study.
An overview of Interpretative Phenomenological Analysis
Interpretative Phenomenological Analysis (IPA) aims to explore processes by which participants make sense of their experiences. This exploration involves harnessing the participants’ capacity for self-reflection through a verbal process aimed at eliciting their understanding, thoughts and views about how they make sense of these experiences. Pauley and McPherson (2010) emphasise that IPA focuses on the participant in context and aims to explore their relationship to and understanding of the phenomena under investigation. Thus, the researcher is seeking to understand how participants make sense of their experiences in terms of how they relate to and understand these phenomena. Importantly the aim in this method is to articulate subjective (as opposed to objective) accounts of their idiosyncratic experiences in the area under study.
Thus:
‘In IPA research, our attempts to understand other people’s relationships to the world are necessarily interpretative, and will focus upon their attempts
to make meanings out of their activities and to things that
happen to them’
(Smith, Larkin and Flowers, 2009 p. 21).
According to Brocki and Wearden (2006) the researcher is trying to enter the participants’ personal world, whilst simultaneously acknowledging that the accessing of this world is dependent on and complicated by the researchers own perspective and assumptions. Thus, the researcher is aiming to establish a process of interpretative activity and the account produced in this endeavour constitutes the joint reflections of the participant and the researcher. Thus, in IPA the interpretations made are bound by the participants ability to selfreflect and adequately articulate their perceptions, experiences and viewpoints and simultaneously on the researcher’s capacity to adequately reflect and analyse. Pauley and McPherson (2010) observe that the process of acknowledging the researcher’s beliefs enables IPA research to elicit new information in relation to existing theoretical positions from the perspective of the lived experience of the participant.
The argument for epistemological coherence: The Primacy of Praxis revisited
Within the IPA literature there are a plethora of justifications within individual studies for the utilisation of IPA in combination with other methods of data collection and analysis (see Brocki and Wearden 2006 for a review). Based on the tenants of IPA articulated in this thesis a question arises of how this method of data collection and analysis can be utilised within in a mixed methods design rooted in the epistemological position of the ‘primacy of praxis’ articulated above.
Smith, Larkin and Flowers (2009) observe that phenomenology is a pluralist endeavour (p 12) that does and should connect with our everyday experience (p 32). The authors also argue that the process of attending to and reflecting upon our own experiences is intrinsic to being human and that phenomenology is ‘a live, dynamic activity, not just a scholarly collection of ideas’ (p 33) and is concerned with lived experience. In the context of research, Smith, Larkin and Flowers, (2009), developed IPA in a healthcare setting. As such, their stated aim appears to be to develop a qualitative research method of practical utility in not only investigating the lived experience of people who come into contact with healthcare professionals but to use the data generated in such research to develop treatments and improve healthcare services.
Inherent to this articulation of IPA is the central tenant of the philosophy of Pragmatism, the ‘Primacy of Praxis’, as expounded earlier in this chapter, that is, Hetherington’s (2006) definition of knowledge in terms of agency, as a process of acting in the world and Hookway’s (2006) exposition of ‘epistemology as a theory of inquiry’ (p 98). Within the philosophy of Pragmatism, reasoning and inquiry are goal directed and problem-solving activities are inherent in and of themselves and these facets are implicit in the Smith, Larkin and Flowers
(2006) exposition of the role and purpose of IPA as a research method in healthcare. Interestingly, Chamberlain (2011) offers a critique of IPA, in which she strongly argues that its epistemological underpinnings lack philosophical rigour. To quote:
‘IPA may be considered wanting in its attempts to provide suitable commentary and discussion on how IPA, as a methodology for inquiry, can deliver a distinctive analysis that sets it clearly apart from other qualitative analysis methodologies, such as thematic analysis or grounded theory, and identifies it as specifically phenomenological and interpretative’ (Chamberlain 2011 p 51).
Chamberlain’s assertion seems to typify the research paradigm debates that are highlighted by Bestia (2010) and which course through and between both academic and professional disciplines. Placing practical utility imbued with agency at the heart of reasoning and viewing this as a process of inquiry, in the minds of some, lacks logical consistency because it neglects the process of assessing the veracity of the beliefs that emerge from this inquiry. Healthcare and its delivery are predicated on action and the epistemology of the ‘Primacy of Praxis’ within a mixed methods design offers perhaps the only viable process by which healthcare research can be conducted.
Ethical considerations
All researchers are bound by a duty of care which compels them to uphold the ethical principles enshrined within the 2000, Declaration of Helsinki, (World Medical Association (WMA), 2004). These include a directive to do no harm; promote good; to guard the rights of the participant above all other considerations (examples would be preserving confidentiality; facilitating informed consent; preserving the right to withdraw from research; in an RCT providing participants in TAU group access to interventions tested in the active treatment arm if proved to be of benefit) and for the researcher to act at all times with honesty and integrity in a non-coercive manner. History catalogues numerous human rights violations carried out in the name of research and consequently researchers are governed by a rigorous set of ethical codes of conduct for research. Ones of relevance here are cited below. As part of her research training the PhD candidate undertook the National Institute of Health Research
(NIHR) Principles of Good Clinical Practice in Research, a one-day training event (NIHR, 2011). The professional practice of the PhD candidate is governed by two codes of ethical conduct both of which include research as a component. These are the Nursing and Midwifery Council
(NMC) Code of Conduct (2018) and the British Association of Behavioural and Cognitive Psychotherapies (BABCP) Standards of Good Practice (2017).
The following section briefly describes how this PhD study assured ethical governance of:
-
Data management
-
Confidentiality of participant information
-
Informed consent
-
Fieldwork and safety guidelines
This information is précised from the RCT study protocol version 9 (Morriss, 2012).
Data Management
The PhD candidate was bound to adhere to the Data Protection Act (DPA) (1998) and ensure the rights of the study participants to privacy and informed consent were upheld at all times.
In addition, there was an undertaking that each participant’s research file only contained the minimum required information for the purposes of the study and that this information was held securely in a locked facility. Electronically stored data, including the trial database, was stored securely on a dedicated web server, on a password protected computer at both the University of Nottingham and Nottinghamshire Healthcare NHS Trust. Access to this data was restricted by user identifiers and passwords. Electronic data was backed up every 24 hours to both local and remote media.
Confidentiality
The clinical information of individual participants obtained in the course of the PhD study was considered confidential and disclosure to third parties was prohibited with relevant exceptions related to maintaining participant welfare. Participant confidentiality was further ensured by utilising identification code numbers to correspond to treatment data in the computer files. This medical information could be shared with the participant’s medical team and all appropriate medical personnel responsible for the participant’s welfare where deemed necessary. Data generated as a result of the trial is available for inspection on request by the participating clinicians, the University of Nottingham representatives, the Trent Research Ethics Committee (REC) (Trent REC reference for the RCT #:09/H0405/42 (Morriss, 2012) and Nottinghamshire Healthcare NHS Foundation Trust Research and Development Centre.
Process for obtaining informed consent
The process for obtaining informed consent from the participants was in accordance with the
Health Research Authority (HRA, 2015); the Good Clinical Practice (GCP) Guidance (NIHR,
2011) and the University of Nottingham Code of Research Conduct and Research Ethics
(2013a). When obtaining written consent, the research associate/PhD candidate and the participant both signed and dated the relevant informed consent form before the participant could engage in the RCT. One copy of the consent form was kept by the participant, one by the research associate and one was placed in the participant’s hospital records. Consent was obtained for the conducting of research assessments as follows:
-
At each quantitative data collection point
-
For participation in the two interventions offered in the RCT (SDS or TAU)
-
For collection of data from healthy controls
-
For taking part in qualitative data collection interviews, including audio recording and transcription of interviews and use of anonymised quotations from these interviews in subsequent publications.
Three separate consent forms were used in this PhD study for quantitative data collection for RCT participants and for the healthy controls and for qualitative data collection for the PhD study participants. Due to word restrictions in this PhD thesis only one exemplar of a consent form is given, that of healthy controls, (see appendix XI). The wording on each consent form was modified to meet the needs of the consent process for the specific assessment taking place.
Participants were informed that the decision to participate in the study was entirely voluntary and it was explained that they could withdraw consent to participate at any time without penalty and that such a decision had no bearing on their current or future health care or benefit claims. Participants were informed that in the event of withdrawal from the RCT any data already collected could not be erased and would likely be used in the final data analyses.
Fieldwork and safety guidelines
University of Nottingham (2013b) Policy and Guidance for the Safe Conduct of Fieldwork were followed in all areas of participant recruitment, assessment and treatment. Where necessary a risk assessment was performed to assess whether a participant was safe to be interviewed unaccompanied or accompanied at home or at a health service base. Procedures were put in place for the safe management of participants.
Ethics Approval to conduct this research
Ethics approval for the PhD study was sought and granted as part of the CLAHRC-NDL RCT. As cited in the CLAHRC-NDL Mood Disorder Trial Protocol (Morriss 2012) the RCT was subject to Multi Centre Research Ethics Approval and local Trust research governance approval in each study site. In Nottingham this was the Trent Research Ethics Committee (REC), (Trent REC reference for the RCT #:09/H0405/42 (Morriss, 2012)) and Nottinghamshire Healthcare NHS Foundation Trust Research and Development (R&D) Centre. In keeping with the trial protocol, the candidate succeeded in securing a protocol amendment from the local Research Ethics Committee (REC) in order to recruit the 30 healthy participant controls required for the PhD study. The CLAHRC-NDL RCT and the PhD study was conducted in accordance with the ethical principles that have their origin in the Declaration of Helsinki (2000) (WMA, 2004), the National Institute of Health Research (NIHR) Principles of Good Clinical Practice (2011), and the Department of Health (DoH) Research Governance Framework for Health and Social Care, (2005).
Chapter 4 Quantitative Results
Introduction
This chapter presents the quantitative results of this PhD study. The chapter begins with a summary and brief definition of the descriptive and then inferential statistical analyses deployed. This is followed by description of the study cohort and its baseline characteristics.
The statistical analysis from the quantitative data collection process is then reported.
The quantitative data for each scale is presented in the following order OAS; FSCSR and SCS.
The statistical data reported to answer the study questions are as follows:
Question 1: To test the psychometric properties of the OAS, FSCSR and SCS in a cohort of patients diagnosed with persistent, treatment resistant depression:
1. Descriptive statistics
The following descriptive statistics are reported here:
I. Demographics of the study cohort
II. Descriptive statistics for each subscale on each measure and total with mean standard deviation for normally distributed variables and median and interquartile range for skewed variables.
III. Item level descriptive statistics
IV. Item-item correlation
V. Correlations among sub-scales and totals
2. Inferential statistics
I. Reliability
The reliability of the OAS, FSCSR and SCS was tested using Cronbach alpha for each sub-scale and total score, split half and test-retest. Cronbach alpha was used to measure the internal consistency of each scale i.e. how closely the items in each scale are related. Split half reliability was used to assess the internal consistency of each scale. Split half measures the degree to which all parts of the test contribute equally to what is being measured. This was executed by taking each scale in turn and comparing the results from one half of each scale with results from the other half of each scale. Test-retest reliability was used to test the external consistency of the OAS, FSCSR and SCS. Test-retest reliability assesses the stability and precision of a construct across time i.e. between baseline and a predetermined post-test time point. If the scores derived at both time points are highly correlated with stable scores and error variances across time, then evidence of test-retest reliability is present. When interpreting correlations in test-retest reliability if the p- value is less than 0.05 and the Pearson’s coefficient is above 0.7 this is indicative of test-retest reliability. If the p-value is greater than 0.05 or the Pearson’s correlation coefficient is below 0.7 then there is no evidence of test-retest reliability.
ii. Validity:
Confirmatory Factor Analysis (CFA) was used to test apriori hypotheses about the relationships between observed variables or indicators (items on a measure) and continuous latent variables (the factors under investigation). CFA was used to assess the correlation between the observed variables and their associated continuous latent variables to test the construct validity of the OAS, FSCSR and SCS. The aim being to assess the degree to which the theoretical model underpinning each measure was supported by the data sample, i.e. making estimations of the relationships between the factors. This is referred to as model fit and the statistics literature reports several indices for assessing this (Cangur and Ercan 2015; Jackson, Gillaspy and Purc-Stephenson 2009; McDonald and Ho 2002). This literature was used to guide the interpretation of the statistical analysis presented here. This decision is justified on the grounds that the chosen literature reflects a degree of consensus regarding indices for interpreting statistical data.
Model fit was assessed using the following indices: chi-square goodness- of -fit test (𝑥2),
Comparative Fit Index (CFI), Tucker Lewis Index (TLI) and Root Mean Square Error of Approximation (RMSEA) (Schreiber, Stage, Nora, Barlow and King, 2006). Non-significant 𝑥2 generally indicates the model does not fit the data well, however, 𝑥2test is sensitive to nonnormal data and large sample size, hence in this study, 𝑥2 test together with CFI, TLI and RMSEA was used to assess approximate model fit. For CFI, TLI and RMSEA (Hu and Bentler, (1999)) recommend a cut-off point of <0.8 as indicative of an excellent fit with 0.10 acting as an upper limit.
In this chapter the CFA results for the OAS, FSCSR and SCS are reported below as individual scale specific CFA plot diagrams, alongside the model fitting indices for each scale. The CFA pathway diagrams for the OAS, FSCSR and SCS show the correlations between the factors in each measure.
Question 2: To examine the degree to which variance in scores on depression measures taken at baseline can be accounted for by variance in levels of shame, self-criticism and selfcompassion
I. Univariate and multivariate regression analysis
Univariate and multivariate regression analysis was used to address question 2 of this PhD thesis. Univariate regression analysis involves the analysis of one dependent variable against one independent variable. Multivariate regression analysis involves the analysis of one dependent variable against two or more independent variables and is a form of inferential statistics which models the relationship between a response variable and one or more predictor variables. For a useful summary of the principles of regression analysis see Frost (2019) and Zeltzer, (2016; 2013; 2011).
The qualitative data is presented within the framework of the Interpretative Phenomenological Analysis (IPA) (Smith, Flowers and Larkin 2009) using a method devised by the PhD candidate and presented in chapter 5 of this thesis.
The demographic profile of the study cohort
The study recruited 187 participants in total. Table 6 (p 135) describes the demographic characteristics of the study cohort at baseline. Complete demographic data was collected on 97% of the cohort. The cohort had a mean age of 46.5 years (range 20–84 years). Within the sample 61% of the participants recruited were female and 39% male.
With regard to employment status, 40.5% of the cohort were unemployed whilst 22.5% were in full-time employment. A further 14.5% were engaged in other employment which, for the purpose of data collection, was defined as, part-time work, sheltered or voluntary work or engagement in higher education. A large proportion of the cohort (68.5%) were in receipt of benefits at baseline. With regard to relationships 49% were married or co-habiting with a partner and 64% had one or more children.
Across the cohort 86.5% had been depressed for more than 12 months. The mean number of years since first diagnosed with depression was 16.7 (range 0.5–49 years) and the median 11.5 (range 0.5–49). Means for the baseline scores on psychometric measures of depression used in the study are reported in Table 7 below (p 136), which can be summarised as follows: Mean score on the HDRS-17 22.6 indicative of a moderate level of depression, (range of scores in this sample, 16–40); BD-I 33.6, indicative of a severe range of depression, (range of scores in this sample, 16–56) and PHQ-9 19.6, indicative of a moderate-severe level of depression (range of scores in this sample 5–27).
Table 8 (p 137) shows the secondary clinical characteristics of the study cohort at baseline. This analysis shows data on the psychiatric and physical health comorbidity of the sample, as well as the presence of depressive recurrence. In summarising the contents of table 8: 179 (95.7%) of the cohort at baseline met diagnostic criteria for a unipolar major depressive episode and 156 (83.4%) reported at least one previous major depressive episode, with 105 (56.1%) reporting melancholia. Further, 146 (78.1%) reported a co-morbid anxiety disorder (the most common of which were panic disorder or agoraphobia 86 (46.2%) and generalised anxiety disorder 85 (45.7%) and 120 (64.2%) of the cohort reported a currently active physical illness.
TABLE 6: DEMOGRAPHIC CHARACTERISTICS OF THE STUDY COHORT AT BASELINE
| Variable | Study cohort (n=187) |
|
Age Mean in years (range) |
46.5 (20–84) |
|
Gender Female (%) Male (%) |
114 (61%) 73 (39%) |
|
Employment status n (%) Full-time employment Other employment[1] Retired unemployed |
[n=181] 39 (22.5%) 21 (11.5%) 26 (14.5%) 73 (40.5%) |
| Receiving benefits n (%) |
[n=181] 124 (68.5%) |
|
Education n (%) Before age 16 Up to age 18 or apprenticeship Highest qualification-A level |
Highest qualification degree or postdegree | [n= 187]
10 (5%)
81 (43%)
40 (21%)
56 (30%) | Relationship status n (%) single
Married
Co-habiting
Divorced
Separated widowed
| [n=187]
46 (22.9%)
81 (43.3%)
10 (5.3%)
33 (17.6%)
9 (4.8%)
6 (3.2%) |
| Children 1 or more n (%) | 119 (64%) |
TABLE 7: PARTICIPANTS CLINICAL CHARACTERISTICS OF DEPRESSION AT BASELINE
|
Variable |
Study cohort (n=187) |
|
Years since first diagnosed with depression (mean, Sd, range) |
16.7 (11.3, 0.5–49) |
|
Years since first diagnosed with depression (median range) |
11.5 (0.5–51) |
| Depressed >12 months n (%) | 81 (86.5%) |
| BaselineHRSD-17 (mean, range) | 22.6 (16–40) |
| Baseline BDI-I (mean, range) | 33.6 (16–56) |
|
Baseline PHQ-9 (mean, range) |
19.6 (5–27) |
TABLE 8: SECONDARY CLINICAL CHARACTERISTICS OF THE STUDY COHORT AT BASELINE
| Characteristic | Number (%) | |
| Current unipolar major depressive episode | 179 (95.7) | |
| Bipolar 2 major depressive episode | 8 (4.3) | |
| Past major depressive episode | 156 (83.4) | |
| Current melancholia | 105 (56.1) | |
| Current psychotic symptoms (delusions and/or hallucinations) | 49 (26.2) | |
| With dysthymia (“double depression”) | 17 (9.1) | |
| Any other comorbid anxiety, substance use or eating disorder | 151 (80.3) | |
| Substance use disorder (alcohol and/or drug abuse or dependence) | 32 (17.1) | |
| Eating disorder (anorexia nervosa, bulimia nervosa, binge eating disorder) | 22 (11.8) | |
| Anxiety disorder: | 146 (78.1) | |
| Panic disorder or agoraphobia | 86 (46.2) | |
| Generalised anxiety disorder | 85 (45.7) | |
| Simple phobia | 48 (25.8) | |
| Social phobia | 44 (23.7) | |
| Obsessive compulsive disorder | 37 (19.9) | |
| Post-traumatic stress disorder | 30 (16.1) | |
| Somatoform disorder (hypochondriasis or another somatoform disorder) | 31 (16.6) | |
| Current active physical illness: | 120 (64.2) | |
| One current active physical illness | 77 (41.2) | |
| Two or more active physical illnesses | 25 (13.4) | |
| Current rheumatological or orthopaedic problem | 43 (23.4) | |
| Current cardiovascular disorder (including diabetes mellitus) | 33 (17.1) | |
| Current respiratory disorder | 26 (13.5) | |
| Current neurological disorder | 18 (9.4) | In summary, as assessed using the above battery of psychometric measures, the cohort met diagnostic criteria for moderate-severe depression with a high degree of psychiatric comorbidity 151 (80.3%), the most common of which was anxiety disorders, 146 (78.1%). In addition, the cohort reported a high level of comorbid physical illness 120 (64.2%). Taking into consideration the severity and duration of the primary diagnosis of depression (with a mean number of years since first being diagnosed with depression of 16.7 years, with 81% of participants reporting depressive symptomatology for a period of greater than the 12 months prior to baseline data collection) alongside co-morbid psychiatric and physical illness, this group represent a cohort of participants experiencing both acute and chronic ill-health over a sustained time period. |
Healthy Controls
The measures tested in this PhD thesis were also administered to a group of healthy controls matched against the demographic data of the study cohort shown in table 6. The purpose of the inclusion of a healthy control group was to establish whether the measures tested in this PhD study measure the constructs they purport to measure (shame, self-criticism and selfcompassion) in the target population i.e. people experiencing persistent, treatment resistant depression and that these constructs are not present in the non-depressed general population. Therefore, the HDRS-17 and BDI-I were administered to assess level of depression in the healthy control group, followed by the administration of the OAS, FSCSR and SCS to test how each measure performed among a group of healthy controls compared to the study cohort. A decision was taken not to administer all three depression measures used in the study. This was informed by two principles. Firstly, given this was a non-depressed sample then it was felt two measures of depression were sufficient to establish the nondepressed status of the healthy control group. Secondly from both an ethical and data quality perspective it is important to maintain a balance between not over burdening participants with excessive workload and collecting high quality data that holds theoretical integrity. This sample was recruited by the author of this PhD thesis and the definition of healthy control and the process of recruitment are described in chapter 3 of this thesis.
In total 40 potential participants made contact, of which 33 met the inclusion criteria for healthy controls. This final group of 33 participants were 51.5% of female with a mean age of 48.7 years. The scores on the HDRS-17 and BDI-I for the healthy control group each confirmed absence of depressive symptomatology both current and past. The mean for these measures for healthy controls compared to the study cohort can be seen in table 9 below.
TABLE 9: MEAN SCORES (SD) ON HDRS-17 AND BDI-I FOR HEALTHY CONTROL GROUP VERSUS STUDY COHORT
| Measure | Mean (SD) SC |
Mean (SD) HC |
Diff (mean SC |
– mean HC) | 95% CI | P value |
| HRSD |
22.60 (5.19) |
1.18 (1.82) |
21.47 | 20.43–22.39 | P<0.001 | |
| BDI | 35.75 (8.87) |
1.90 (2.24) |
33.84 | 32.32–35.35 | P<0.001 | |
| OAS |
43.68 (16.00) |
9.24 (6.93) |
34.44 | 30.91–37.96 | P<0.001 | |
| FSCSR | 46.50 (9.59) | 33.57 (4.69) | 12.92 | 10.77–15.08 | P<0.001 | |
| SCS |
50.40 (13.70) |
75.79 (8.54) | — 25.38 | -28.98 — -21.78 | P<0.001 | SC = Study Cohort HC = Healthy Controls |
As indicated by the results in table 9 the healthy control sample were deemed non-depressed as measured on the HDRS-17 (mean score SC = 22.60 (SD- 5.19); HC = 1.18 (SD 1.82)) and BDII (mean score SC = 35.75 (SD 8.87); HC = 1.90 (SD 2.24), with confidence intervals between
20.43–22.39 (HRSD-17) and 32.32–35.35 (BDI-I) and a statistically significant p value of
P<0.001. With regard to the three measures tested in this study the OAS mean score for the study cohort 43.68 (SD 16.00) and the healthy controls was 9.24 (SD 6.93), with confidence intervals between 30.91–37.96 and a statistically significant p value of P<0.001. On the FSCSR the mean score for the study cohort 46.50 (SD 9.59) and healthy controls was 33.57 (SD 4.69), with 95% confidence intervals of 10.77–15.08 and a statistically significant p value of P<0.001. On the SCS the mean score for and the study cohort 50.40 (SD 13.70) and the healthy controls was 75.40 (SD 8.54) with negative confidence intervals of -28.98 — -21.78 and a statistically significant p vale of P<0.001.
Descriptive Statistics for Other as Shamer Scale (OAS) baseline
The OAS is comprised of 3 Factors:
-
Inferior (items: 1,2,3,5,6,7,8)
-
Emptiness (items 15,16,17,18)
-
Mistakes (items 3,9,10, 11,12,13,14)
In the second publication which details the development of the OAS (Allan, Gilbert and Goss, 1994) the authors note the following:
‘Item 10 failed to load above the criterion on any factor….. The item “People see me as striving for perfection but being unable to reach my own standards” (item 10) performed well with respect to the overall scale coefficient and was retained in calculating the total
OAS score. However, this item is not included in the subfactor scores as it did not load above
the cut off on any factor’.
(Allan, Gilbert and Goss, 1994 p. 715)
When the OAS as devised item 10 (‘People see me as striving for perfection but being unable to reach my own standards’) was in the mistakes sub-scale. Given how item 10 performed when the scale was devised (see Allan, Gilbert and Goss, 1994 p. 715), in the data analysis of this PhD thesis item 10 was excluded from the mistakes sub-scale analysis. However, it was included in the CFA to assess how it performed. This latter decision was based on the fact the study sample comprises a clinical cohort (as opposed to the student cohort in the Goss, Gilbert and Allan (1994) sample) and therefore in terms of completeness it was valid to assess item 10 as part of CFA.
TABLE 10: SUMMARY STATISTICS FOR OAS AT BASELINE
| cases | |||||||
| Valid | Missing | Total | |||||
| N | Percent | N | Percent | N | Percent | ||
| Inferior baseline | 148 | 93.7% | 10 | 6.3% | 158 | 100.0% | |
| Emptiness baseline | 148 | 93.7% | 10 | 6.3% | 158 | 100.0% | |
| Mistakes baseline | 148 | 93.7% | 10 | 6.3% | 158 | 100.0% | |
| The summary statistics for the OAS at baseline can be seen in Table 10. As reported in chapter 3 of this thesis, one study site failed to administer the OAS. This reduced the sample from the original 187 to 158. A further 10 participants then either failed or refused to complete the OAS. The issue of failure/refusal to complete questionnaires is addressed more fully in the discussion chapter of this thesis. As a result, the sample size (N=148) for this measure is smaller than that reported below for the FSCSR and SCS. |
TABLE 11: DISTRIBUTION FOR EACH SUB-SCALE OF OAS AT BASELINE
| OAS | Mean | Median | Minimum | Maximum | Std.Dev. | |
|
Inferior BASELINE |
18.64 | 20.00 | 0.00 | 28.00 | 7.00 | |
| Emptiness BASELINE | 8.87 | 9.00 | 0.00 | 16.00 | 4.15 | |
| Mistakes BASELINE | 13.99 | 14.00 | 0.00 | 24.00 | 5.98 | Table 11 shows the mean, median, maximum and minimum and standard deviation for each of the sub-scales of the OAS at baseline. For each sub-scale the scores cluster widely around the mean with the inferior sub-scale showing the largest standard deviation and emptiness the lowest standard deviation of the three sub-scales. |
The histogram for the inferior sub-scale demonstrated a moderate negative skew (see appendix XIX for the histogram of inferior sub-scale at baseline), indicating a preponderance of high scores on this sub-scale and a negative kurtosis (platykurtic). Fifty per cent of the scores on the inferior sub-scale fall between 13 and 24 with no outliers (see appendix XIX for the boxplot of inferior sub-scale at baseline).
The emptiness sub-scale shows a multimodal distribution (see histogram for emptiness subscale at baseline in appendix XX) with an excess of kurtosis. Fifty per cent of the scores falling between 6 and 12, with no outliers (see box plot for the emptiness sub-scale at baseline in appendix XX).
The mistakes sub-scale (see the histogram for the mistakes sub-scale at baseline in appendix XXI) shows a less marked negative skew and a negative kurtosis (platykurtic) distribution. Fifty per cent of the scores falling between 10 and 18 with no outliers (see the box plot for mistakes sub-scale at baseline in appendix XXI).
Reliability for Other as Shamer Scale (OAS) baseline
TABLE 12: CRONBACH’S ALPHA SCORES AT BASELINE FOR OAS SCALE
| Sub-scale | Cronbach’s Alpha | Number of items | |
| Inferior | 0.93 | 7 | |
| Emptiness | 0.82 | 4 | |
| Mistakes | 0.90 | 6 | |
| All items | 0.95 | 18 | Table 12 shows a Cronbach Alpha scores at baseline for the scale as a whole and each subscale. The scores rendered are indicative of a high degree of internal consistency both for the OAS as a scale and each of its individual sub-scales (Bland and Altman 1997). |
Tables 13 and 14 below show the item statistics (mean and standard deviation) and item to item correlations for the inferior sub-scale of the OAS at baseline. In summary the mean item score for this sub-scale is 2.65 with a range from 2.32–3.19 and variance of 0.09
TABLE 13: ITEM STATISTICS FOR SUB-SCALE INFERIOR AT BASELINE
| Inferior | mean | Standard deviation | N |
| OAS 1 | 2.92 | 1.07 | 145 |
| OAS 2 | 2.71 | 1.21 | 145 |
| OAS 4 | 3.19 | 1.03 | 145 |
| OAS 5 | 2.46 | 1.20 | 145 |
| OAS 6 | 2.32 | 1.29 | 145 |
| OAS 7 | 2.49 | 1.26 | 145 |
| OAS 8 | 2.48 | 1.21 | 145 |
In this analysis n = 145 as three participants did not endorse all the items in the scale.
TABLE 14: ITEM STATISTICS FOR SUB-SCALE INFERIOR AT BASELINE
| Inferior | OAS 1 | OAS 2 | OAS 4 | OAS 5 | OAS 6 | OAS 7 | OAS 8 | |
| OAS 1 | 1.00 | 0.81 | 0.56 | 0.70 | 0.67 | 0.65 | 0.60 | |
| OAS 2 | 0.81 | 1.00 | 0.55 | 0.73 | 0.71 | 0.64 | 0.71 | |
| OAS 4 | 0.56 | 0.55 | 1.00 | 0.54 | 0.54 | 0.57 | 0.57 | |
| OAS 5 | 0.70 | 0.73 | 0.54 | 1.00 | 0.76 | 0.67 | 0.69 | |
| OAS 6 | 0.67 | 0.71 | 0.54 | 0.76 | 1.00 | 0.68 | 0.77 | |
| OAS 7 | 0.65 | 0.64 | 0.57 | 0.67 | 0.68 | 1.00 | 0.74 | |
| OAS 8 | 0.60 | 0.71 | 0.57 | 0.69 | 0.77 | 0.74 | 1.00 | In the Inferior sub-scale of the OAS at baseline, all item to item correlations were above 0.3 which indicates an acceptable level of association of each item to the construct Inferior. Item 4, (‘I feel insecure about others opinions of me’) demonstrated the weakest association. Items 2 (‘I think that other people look down on me’) and item 6 (‘others see me as small and insignificant’) demonstrated the strongest association. |
Tables 15 and 16 below show the item statistics (mean and standard deviation) and item to item correlations for the emptiness sub-scale of the OAS at baseline. In summary the mean item score for this sub-scale was 2.22 with a range from 2.16–2.34 and variance of 0.2
TABLE 15: ITEM STATISTICS FOR SUB-SCALE EMPTINESS AT BASELINE
| Emptiness | Mean | Standard Deviation | Number of respondents | % |
Total sample size |
|
| OAS 15 | 2.34 | 1.27 | 144 | 90.6 | 158 | |
| OAS 16 | 2.16 | 1.27 | 144 | 90.6 | 158 | |
| OAS 17 | 2.24 | 1.24 | 144 | 90.6 | 158 | |
| OAS 18 | 2.16 | 1.26 | 144 | 90.6 | 158 | In this analysis n = 144 as four participants did not endorse all the items in the scale. |
TABLE 16: ITEM TO ITEM CORRELATION FOR SUB-SCALE EMPTINESS AT BASELINE
| Emptiness | OAS 15 | OAS 16 | OAS 17 | OAS 18 | |
| OAS 15 | 1.00 | 0.48 | 0.48 | 0.36 | |
| OAS 16 | 0.48 | 1.00 | 0.73 | 0.54 | |
| OAS 17 | 0.48 | 0.73 | 1.00 | 0.64 | |
| OAS 18 | 0.36 | 0.54 | 0.64 | 1.00 | In the emptiness sub-scale of the OAS, item 18 (‘others see me as fragile’) did not score above 0.3 indicating a weaker association to the construct emptiness than the other items in this sub-scale. Item 17 (‘others think there is something missing in me’) showed the strongest association. |
Tables 17 and 18 below show the item statistics (mean and standard deviation) and item to item correlations for the mistakes sub-scale of the OAS at baseline. In summary the mean item score for this sub-scale was 2.31 with a range from 1.97–3.09 and variance of 1.12
TABLE 17: ITEM STATISTICS FOR SUB-SCALE MISTAKES AT BASELINE
| Mistakes | Mean | Standard Deviation | Number of respondents | % | Total sample |
size |
| OAS 3 | 2.08 | 1.18 | 146 | 90.6 | 158 | |
| OAS 9 | 2.30 | 1.20 | 146 | 90.6 | 158 | |
| OAS 11 | 3.09 | 0.97 | 146 | 90.6 | 158 | |
| OAS 12 | 2.17 | 1.15 | 146 | 90.6 | 158 | |
| OAS 13 | 1.97 | 1.31 | 146 | 90.6 | 158 | |
| OAS 14 | 2.35 | 1.24 | 146 | 90.6 | 158 | In this analysis n = 146 as two participants did not endorse all the items in the scale. |
TABLE 18: ITEM TO ITEM CORRELATION FOR SUB-SCALE MISTAKES AT BASELINE
| Mistakes | OAS 3 | OAS 9 | OAS 11 | OAS 12 | OAS 13 | OAS 14 |
| OAS 3 | 1.00 | 0.57 | 0.44 | 0.68 | 0.68 | 0.58 |
| OAS 9 | 0.57 | 1.00 | 0.61 | 0.61 | 0.61 | 0.62 |
| OAS 11 | 0.44 | 0.61 | 1.00 | 0.48 | 0.49 | 0.62 |
| OAS 12 | 0.68 | 0.61 | 0.48 | 1.00 | 0.81 | 0.69 |
| OAS 13 | 0.68 | 0.61 | 0.49 | 0.81 | 1.00 | 0.79 |
| OAS 14 | 0.54 | 0.64 | 0.63 | 0.66 | 0.73 | 1.00 |
In the mistakes sub-scale of the OAS all item correlations were above 0.3 which indicated an acceptable level of association between all the items to the construct mistakes. Item 11, (‘I think others are able to see my defects’) showed the weakest association, with items 12 (‘others are critical or punishing when I make a mistake’) and item 13 (‘people distance themselves from me when I make a mistake’) showing the strongest association.
Split-Half Reliability for OAS at baseline
Tables 19 and 20 below shows the split half reliability of the OAS at baseline which demonstrated good internal consistency for the OAS.
TABLE 19: SUMMARY ITEM MEANS STATISTICS FOR OAS AT BASELINE
| Mean | minimum | maximum | range | Maximum/ | |
| minimum | |||||
| Item means | Part 1 | 2.55 |
2.30
2.42 | 2.09
1.99
1.99 | 3.18
3.07
3.18 | 1.09
1.08
1.19 | 1.52
1.54
1.59 |
| Part 2 |
| Both parts |
| Variance | N of items | ||
| Item means | Part 1 | 0.11 | 9a |
| Part 2 | 0.09 | 9b | |
| Both parts | 0.11 | 18 | The items are OAS 1, OAS 2, OAS 3, OAS 4, OAS, 5, OAS 6, OAS, 7, OAS, 8 OAS 9 |
The items are OAS 10, OAS 11, OAS 12, OAS 13, OAS, 14, OAS 15, OAS, 16, OAS, 17 OAS 18 TABLE 20: SPLIT HALF RELIABILITY SCALE STATISTICS FOR OAS AT BASELINE
| Mean | Variance | Std. Deviation | N of Items | |
| Part 1 |
Part
2
Both
Parts | 22.96 | 78.46 | 8.85 | 9a |
| 20.72 | 63.65 | 7.97 | 9b | |
| 43.68 | 259.45 | 16.10 | 18 | a. The items are OAS 1, OAS 2, OAS 3, OAS 4, OAS 5, OAS 6, OAS 7, OAS, 8, OAS 9 |
b. The items are OAS 10, OAS 11, OAS, 12, OAS, 13, OAS 14, OAS, 15, OAS 16, OAS 17, OAS 18
Test-retest reliability for OAS at baseline and 6 months
Table 21 shows the test-retest reliability for the OAS using Pearson Product Moment R correlation (Dancy, Reidy and Rowe 2012) comparing baseline with 6 months. The rationale for the time points for conducting test-retest reliability is given in chapter 3 of this thesis. At baseline the OAS was administered to 150 participants (N) and to 97 participants at 6 months.
This is because the 6-month data collection point was collected by posting questionnaires to participants rather than the face to face interview that took place a baseline. This resulted in a 35.3% (53 participants) reduction in sample size.
The Pearson correlation is the test-retest reliability coefficient and the sig. (2 tailed) is the P value which indicates the statistical significance of the coefficient. Test retest reliability for the inferior (0.62 P < 0.01) mistakes (0.64 P< 0.01) factors is moderate but significant at the 0.01 level (2 tailed). The emptiness factor (0.48 P< 0.01) demonstrates a weaker level of testretest reliability but still at a significant level. The correlations are significant at a 0.01 level (2 tailed).
TABLE 21: TEST-RETEST RELIABILITY FOR OAS AT BASELINE AND 6 MONTHS
**. Correlation is significant at the 0.01 level (2-tailed).
| Inferior baseline | Emptiness baseline | Mistakes baseline | Inferior |
6months | Emptiness
6months | Mistakes
6months |
| Inferior baseline | Pearson r |
Sig. (2 tailed)
N
| 1 |
149 | 0.67**
0.01
149 | 0.82**
0.01
149 | 0.62**
0.01
92 | 0.45**
0.01
92 | 0.51**
0.01
92 |
| Emptiness baseline | Pearson |
Correlation
Sig. (2 tailed)
N
| 0.67** |
0.01
149 | 1
149 | 0.56**
0.01
149 | 0.38**
0.01
91 | 0.48**
0.01
91 | 0.33*
0.01
91 |
| Mistakes baseline | Pearson |
Correlation
Sig. (2 tailed)
N
| 0.82** |
0.01
149 | 0.56**
0.01
149 | 1
0.01
149 | 0.62**
0.01
91 | 0.43**
0.01
91 | 0.64
0.01
91
| Inferior |
6 months | Pearson
Correlation
Sig. (2 tailed)
N
| 0.62** |
0.01
92 | 0.38**
0.01
91 | 0.62**
0.01
91 | 1
97 | 0.67**
0.01
97 | 0.82**
0.01
97 |
| Emptiness 6 months | Pearson |
Correlation
Sig. (2 tailed)
N
| 0.45** |
0.01
92 | 0.48**
0.01
91 | 0.43**
0.01
97 | 0.67**
0.01
97 | 1
97 | 0.65**
0.01
97 |
| Inferior |
6 months | Pearson
Correlation
Sig. (2 tailed)
N
| 0.51** |
0.01
92 | 0.33**
0.01
91 | 0.64**
0.01
91 | 0.82**
0.01
97 | 0.65**
0.01
97 | 1
97 |
Confirmatory Factor Analysis (CFA)
CFA was conducted to test the factor structure of the OAS using Mplus version, 7.4 (Muthén and Muthén, (1998–2012)), in its default setting for ordered items using Weighted Least Square Mean Variance adjusted (WLSMV) estimator on the baseline data collated from the
OAS, FSCSR and SCS. Missing values were automatically accounted for using the full information maximum likelihood approach built into Mplus. The continuous latent variables and indicators tested in this PhD thesis are illustrated in table 22 (see appendix XII for the complete OAS scale).
TABLE 22: THE CONTINUOUS LATENT VARIABLES AND INDICATORS TESTED FOR OAS, FSCSR AND SCS
| Measure | Continuous latent variables |
(factors) | Number of indicators per factor identified by item number on measure |
| Other as Shamer Scale (OAS) | Inferior |
Empty
Mistakes | 7 (1 2 4 5 6 7 8)
4 (15 16 17 18)
6 (3 9 10 11 12 13 14) |
| Forms of Self-Criticism and |
Self-reassurance Scale (FCSRS) | Inadequate
Hate
Reassured | 9 (1 2 4 6 7 14 17 18 20)
5 (9 10 12 15 21)
8 (3 5 8 11 13 16 19 21) |
| Self-Compassion Scale (SCS) | Kindness |
Judgement
Common Humanity
Isolation
Mindfulness
Overidentification | 5 (5 12 19 23 26)
5 (1 8 11 16 21)
4 (3 7 10 15)
4 (4 13 18 25)
4(2 6 20 24)
4 (9 14 17 22) | The model fit indices for the OAS is shown in table 23 below: The estimation procedure used in this analysis is Weighted Least Squares Maximum Variance (WLSMV). As described by Li (2016) this procedure has been specifically designed for analysing categorical observed data and assumes a normal latent distribution underlying each observed categorical variable. TABLE 23: MODEL FIT INDICES FOR OAS
| Measure | 𝑥2 | CFI | TLI | RMSEA |
| OAS | 274.91 |
P 0.01 | 0.97 | 0.97 | 0.86 |
Confirmatory Factor Analysis for Other as Shamer Scale
Confirmatory Factor Analysis (CFA) was conducted to test the three-factor model of the 18 item Other as Shamer Scale (OAS) (N= 149 see above for description of sample). 42 cases were missing across all variables and these cases were not included in the analysis. The CFA path diagram for the OAS at baseline is shown in figure 6 below. The CFA was assessed for exact model fit using WMSLV and Chi-square and for approximate fit using CFI, TLI and RMSEA. In assessing model fit (see table 23) the Chi-square P value of P<0.01 indicates no exact model fit. The CFI (0.97) and TLI (0.97) values indicate an acceptable fit. The RMSEA (0.86) demonstrates a convergent fit with the data sample.
Overall, the CFA pathway diagram for the OAS (see figure 6 p 150) showed a strong positive association between inferior and mistakes (0.88) and emptiness and inferior (0.78). The correlation between emptiness and mistakes showed a weak positive association (0.67). The CFA for OAS using the original factor structure showed an RMSEA of 0.10 which is just above the cut-off point of 0.1. The model modification index suggested loading items 12 (‘others are critical or punishing of me when I make a mistake’) and 13 (‘people distance themselves from me when I make a mistake’) on to the inferior factor would significantly improve the model fit (Marsh, Morin, Parker and Kaur, (2014). Hence a new model with items 12 and 13 crossloaded on both the inferior and mistakes factor was re-run. The model fit indices for this are RMSEA (0.86), CFI (0.97), TLI (0.97), CHI2 274.91 (130) with P value (P< 0.001). Both item 12 and 13 have negative loading parameters.
Item 15 (‘others see me as fragile’) showed a weaker association (0.56) with the construct emptiness and correlated poorly with items 16, 17 and 18 which constitute the other items in the emptiness sub-scale. Item 10 (‘people see me striving for perfection’) in the mistakes subscale showed a weak association (0.46) with the construct mistakes and did not correlate with either the inferior or emptiness constructs.
FIGURE 6: CONFIRMATORY FACTOR ANALYSIS PATH DIAGRAM FOR THE OTHER AS SHAMER SCALE (OAS)
Descriptive Statistics for Forms of Self-Criticising Self -Reassuring Scale (FSCRS)
The FSCSR is comprised of 3 Factors:
-
Inadequate self (items 1,2,4,6,7,14,17,18,20)
-
Hated Self (items 9,10,12,15,22)
-
Reassured self (items 3,5,8,11,13)
TABLE 24: SUMMARY STATISTICS FOR FSCSR AT BASELINE
| Cases | ||||||||
| Valid | Missing | Total | ||||||
| N | Percent | N | Percent | N | Percent | |||
| Inadequate selfBASELINE | 177 | 93.8% | 10 | 6.3% | 187 | 100.0% | ||
| Hated selfBASELINE | 177 | 93.8% | 10 | 6.3% | 187 | 100.0% | ||
| Reassured selfBASELINE | 177 | 93.8% | 10 | 6.3% | 187 | 100.0% | In summarising Table 24 (n = 177) refers to the fact 10 participants either failed or refused to complete the FSCSR. The issue of failure/refusal to complete questionnaires is addressed more fully in the discussion chapter of this thesis. |
TABLE 25: DISTRIBUTION FOR EACH SUB-SCALE OF FSCSR AT BASELINE
| FSCSR | Mean | Median | Minimum | Maximum | Std.Dev. |
| Inadequate self-BASELINE | 7.02 | 6.00 | .00 | 24.00 | 6.38 |
|
Hated self BASELINE |
11.68 | 12.00 | .00 | 20.00 | 4.99 |
|
Reassured self BASELINE |
7.02 | 6.00 | .00 | 24.00 | 4.96 |
Table 25 shows the mean, median and standard deviation for each of the sub-scales of the FSCSR at baseline. For the sub-scale inadequate self, the scores cluster widely around the mean with a large standard deviation.
The histogram in appendix XXII showed a moderate negative skewed distribution and a negative kurtosis (leptokurtic distribution) The box plot for the sub-scale inadequate self in appendix XXII showed 50% of the scores fell between 23 and 34 with four outliers, clustered between scores of 6–10. For the sub-scale hated self the scores clustered widely around the mean with a large standard deviation. The distribution was multimodal (see the histogram for sub-scale hated self in appendix XXIII) with, in descending order, the most frequently endorsed score being ‘moderately like me’ followed by ‘a little bit like me’ and ‘extremely like me’. There was an excess of kurtosis, this is reflective of the range of responses to items in this sub-scale. The box plot for the sub-scale hated self (see appendix XXIII) showed 50% of the scores fell between 7 and 16 with no outliers. For the sub-scale reassured self, the scores clustered widely around the mean with a large standard deviation. The histogram in appendix XXIV showed a moderately positive skew with low kurtosis. There was a greater frequency of scores clustered towards the ‘never and seldom like me’ endorsements on the scale. The box plot for the sub-scale reassured self (see appendix XXIV) showed 50% of the scores fall between 3–10 with four outliers scoring between 21–24.
Reliability of the FSCSR at baseline
TABLE 26: CRONBACH’S ALPHA FOR FSCSR AT BASELINE
| Sub-scale | Cronbach’s Alpha | Number of items |
| Inadequate Self | 0.83 | 9 |
| Hated Self | 0.75 | 5 |
| Reassured Self | 0.75 | 8 |
| All items | 0.71 | 22 |
Table 26: shows a Cronbach Alpha scores at baseline for the scale as a whole and each subscale. The scores rendered are indicative of an acceptable degree of internal consistency both for the FSCSR as a scale and each of its individual sub-scales (Bland and Altman, 1997).
Tables 27 and 28 below show the item statistics (mean and standard deviation) and item to item correlations for the sub-scale inadequate self of the FSCSR at baseline. In summary the mean item score for this sub-scale is 3.08 with a range from 2.42–3.50 and variance of 1.08
TABLE 27: ITEM STATISTICS FOR SUB-SCALE INADEQUATE SELF AT BASELINE
| Inadequate |
Self | Mean | Standard Deviation | Number of respondents | % | Total sample
size |
| FSCSR 1 | 3.50 | 0.76 | 177 | 92.2 | 187 |
| FSCSR 2 | 3.36 | 0.85 | 177 | 92.2 | 187 |
| FSCSR 4 | 2.42 | 1.21 | 177 | 92.2 | 187 |
| FSCSR 6 | 3.19 | 1.19 | 177 | 92.2 | 187 |
| FSCSR 7 | 2.91 | 1.16 | 177 | 92.2 | 187 |
| FSCSR 14 | 3.31 | 0.96 | 177 | 92.2 | 187 |
| FSCSR 17 | 3.15 | 1.14 | 177 | 92.2 | 187 |
| FSCSR 18 | 2.92 | 1.15 | 177 | 92.2 | 187 |
| FSCSR 20 | 3.03 | 1.18 | 177 | 92.2 | 187 |
TABLE 28: ITEM TO ITEM CORRELATION FOR SUB-SCALE INADEQUATE SELF AT BASELINE
| Inadequate |
self | FSCSR
1 | FSCSR
2 | FSCSR
4 | FSCSR
6 | FSCSR
7 | FSCSR 14 | FSCSR 17 | FSCSR 18 | FSCSR 20 |
| FSCSR 1 | 1.00 | 0.65 | 0.24 | 0.48 | 0.47 | 0.44 | 0.40 | 0.34 | 0.21 | |
| FSCSR 2 | 0.65 | 1.00 | 0.29 | 0.55 | 0.50 | 0.55 | 0.39 | 0.33 | 0.25 | |
| FSCSR 4 | 0.24 | 0.29 | 1.00 | 0.12 | 0.19 | 0.33 | 0.24 | 0.23 | 0.24 | |
| FSCSR 6 | 0.48 | 0.55 | 0.12 | 1.00 | 0.61 | 0.46 | 0.42 | 0.37 | 0.28 | |
| FSCSR 7 | 0.47 | 0.50 | 0.19 | 0.61 | 1.00 | 0.49 | 0.35 | 0.43 | 0.12 | |
| FSCSR 14 | 0.44 | 0.55 | 0.33 | 0.46 | 0.49 | 1.00 | 0.57 | 0.50 | 0.33 | |
| FSCSR 17 | 0.40 | 0.39 | 0.24 | 0.42 | 0.35 | 0.57 | 1.00 | 0.43 | 0.28 | |
| FSCSR 18 | 0.34 | 0.33 | 0.23 | 0.37 | 0.43 | 0.50 | 0.43 | 1.00 | 0.31 | |
| FSCSR 20 | 0.21 | 0.25 | 0.24 | 0.28 | 0.12 | 0.33 | 0.28 | 0.31 | 1.00 | In the sub-scale Inadequate Self correlations for item 4, (‘I find it hard to control my anger and frustration at myself’) and item 20 (‘There is part of me that wants to get rid of the parts I don’t like’) are below 0.3 which indicates there is a weaker association to the construct inadequate self. The strongest association is shown by item 1 (‘I am easily disappointed in myself’) and item 2 (‘There is part of me that puts me down’). |
Tables 29 and 30 below show the item statistics (mean and standard deviation) and item to item correlations for the Hated Self sub-scale of the FSCSR at baseline. In summary the mean item score for this sub-scale is 2.34 with a range from 1.77–3.00 and variance of 1.23.
TABLE 29: ITEM STATISTICS FOR SUB-SCALE HATED SELF AT BASELINE
| Hated self | Mean | Standard Deviation | Number of respondents | % | Total sample size |
| FSCSR 9 | 1.77 | 1.43 | 177 | 92.2 | 187 |
| FSCSR 10 | 2.47 | 1.43 | 177 | 92.2 | 187 |
| FSCSR 12 | 2.50 | 1.23 | 177 | 92.2 | 187 |
| FSCSR 15 | 2.00 | 1.51 | 177 | 92.2 | 187 |
| FSCSR 22 | 3.00 | 1.31 | 177 | 92.2 | 187 |
TABLE 30: ITEM TO ITEM CORRELATION FOR SUB-SCALE HATED SELF AT BASELINE
| Hated self | FSCSR 9 | FSCSR 10 | FSCSR 12 | FSCSR 15 | FSCSR 22 |
| FSCSR 9 | 1.00 | 0.45 | 0.42 | 0.33 | 0.25 |
| FSCSR 10 | 0.45 | 1.00 | 0.45 | 0.42 | 0.51 |
| FSCSR 12 | 0.42 | 0.45 | 1.00 | 0.36 | 0.31 |
| FSCSR 15 | 0.33 | 0.42 | 0.36 | 1.00 | 0.32 |
| FSCSR 22 | 0.25 | 0.51 | 0.31 | 0.32 | 1.00 |
In the sub-scale hated self of the FSCSR correlations for item 15 (‘I call myself names’) and item 22 (‘I don’t like being me’) are below 0.3 indicating a weak association with the construct hated self. The strongest association is shown between item 10 (‘I have a sense of disgust with myself’) and item 12 (‘I stop caring about myself’).
Tables 31 and 32 below show the item statistics (mean and standard deviation) and item to item correlations for the sub-scale reassured self of the FSCSR at baseline. In summary the mean item score for this sub-scale is 0.87 with a range from 1.86–0.56 and variance of 1.30
TABLE 31: ITEM STATISTICS FOR SUB-SCALE REASSURED SELF AT BASELINE
| Reassured self | Mean | Standard Deviation | Number of respondents | % | Total sample |
size |
| FSCSR_3 | 1.22 | 1.29 | 174 | 92.2 | 187 |
| FSCSR_5 | 0.56 | 0.98 | 174 | 92.2 | 187 |
| FSCSR_8 | 0.78 | 1.01 | 174 | 92.2 | 187 |
| FSCSR_11 | 0.89 | 0.92 | 174 | 92.2 | 187 |
| FSCSR_13 | 0.58 | 0.91 | 174 | 92.2 | 187 |
| FSCSR_16 | 0.50 | 0.83 | 174 | 92.2 | 187 |
| FSCSR_19 | 1.86 | 1.21 | 174 | 92.2 | 187 |
| FSCSR_21 | 0.62 | 0.90 | 174 | 92.2 | 187 |
TABLE 32: ITEM TO ITEM CORRELATIONS FOR SUB-SCALE REASSURED SELF AT BASELINE
| Reassured Self | FSCSR |
3 | FSCSR
5 | FSCSR
8 | FSCSR 11 | FSCSR 13 | FSCSR 16 | FSCSR 19 | FSCSR 21 |
| FSCSR 3 | 1.00 | 0.26 | 0.23 | 0.27 | 0.34 | 0.19 | 0.12 | 0.24 | |
| FSCSR 5 | 0.26 | 1.00 | 0.41 | 0.18 | 0.39 | 0.32 | 0.01 | 0.23 | |
| FSCSR 8 | 0.23 | 0.41 | 1.00 | 0.43 | 0.53 | 0.46 | 0.17 | 0.41 | |
| FSCSR 11 | 0.27 | 0.18 | 0.43 | 1.00 | 0.48 | 0.32 | 0.19 | 0.41 | |
| FSCSR 13 | 0.34 | 0.39 | 0.53 | 0.48 | 1.00 | 0.39 | 0.21 | 0.39 | |
| FSCSR 16 | 0.19 | 0.32 | 0.46 | 0.32 | 0.39 | 1.00 | 0.09 | 0.45 | |
| FSCSR 19 | 0.12 | 0.01 | 0.17 | 0.19 | 0.21 | 0.09 | 1.00 | 0.28 | |
| FSCSR 21 | 0.24 | 0.23 | 0.41 | 0.41 | 0.39 | 0.45 | 0.28 | 1.00 | In the sub-scale reassured self of the FSCSR item 19 (‘I am able to care and look after myself’) does not reach the acceptable cut off of 0.3 when compared with any other item in the subscale and does not appear to fit in this data sample. Item 3 (‘I am able to remind myself of positive things about myself’) only reaches a cut off 0.3 when compared with item 13 (‘I find it easy to like myself’). Item 5 (‘I find it easy to forgive myself’) also score below 0.3 when correlated with items 3 (‘I am able to remind myself of positive things about myself’), 11 (‘I can still feel loveable and acceptable’) and 21 (‘I encourage myself for the future’) indicating there is a weaker association to the construct reassured self. Item 8, (‘I still like being me’) shows the strongest association to this construct. |
Split half reliability for the FSCSR at baseline
TABLE 33: SUMMARY ITEM MEANS STATISTICS FOR FSCSR AT BASELINE
| Mean |
| Minimum | Maximum | Range | Maximum/minimum | |||
| Item Means | Part 1 | 2.11 | 0.56 | 3.50 | 2.94 | 6.18 |
| Part 2 | 2.15 | 0.49 | 3.35 | 2.85 | 6.74 | |
| Both | 2.13 | 0.49 | 3.50 | 3.01 | 7.05 |
| Variance | N of items | ||
| Item means | Part 1 | 1.22 | 11a |
| Part 2 | 1.24 | 11b | |
| Both parts | 1.17 | 22 |
a. The items are: FSCSR 1, FSCSR 2, FSCSR 3, FSCSR4, FSCSR 5, FSCSR 6, FSCSR 7, FSCSR 8,
FSCSR, 9, FSCSR 10, FSCSR 11
b. The items are: FSCSR 12, FSCSR 13, FSCSR 14, FSCSR 15, FSCSR 16, FSCSR 17, FSCSR 18, FSCSR 19, FSCSR, 20, FSCSR 21, FSCSR 22
Table 34 below, shows the split half reliability of the FSCSR at baseline which demonstrated good internal consistency for the FSCSR.
TABLE 34: SPLIT HALF RELIABILITY SCALE STATISTICS FOR FSCSR AT BASELINE
| Mean | Variance | Std. |
deviation | N of items |
| Part 1 | 23.24 | 27.50 | 5.24 | 11a | |
| Part 2 | 23.68 | 27.31 | 5.22 | 11b | |
| Both parts | 46.93 | 89.16 | 9.44 | 22 | a. The items are: FSCSR 1, FSCSR 2, FSCSR 3, FSCSR4, FSCSR 5, FSCSR 6, FSCSR 7, FSCSR 8, |
FSCSR, 9, FSCSR 10, FSCSR 11
b. The items are: FSCSR 12, FSCSR 13, FSCSR 14, FSCSR 15, FSCSR 16, FSCSR 17, FSCSR 18, FSCSR 19, FSCSR, 20, FSCSR 21, FSCSR 22
Test-retest reliability for FSCSR at baseline and 6 months
Table 35 shows the test-retest reliability for the FSCSR using Pearson Product Moment R correlation (Dancy, Reidy and Rowe 2012) comparing baseline with 6 months. The rationale for the time points for conducting test-retest reliability is given in chapter 3 of this thesis. At baseline the FSCSR was administered to 177 participants and to 124 participants at 6 months. This is because the 6-month data collection point was collected by posting questionnaires to participants rather than the face to face interview that took place a baseline. This resulted in a 31.1% (56 participants) reduction in sample size. The Pearson correlation is the test-retest reliability coefficient and the sig. (2 tailed) is the P -value which indicates the statistical significance of the coefficient. For the FSCSR each factor shows a moderate but significant level of test retest reliability as follows: hated self (0.712 P<0.001). Inadequate self (0.527 P<0.001 and reassured self (0.457 P<0.001) at the 0.01 level (2 tailed).
TABLE 35: TEST -RETEST RELIABILITY FOR FSCSR BETWEEN BASELINE AND 6 MONTHS
**Correlation is significant the <0.01 level (2-tailed)
| Inadequat e self |
Baseline | Hated self
baselin e | Reassure d self
Baseline | Inadequat e self
6 months | Hated self
6
month
s | Reassure d self
6 months |
| Inadequat e self |
Baseline | Pearson
Correlatio n
Sig. (2 tailed)
N
| 1 |
177 | 0.69**
<0.01
177 | -0.35**
<0.01
177 | 0.52**
<0.01
122 | 0.43**
<0.01
122 | -0.341**
<0.01
122 | |
Hated self baseline | Pearson
Correlatio n
Sig. (2 tailed)
N
| 0.69** |
<0.01
177 | 1
<0.01
177 | -0.38**
<0.01
177 | 0.47**
<0.01
122 | 0.71**
<0.01
122 | -0.44
<0.01
122 |
Reassured
self baseline | Pearson
Correlatio n
Sig. (2 tailed)
N
| -0.35** |
0.00
177 | -.387**
0.00
177 | 1
0.00
177 | -0.25**
0.00
122 | -0.25**
0.00
122 | 0.45**
0.00
122 | |
Inadequat e
self
6 months | Pearson
Correlatio n
Sig. (2 tailed)
N
| 0.52** |
0.00
122 | 0.47**
0.00
122 | -0.25**
0.00
122 | 1
0.00
124 | 0.71**
0.00
124 | -0.59**
0.00
124 |
| Hated self |
6months | Pearson
Correlation
Sig. (2 tailed)
N
| 0.43** |
0.00
122 | 0.712**
0.00
122 | -0.25**
0.00
122 | 0.71**
0.00
122 | 1
124 | -0.65**
0.00
124 | |
Reassured
self
6 months | Pearson
Correlation
Sig. (2 tailed)
N
| -0.34** |
0.00
122 | -0.44**
0.00
122 | 0.45**
0.00
122 | -0.59
0.00
122 | -0.65**
0.00
124 | 1
124 |
Confirmatory Factor Analysis for the Forms of Self-Criticism and self-Reassurance Scale (FSCSR)
Confirmatory Factor Analysis was conducted to test the three-factor model of the 22 item Forms of Self-Criticism and Self-Reassurance Scale (N= 177, see above for description of sample). 12 cases were missing across all variables and these cases were not included in the analysis. The CFA path diagram for the FSCSR is shown in figure 7 below. The CFA was assessed for exact model fit using WMSLV and Chi-square and for approximate fit using CFI, TLI and RMSEA. In assessing model fit (see table 36) the Chi-square p value of P<0.01 indicates no exact model fit. The CFI (0.94) TLI (0.94) values indicate acceptable level of approximate model fit. The RMSEA (0.06) is indicative of a convergent fit.
TABLE 36: MODEL FIT INDICES FOR FSCSR
| Measure | 𝑥2 | CFI | TLI | RMSEA |
| FSCSR | 3507.97 |
P 0.01 | 0.94 | 0.94 | 0.06 | Overall the CFA pathway diagram for the FSCSR showed a strong positive correlation (0.86) between the factor’s inadequate self and hated self and a moderate negative correlation (0.66) between the factors hated self and reassured self and factors reassured self and inadequate self (-0.53).
FIGURE 7: CONFIRMATORY FACTOR ANALYSIS PATH DIAGRAM FOR THE FORMS OF SELF-CRITICISING AND SELFREASSURING SCALE (FSCSR)
Descriptive Statistics for Self-Compassion Scale (SCS) baseline
The SCS is compiled of six sub-scales as follows:
Self-kindness (items 5, 12, 19, 23, 26) versus Self-judgement (items 1, 8, 11, 16, 21)
Common humanity (items 3, 7, 10, 15) versus Isolation (items 4, 13, 18, 25)
Mindfulness (items 9, 14, 17, 22) versus Over-identification (items 2, 6, 20, 24)
TABLE 37: SUMMARY STATISTICS FOR SELF-COMPASSION SCALE (SCS) AT BASELINE
| Cases | |||||||
| Valid | Missing | Total | |||||
| N | Percent | N | Percent | N | Percent | ||
| Self-Kindness | 179 | 93.2% | 8 | 6.8% | 187 | 100.0% | |
| Self-judgement | 179 | 93.2% | 8 | 6.8% | 187 | 100.0% | |
| Common Humanity | 179 | 93.2% | 8 | 6.8% | 187 | 100.0% | |
| isolation | 179 | 93.2% | 8 | 6.8% | 187 | 100.0% | |
| Mindfulness | 179 | 93.2% | 8 | 6.8% | 187 | 100.0% | |
| Over identification | 179 | 93.2% | 8 | 6.8% | 187 | 100.0% | In summarising Table 37 n = 179 refers to the fact 8 participants either failed or refused to complete the SCS. The issue of failure/refusal to complete questionnaires is addressed more fully in the discussion chapter of this thesis. |
TABLE 38: DISTRIBUTION FOR EACH SUB-SCALE OF SCS AT BASELINE
| SCS | Mean | Median | Minimum | Maximum | Std.Dev. | |
| Self-kindness | 8.37 | 8.00 | 5.00 | 19.00 | 3.309 | |
| Self-judgement | 9.85 | 10.00 | 5.00 | 21.25 | 3.484 | |
| Common Humanity | 8.17 | 8.00 | 4.00 | 20.00 | 3.406 | |
| Isolation | 7.53 | 7.00 | 4.00 | 17.33 | 2.916 | |
| Mindfulness | 8.69 | 8.00 | 4.00 | 19.00 | 3.38 | |
| Over identification | 7.79 | 7.00 | 4.00 | 16.00 | 3.002 | Table 38 shows the mean, median and standard deviation for each of the sub-scales of the SCS at baseline. For the sub-scale self-kindness at baseline, scores clustered widely around the mean with a large standard deviation. There was a marked positive skew (see histogram for sub-scale self-kindness in appendix XXV) with positive kurtosis. The histogram reveals some bars which are absent which indicates that for some items there were no frequencies. |
Fifty per cent of the scores fell between 2–10 with four outliers at 18 and 19 (see box plot for sub-scale self-kindness in appendix XXV).
For the sub-scale self-judgement, scores cluster widely around the mean with a large standard deviation. There is a positively skewed multimodal distribution (see histogram for sub-scale self-judgement in appendix XXVI) with an excess of kurtosis. The histogram revealed some bars were absent which indicates there are no frequencies for some items. The items on the negative subscales are reversed scored therefore this distribution would be expected in a cohort of participants diagnosed with persistent, treatment resistant depression. Fifty per cent of the scores fall between 7 and 12 with two outliers at scores of 20 and 22 (see the boxplot for sub-scale selfjudgement in appendix XXVI).
For the sub-scale common humanity scores clustered widely around the mean with a large standard deviation. There was a positive skew with a multimodal distribution (see histogram for sub-scale common humanity in appendix XXVII) and an excess of kurtosis. The histogram revealed some bars were absent which indicates there were no frequencies for these items. Fifty per cent of the scores fell between 5 and 10 with three outliers falling between scores of 18–20 (see box plot for sub-scale common humanity in appendix XXVII).
For the sub-scale isolation at baseline scores cluster widely around the mean with a large standard deviation. There is a marked positive skew with a bimodal distribution (see histogram for sub-scale isolation in appendix XXVIII). The histogram revealed some bars were absent which indicates there were no frequencies for these items. The items on the negative subscales are reversed scored therefore this distribution would be expected in a cohort of participants diagnosed with persistent, treatment resistant depression. Fifty per cent of the scores falling between 5 and 9 with two outliers falling at scores 16 and 17 (see box plot for sub-scale isolation in appendix XXVIII).
For the sub-scale mindfulness at baseline scores clustered widely around the mean with a large standard deviation. There was a positive skew with a multimodal distribution and an excess of kurtosis (see histogram for sub-scale mindfulness in appendix XXIX). The histogram revealed some bars were absent which indicates there were no frequencies for these items. Fifty per cent of the scores fell between 6 and 11 with one outlier at a score of 18 (see box plot for sub-scale mindfulness in appendix XXIX).
For the sub-scale over-identification at baseline scores cluster widely around the mean with a large standard deviation. There is a positive skew with a multimodal distribution (see histogram for sub-scale overidentification in appendix XXX) and an excess of kurtosis. The histogram reveals some bars are absent which indicates there are no frequencies for some items. The items on the negative sub-scales are reversed scored therefore this distribution would be expected in a cohort of participants diagnosed with persistent, treatment resistant depression. Fifty per cent of the scores falling between 5 and 8.5 with one outlier with a score of 22 (see box plot for subscale overidentification in appendix XXX).
Reliability of SCS at baseline
TABLE 39: CRONBACH’S ALPHA FOR SCS AT BASELINE
| Sub-scale | Cronbach’s Alpha | Number of items | |
| Self-kindness | 0.73 | 5 | |
| Self-judgement | 0.66 | 5 | |
| Common humanity | 0.72 | 4 | |
| Isolation | 0.60 | 4 | |
| Mindfulness | 0.76 | 4 | |
| Over identification | 0.64 | 4 | |
| All variables | 0.87 | 26 | Table 39 shows a Cronbach Alpha scores at baseline for the SCS scale as a whole and each sub-scale. The scores rendered for the whole scale and the self-kindness, common humanity and mindfulness are indicative of an acceptable degree of internal consistency. However, the self-judgment, isolation and over-identification sub-scales do not reach a satisfactory level of internal consistency (Bland and Altman 1997). |
Tables 40 and 41 below show the item statistics (mean and standard deviation) and item to item correlations for the sub-scale self-kindness at baseline. In summary the mean item score for this sub-scale is 1.67 with a range from 1.39–1.90 and variance of 0.51
TABLE 40: ITEM STATISTICS FOR SUB-SCALE SELF-KINDNESS AT BASELINE
| Self-kindness | Mean | Std. Deviation | N | |
| SCS 5 | 1.72 | 1.06 | 168 | |
| SCS 12 | 1.39 | 0.78 | 168 | |
| SCS 19 | 1.52 | 0.75 | 168 | |
| SCS 23 | 1.90 | 1.161 | 168 | |
| SCS 26 | 1.85 | 0.96 | 168 | In table 40 n = 168 is accounted for as follows: 8 participants did not complete the measure and a further 11 failed to complete at least one item. |
TABLE 41: ITEM TO ITEM CORRELATION FOR SUB-SCALE SELF-KINDNESS AT BASELINE
| Self-kindness | SCS 5 | SCS 12 | SCS 19 | SCS 23 | SCS 26 | |
| SCS 5 | 1.00 | 0.55 | 0.53 | 0.25 | 0.35 | |
| SCS 12 | 0.55 | 1.00 | 0.51 | 0.22 | 0.29 | |
| SCS 19 | 0.53 | 0.51 | 1.00 | 0.36 | 0.40 | |
| SCS 23 | 0.25 | 0.22 | 0.36 | 1.00 | 0.26 | |
| SCS 26 | 0.35 | 0.29 | 0.40 | 0.26 | 1.00 | In the sub-scale self-kindness correlations for item 23 (‘I’m tolerant of my own flaws and inadequacies’) score below 0.3 indicating there is a weaker association to the construct selfkindness. Item 19 (‘I’m kind to myself when experiencing suffering’) shows the strongest association to this construct. |
Tables 42 and 43 below show the item statistics (mean and standard deviation) and item to item correlations for the sub-scale self-judgement at baseline. In summary the mean item score for this sub-scale is 1.93 with a range from 1.70–2.35 and variance of 0.65.
TABLE 42: ITEM STATISTICS FOR SUB-SCALE SELF-JUDGMENT AT BASELINE
| Self-judgment | Mean | Std. Deviation | N |
| SCS 1 | 1.79 | 0.90 | 169 |
| SCS 8 | 1.84 | 1.09 | 169 |
| SCS 11 | 2.35 | 1.20 | 169 |
| SCS16 | 1.70 | 0.78 | 169 |
| SCS 21 | 1.97 | 0.98 | 169 |
In table 42 n= 169 as 10 participants did not complete the measure and a further 8 refused/failed to complete at least 1 item on this sub-scale.
TABLE 43: ITEM TO ITEM CORRELATIONS FOR SUB-SCALE SELF-JUDGEMENT AT BASELINE
| Self-judgement | SCS 1 | SCS 8 | SCS 11 | SCS 16 | SCS 21 |
| SCS 1 | 1.00 | 0.34 | 0.38 | 0.42 | 0.22 |
| SCS 8 | 0.34 | 1.00 | 0.22 | 0.38 | 0.27 |
| SCS 11 | 0.38 | 0.22 | 1.00 | 0.20 | 0.22 |
| SCS 16 | 0.42 | 0.38 | 0.20 | 1.00 | 0.23 |
| SCS 21 | 0.22 | 0.27 | 0.22 | 0.23 | 1.00 |
In the sub-scale self-judgement correlations for item 8 (‘when times are difficult I tend to be tough on myself’), item 11 (‘I’m intolerant and impatient towards those aspects of my personality I don’t like’), item 16 (‘When I see aspects of myself I don’t like I get down on myself’) and item 21 (‘I can be a bit cold-hearted towards myself when I’m experiencing suffering’) each score below 0.3 indicating there is a weaker association to the construct selfjudgement. Item 1 (‘I’m disapproving and judgemental about my own flaws and inadequacies’) shows the strongest association to this construct.
Tables 44 and 45 below show the item statistics (mean and standard deviation) and item to item correlations for the common humanity scale of the SCS at baseline. In summary the mean item score for this sub-scale is 2.04 with a range from 1.82–2.25 and variance of 0.43
TABLE 44: ITEM STATISTICS FOR SUB-SCALE COMMON HUMANITY AT BASELINE
| Common humanity | Mean | Std. Deviation | N | |
| SCS 3 | 2.25 | 1.14 | 177 | |
| SCS 7 | 2.20 | 1.25 | 177 | |
| SCS 10 | 1.82 | 1.06 | 177 | |
| SCS 15 | 1.92 | 1.09 | 177 | In table 44 n = 177 as 8 participants did not complete the measure and a further 2 refused/failed to complete at least 1 item on this sub-scale. |
TABLE 45: ITEM TO ITEM CORRELATIONS FOR SUB-SCALE COMMON HUMANITY AT BASELINE
| Common humanity | SCS 3 | SCS 7 | SCS 10 | SCS 15 | |
| SCS 3 | 1.00 | 0.43 | 0.32 | 0.39 | |
| SCS 7 | 0.43 | 1.00 | 0.45 | 0.35 | |
| SCS 10 | 0.32 | 0.45 | 1.00 | 0.45 | |
| SCS 15 | 0.39 | 0.35 | 0.45 | 1.00 | In the sub-scale common humanity correlations for each item are just above 0.3 indicating there is a weak, but acceptable association to the construct common humanity. Item 10 (‘when I feel inadequate in some way, I try to remind myself that feelings of inadequacy are shared by most people’) and item 7 (‘when I am down and out, I remind myself that there are lots of other people in the world feeling like I am’) showed the strongest association to this construct. |
Tables 46 and 47 below show the item statistics (mean and standard deviation) and item to item correlations for the sub-scale isolation at baseline. In summary the mean item score for this sub-scale is 1.85 with a range from 1.84–2.04 and variance of 0.20
TABLE 46: ITEM STATISTICS FOR SUB-SCALE ISOLATION AT BASELINE
| Isolation | Mean | Std. Deviation | N | |
| SCS 4 | 1.84 | 1.02 | 171 | |
| SCS 13 | 1.84 | 1.05 | 171 | |
| SCS 18 | 2.04 | 1.15 | 171 | |
| SCS 25 | 1.69 | 0.88 | 171 | In table 46 n = 171 as 8 participants did not complete the measure and a further 8 refused/failed to complete at least 1 item on this sub-scale. |
TABLE 47: ITEM TO ITEM CORRELATIONS FOR SUB-SCALE ISOLATION AT BASELINE
| Isolation | SCS 4 | SCS 13 | SCS 18 | SCS 25 | |
| SCS 4 | 1.00 | 0.18 | 0.30 | 0.30 | |
| SCS 13 | 0.18 | 1.00 | 0.52 | 0.13 | |
| SCS 18 | 0.30 | 0.52 | 1.00 | 0.19 | |
| SCS 25 | 0.30 | 0.13 | 0.19 | 1.00 | In the sub-scale isolation correlations item 4 (‘when I think about my inadequacies, it tends to make me feel more separate and cut off from the rest of the world’) and item 25 (‘When I fail at something important to me I tend to feel alone in my failure’) each score below 0.3 indicating there is a weaker association to the construct isolation. Item 18 (‘when I’m really struggling, I tend to feel like other people must be having an easier time of it’) shows the strongest association. |
Tables 48 and 49 below show the item statistics (mean and standard deviation) and item to item correlations for the sub-scale mindfulness at baseline. In summary the mean item score for this subscale is 2.16 with a range from 1.74–2.69 and variance of 0.95
TABLE 48: ITEM STATISTICS FOR SUB-SCALE MINDFULNESS AT BASELINE
| Mindfulness | Mean | Std. Deviation | N | |
| SCS 9 | 2.69 | 1.19 | 168 | |
| SCS 14 | 2.16 | 1.09 | 168 | |
| SCS 17 | 2.06 | 1.03 | 168 | |
| SCS 22 | 1.74 | 0.98 | 168 | In table 48 n = 168 as 8 participants failed to complete the measure and a further 11 refused/failed to complete at least 1 item on this sub-scale. |
TABLE 49: ITEM TO ITEM CORRELATIONS FOR SUB-SCALE MINDFULNESS AT BASELINE
| SCS 9 | SCS 14 | SCS 17 | SCS 22 | ||
| SCS 9 | 1.00 | 0.51 | 0.37 | 0.26 | |
| SCS 14 | 0.51 | 1.00 | 0.58 | 0.43 | |
| SCS 17 | 0.37 | 0.58 | 1.00 | 0.52 | |
| SCS 22 | 0.26 | 0.43 | 0.52 | 1.00 | In the sub-scale mindfulness correlations, item 22 (‘When I’m feeling down I try to approach my feelings with curiosity and openness’) is below 0.3 indicating there is a weaker association to the construct mindfulness Item 17 (‘When I fail at something important to me I try to keep things in perspective’) shows the strongest association to the construct. |
Tables 50 and 51 below show the item statistics (mean and standard deviation) and item to item correlations for the sub-scale overidentification at baseline. In summary the mean item score for this sub-scale is 1.92 with a range from 1.58–2.37 and variance of 0.52.
TABLE 50: ITEM STATISTICS FOR SUB-SCALE OVERIDENTIFICATION AT BASELINE
| Over-identification | Mean | Std. Deviation | N | |
| SCS 2 | 1.58 | 0.87 | 171 | |
| SCS 6 | 1.64 | 0.94 | 171 | |
| SCS 20 | 2.10 | 1.09 | 171 | |
| SCS 24 | 2.37 | 1.22 | 171 | In table 50 n = 171 as 8 participants failed to complete the measure and a further 8 refused/failed to complete at least 1 item on this sub-scale. |
TABLE 51: ITEM TO ITEM CORRELATIONS FOR SUB-SCALE OVERIDENTIFICATION AT BASELINE
| Overidentification | SCS 2 | SCS 6 | SCS 20 | SCS 24 | |
| SCS 2 | 1.00 | 0.35 | 0.30 | 0.25 | |
| SCS 6 | 0.35 | 1.00 | 0.20 | 0.30 | |
| SCS 20 | 0.30 | 0.20 | 1.00 | 0.44 | |
| SCS 24 | 0.25 | 0.30 | 0.44 | 1.00 | In the sub-scale overidentification correlations, item 2 (‘when I’m feeling down I tend to obsess and fixate on everything that is wrong’) and item 6, (‘when I fail at something important to me become consumed with feelings of inadequacy’) each score below or at 0.3 indicating there is a weaker association to the construct overidentification. Item 20 (‘When something upsets me I get carried away with my feelings’) shows the strongest association. |
Split half reliability for SCS at baseline
TABLE 52: SUMMARY ITEM MEANS FOR SCS AT BASELINE
| Mean | Minimum | Maximum | Range | Maximum / Minimum | ||
| Item Means | Part 1 | 1.92 | 1.40 | 2.68 | 1.27 | 1.90 |
| Part 2 | 1.92 | 1.50 | 2.33 |
2.68 | 0.83 | 1.55 |
| Both Parts | 1.92 | 1.40 | 1.27 | 1.908 | Variance | N of Items | |
| Item Means | Part 1 | 0.134 | 13a |
13b
26 |
| Part 2 | 0.053 | |
| Both Parts | 0.090 | a. The items are: SCS 1, SCS 2, SCS 3, SCS 4, SCS 5, SCS 6, SCS 7, SCS 8, SCS 9, SCS 10, SCS 11, |
SCS, 12, SCS 13
b. The items are: SCS 14, SCS 15, SCS 16, SCS 17, SCS 18, SCS 19, SCS 20, SCS 21, SCS 22, SCS 23, SCS 24, SCS, 25, SCS 26
Table 53 below shows the split half reliability for the SCS at baseline which demonstrated good internal consistency for the SCS.
TABLE 53: SPLIT HALF RELIABILITY SCALE STATISTICS FOR SCS AT BASELINE
| Mean | Variance | Std. Deviation | N of Items | ||
| Part 1 | 25.05 | 44.87 | 6.69 | 13a | |
| Part 2 | 24.98 | 50.35 | 7.09 | 13b | |
| Both Parts | 50.02 | 170.48 | 13.05 | 26 | a. The items are: SCS 1, SCS 2, SCS 3, SCS 4, SCS 5, SCS 6, SCS 7, SCS 8, SCS 9, SCS 10, SCS 11, |
SCS, 12, SCS 13
b. The items are: SCS 14, SCS 15, SCS 16, SCS 17, SCS 18, SCS 19, SCS 20, SCS 21, SCS 22, SCS 23, SCS 24, SCS, 25, SCS 26
Test-retest reliability for SCS at baseline
Table 54 shows the test-retest reliability for the SCS using Pearson Product Moment R correlation (Dancy, Reidy and Rowe 2012) comparing baseline with 6 months. The rationale for the time points for conducting test-retest reliability is given in chapter 3 of this thesis. At baseline the SCS was administered to 179 participants (N) and to 124 participants at 6 months. This is because the 6-month data collection point was collected by posting questionnaires to participants rather than the face to face interview that took place a baseline. This resulted in a 31.1% (56 participants) reduction in sample size. The Pearson correlation is the test-retest reliability coefficient and the sig. (2 tailed) is the P -value which indicates the statistical significance of the coefficient.
For the SCS the following factors, common humanity (0.61 P<0.01); mindfulness (0.57 P<0.01) and self-judgement (0.57 P<0.01) showed a moderate statistically significant test re-test reliability, whilst overidentification (0.48 P<0.01) Isolation (0.39 P<0.01) demonstrated a low, statistically significant test-retest reliability. Self-kindness (-0.04 P<0.59) showed no statistically significant test-retest reliability.
TABLE 54: TEST RETEST FOR SCS AT BASELINE AND 6 MONTHS (**. CORRELATION IS SIGNIFICANT AT 0.01 LEVEL (2 TAILED)
| Correlation | Self- |
Kindness baseline | Self-
judgement baseline | Common Humanity baseline | Isolation baseline | Over
Identification baseline | Mindfulness baseline | SelfKindness
6months | Self-
judgement
6months | Common Humanity
6months | Isolation 6months | Over
Identification
6months | Mindfulness
6months |
| Self-Kindness baseline | Pearson |
Sig.(2tailed) N | 1
180 | 0.41**
<0.01
180 | 0.53**
<0.01
179 | 0.18*
<0.01
180 | 0.38**
<0.01
180 | 0.50**
<0.01
180 | -0.04
<0.01
122 | 0.38**
<0.01
122 | 0.47**
<0.01
122 | 0.22*
<0.01
122 | 0.37**
<0.01
122 | 0.39**
<0.01
122 |
| Self-judgement baseline | Pearson Sig.(2tailed) |
N | 0.41**
<0.01
180 | 1
180 | 0.22**
<0.01
179 | 0.48**
<0.01
180 | 0.59**
<0.01
180 | 0.34**
<0.01
180 | -0.21
0.81
122 | 0.57**
<0.01
122 | 0.21*
<0.01
121 | 0.29**
<0.01
122 | 0.45**
<0.01
122 | 0.18*
<0.01
121 |
| Common Humanity baseline | Pearson |
Sig.(2tailed) N | 0.53**
<0.01
179 | 0.22**
<0.01
179 | 1
179 | 0.14*
0.04
179 | 0.27**
<0.01
179 | 0.60**
<0.01
179 | -0.81
0.38
121 | 0.23**
<0.01
121 | 0.61**
<0.01
120 | 0.10
0.25
121 | 0.37**
<0.01
121 | 0.49**
<0.01
120 |
| Isolation baseline | Pearson |
Sig.(2tailed) N | 0.18*
<0.01
180 | 0.48**
<0.01
180 | 0.14*
0.04
179 | 1
180 | 0.45**
<0.01
180 | 0.20**
<0.01
180 | -0.36
0.69
122 | 0.28**
<0.01
122 | 0.11
0.20
121 | 0.39**
<0.01
122 | 0.35**
<0.01
122 | 0.10
0.27
121 |
| Over |
Identification
Baseline | Pearson
Sig.(2tailed) N | 0.38**
<0.01
180 | 0.59**
<0.01
180 | 0.27**
<0.01
179 | 0.45**
<0.01
180 | 1
180 | 0.48**
<0.01
180 | -0.06
0.46
122 | 0.32** <0.01
122 | 0.18*
0.04
121 | 0.20*
0.02
122 | 0.48** <0.01
122 | 0.22*
<0.01
121 |
| Mindfulness baseline | Pearson |
Sig.(2tailed) N | 0.50** <0.01
180 | 0.34** <0.01
180 | 0.60** <0.01
179 | 0.20** <0.01
180 | 0.48** <0.01
180 | 1
180 | -0.09
0.30
122 | 0.31** <0.01
122 | 0.46** <0.01
121 | 0.22*
<0.01
122 | 0.38** <0.01
122 | 0.57** <0.01
121 |
| Self-Kindness |
6months | Pearson
Sig.(2tailed) N | -0.04
0.59
122 | -0.21
0.81
122 | -0.81
0.38
121 | -0.03
0.69
122 | -0.06
0.46
122 | -0.09
0.30
122 | 1
124 | 0.63** <0.01
123 | 0.62** <0.01
123 | 0.50**
<0.01
123 | 0.56** <0.01
123 | 0.55**
<0.01
123 |
| Self-judgement |
6months | Pearson
Sig.(2tailed) N | 0.38**
<0.01
122 | 0.57**
<0.01
122 | 0.23**
<0.01
121 | 0.28**
<0.01
122 | 0.32**
<0.01
122 | 0.31**
<0.01
122 | 0.63**
<0.01
123 | 1
124 | 0.36**
<0.01
123 | 0.57**
<0.01
124 | 0.68**
<0.01
124 | 0.30**
<0.01
123 |
Common Humanity
6months | Pearson
Sig.(2tailed) N | 0.47** <0.01
121 | 0.21*
<0.01
121 | 0.61** <0.01
120 | 0.11
0.20
121 | 0.18* 0.04
121 | 0.46** <0.01
121 | 0.62** <0.01
123 | 0.36** <0.01
123 | 1
123 | 0.31** <0.01
123 | 0.48** <0.01
123 | 0.64** <0.01
123 | 199
| Isolation |
6months | Pearson
Sig.(2tailed) N | 0.22*
<0.01
122 | 0.29**
<0.01
122 | 0.10
0.25
121 | 0.39**
<0.01
122 | 0.20*
0.02
122 | 0.22*
<0.01
122 | 0.50**
<0.01
123 | 0.57**
<0.01
124 | 0.31**
<0.01
123 | 1
124 | 0.53**
<0.01
124 | 0.28**
<0.01
123 |
| Over |
Identification
6months | Pearson
Sig.(2tailed) N | 0.37**
<0.01
122 | 0.45**
<0.01
122 | 0.37**
<0.01
121 | 0.35**
<0.01
122 | 0.48**
<0.01
122 | 0.388**
<0.01
122 | 0.56**
<0.01
123 | 0.68**
<0.01
124 | 0.48**
<0.01
123 | 0.53**
<0.01
124 | 1
124 | 0.38**
<0.01
123 |
| Mindfulness |
6months | Pearson
Sig.(2tailed) N | 0.39**
<0.01
121 | 0.182*
0.04
121 | 0.49**
<0.01
120 | 0.10
0.27
121 | 0.22*
<0.01
121 | 0.57**
<0.01
121 | 0.55**
<0.01
123 | 0.30** <0.01
23 | 0.64**
<0.01
123 | 0.28**
<0.01
123 | 0.38** <0.01
123 | 1
123 | 200
Confirmatory Factor Analysis (CFA) for SCS
Confirmatory Factor Analysis was conducted to test the six-factor model of the 26 item Self Compassion Scale (SCS) (n = 179, see above for description of sample). The number of cases with data missing on all variables was 12 and these were not included in the analysis. The CFA was assessed for exact model fit using WMSLV and Chi-square and for approximate fit using CFI, TLI and RMSEA. In assessing model fit (see table 55) the Chi-square p value of P<0.01 indicates no exact model fit. The approximate fit Chi -square (3484.54), CFI (0.920) and TLI (0.90) values indicate an acceptable fit. The RMSEA (0.070) demonstrates a close to good fit with the data sample.
TABLE 55: MODEL FIT INDICES FOR SCS
| Measure | 𝑥2 | CFI | TLI | RMSEA |
| SCS | 3484.54 |
P< 0.001 | 0.92 | 0.90 | 0.07 | The SCS CFA pathway (see figure 8 below) showed a strong positive association between over identification and self- judgement (0.92); common humanity and mindfulness (0.86); judgement and isolation (0.80); kindness and common humanity (0.78); isolation and over identification (0.77); Kindness and Self-judgment (0.70); kindness and mindfulness (0.76) and over identification and mindfulness (0.70).
A moderate positive association between kindness and overidentification (0.66) and self judgement and mindfulness (0.55).
A weak positive association between common humanity and over identification (0.49); judgement and common humanity (0.43); kindness and isolation (0.42); kindness and isolation (0.42); mindfulness and isolation (0.37) and common humanity and isolation (0.30).
232
FIGURE 8: CONFIRMATORY FACTOR ANALYSIS PATH DIAGRAM FOR THE SELF COMPASSION SCALE (SCS)
(see appendix XIV for item statements 1–22 presented in their six factor clusters)
K=Kindness, SJ=Judgement, CH=Common Humanity, I=Isolation, M=Mindfulness OI=Overidentification
202
Objective 2: To determine how levels of shame, self-criticism and self-compassion correlate with level of depression
The second objective of this PhD study was to examine the degree to which variance in scores on depression measures taken at baseline can be accounted for by variance in levels of shame, self-criticism and self-compassion. Both univariate and multivariate regression analyses were conducted using the statistical package STATA (Stata Corps, 2013) to explore the possible association between baseline scores on HDRS-17, BDI-I and PHQ-9 and each total score on the OAS, FSCRS, SCS.
The following analyses were conducted:
-
Univariate regression analysis was carried out to regress each individual baseline score on the HDRS-17, BDI-I and PHQ-9 (each treated as a single dependent variables) against the individual total score for the OAS, FSCRS and SCS (each treated as a single independent variable).
-
Multivariate regression was carried out to regress each baseline score on the HDRS17, BDI-I and PHQ-9 (each treated as a single dependent variables) against the collated total scores of each of the OAS, FSCRS and SCS. The results are tabulated below in tables.
-
All univariate and multivariate modelling was rerun with missingness imputed by means of multiple imputation under the missing at random assumption. The results were a sensitivity analysis to check the robustness of regression parameters sensitive to missing data. The results obtained with both the observed data and missing data imputed are consistent and therefore only the observed data results were reported.
Tables 56, 57 and 58 show the univariate and multivariate regression analyses for the OAS, FSCSR and SCS against the HDRS-17, BDI-I and SCS respectively. The following regression parameters are shown: 95% confidence intervals, R2, p value and regression coefficients.
Table 56 shows the univariate and multivariate regression modelling for HRSD-17 with the OAS, FSCSR and SCS.
TABLE 56: INFLUENCE OF OAS, FSCSR AND SCS ON HRSD-17 BY UNIVARIATE AND MULTIVARIATE REGRESSION MODELLING
| Measure | Univariate | Multivariate | ||
| HDRS-17 | Coefficient (95% CI) P = | R2 | Coefficient (95% CI) P = | R2 |
| OAS | 0.10 (-0.04–0.25) P = |
0.07 | 0.09 | 0.08 (-0.07–0.24) P =
0.09 | 0.11 |
| FSCSR | 0.12 (0.09–0.14) |
P =< 0.01 | 0.05 | 0.05 (0.00-0.10) P =
0.04 | 0.11 |
| SCS | -0.09 (-0.22-0.03) |
P = 0.09 | 0.06 | -0.02 (-0.08-0.03) P =
0.12 | 0.11 | From the univariate data the following can be inferred. There is a positive association between HDRS-17 and OAS (coefficient 0.10, P value of 0.07), this is outside the chosen level of 0.05 significance, with an R2 value of 9% and a negative confidence interval value at zero (-0.04 - 0.25). There is a positive association between HDRS-17 and FSCSR (coefficient 0.12, P = <0.01) which is within the chosen level of 0.05 significance, with an R2 value of 5% and confidence intervals at zero (0.09 - 0.14). There is a negative association between HDRS-17 and SCS (coefficient -0.09, P = 0.09) which is outside the chosen level of 0.05 significance, with an R2 value of 6% and a negative confidence interval value at zero ( -0.22 - 0.03).
Overall, these results can be summarised as there being a significant positive association between scores on the OAS and FSCSR and severity of depression as rated on the HDRS17. Likewise, there is a significant negative association between scores on the SCS and severity of depression as rated on the HDRS-17.
The multivariate data shows the R2 value for this data is 11%. From the multivariate data it can be inferred there is a positive correlation between the HDRS-17 and OAS
(coefficient 0.08) and FSCSR (coefficient 0.05) and a negative correlation with the SCS (coefficient -0.02). For the OAS (P= 0.09) and SCS (p= 0.12) the P values are outside the chosen level of 0.05 significance. The P value for the FSCSR (P = 0.04) is within the chosen level of 0.05 significance. The confidence intervals for the OAS (CI = — 0.07 — 0.24) and the SCS (CI= — 0.08 — 0.03) are at zero each with one negative anchor. The confidence intervals for the FSCSR (CI= 0.00- 0.10) are at zero.
Overall, the severity of depression on the HDRS-17 has a relatively small effect on the OAS, FSCSR and SCS. The only significant but very weak correlation, controlling for age, gender and centre is the FSCSR.
Table 57 shows the univariate and multivariate regression modelling for BDI-I with the OAS, FSCSR and SCS.
TABLE 57: INFLUENCE OF OAS, FSCSR AND SCS ON BDI-I UNIVARIATE AND MULTIVARIATE REGRESSION MODELLING
| Measure | Univariate | Multivariate | ||
| BDI-I | Coefficient (95% CI) P |
= | R2 | Coefficient (95% CI) P
= | R2 |
| OAS | 0.29 (0.20–0.38) P = |
0.01 | 0.27 | 0.22 (0.12–0.32) P =
0.02 | 0.34 |
| FSCSR | 0.28 (0.18–0.38) |
P= <0.01 | 0.05 | 0.07 (-0.39–0.54) P=
0.28 | 0.34 |
| SCS | — 0.27(-0.46 — -0.08) |
P= 0.02 | 0.21 | -0.16 (-0.62–0.29) P =
0.13 | 0.34 | From the univariate data it can be inferred there is a positive association between the BDI-I and OAS (coefficient 0.29, P = 0.01) which is within the chosen level of 0.05 significance, with an R2 value of 27% and confidence interval values at zero (0.20 — 0.38). There is a positive association between the BDI-I and FSCSR (coefficient 0.28 p = 0.00) which is within the chosen level of 0.05 significance, with an R2 value of 5% and confidence interval values at zero (0.18 — 0.38). There is a negative association between
BDI-I and SCS (coefficient -0.27, P = 0.02) which is within the chosen level of 0.05 significance, with an R2 value of 21% and negative confidence interval values at zero ( —
0.46 — 0.08).
Overall these results can be summarised as there being a significant positive association between scores on the OAS and FSCSR and severity of depression as rated on the BDI-I. Likewise, with there is a significant negative association between scores on the SCS and severity of depression as rated on the BDI-I.
From the multivariate data it can be inferred there is a positive correlation between the BDI-I and OAS (coefficient 0.22) and FSCSR (coefficient 0.07) and a negative correlation with the SCS (coefficient -0.16). For the OAS (P = 0.02) the P value is within the chosen level of 0.05 significance, whilst the P values for the FSCSR (P= 0.24) and SCS (P = 0.13), are outside the chosen level of significance. The confidence intervals for the OAS are at zero (CI = 0.12 — 0.32). The confidence intervals for the FSCSR (CI = -0.39 — 0.54) and SCS (CI= -0.26 — 0.26) are at zero with both FSCSR and SCS each possessing one negative anchor.
Overall, controlling for age, gender and centre the severity of depression on the BDI has a mild, significant effect on the OAS scale and a non-significant effect on the FSCSR and SCS.
Table 58 shows the univariate and multivariate regression modelling for PHQ-9 with the OAS, FSCSR and SCS.
TABLE 58: INFLUENCE OF OAS, FSCSR AND SCS ON PHQ-9 UNIVARIATE AND MULTIVARIATE REGRESSION MODELLING
| Measure | Univariate | Multivariate | ||
| PHQ-9 | Coefficient (95% CI) P = | R2 | Coefficient (95% CI) P = | R2 |
| OAS | 0.13 (-0.03–0.30) P = 0.06 | 0.20 | 0.11 (0.10–0.13) P<0.01 | 0.21 |
| FSCSR | 0.11 (0.04–0.17) P = 0.01 | 0.07 | 0.00 (-0.15–0.17) P = 0.71 | 0.21 |
| SCS | -0.10 (-0.24–0.03) P = 0.09 | 0.10 | -0.03 (-0.25–0.17) P = 0.27 | 0.21 |
From the univariate data there can be inferred a positive association between the PHQ-9 and OAS (coefficient 0.13, P = 0.06) which is outside the chosen level of 0.05 significance, with an R2 value of 20% and negative confidence interval values at zero (-0.03 — 0.30). There can be inferred a positive association between the PHQ-9 and FSCSR (coefficient 0.11 P = 0.01) which is within the chosen level of 0.05 significance, with an R2 value of 7% and confidence interval values at zero (0.04 — 0.17). There can be inferred a negative association between PHQ-9 and SCS (coefficient -0.10, P = 0.09) which is outside the chosen level of 0.05 significance, with an R2 value of 10% and negative confidence interval values at zero (-0.24 — 0.03).
Overall, these results can be summarised as there being a non-significant positive association between scores on the OAS and severity of depression as rated on the PHQ9. There is a significant positive association between scores on the FSCSR and severity of depression as rated on the PHQ-9. There is a non-significant negative association between scores on the SCS and severity of depression as rated on the PHQ-9.
For the multivariate data the R2 value is 21%. From this data it can be inferred a positive association between the PHQ-9 and OAS (coefficient 0.11 and FSCSR (coefficient 0.00) and a negative association with the SCS (coefficient — 0.03). For the OAS (p= 0.00) and the SCS (P = 0.03) the P value is within the chosen level of 0.05 significance, whilst the P value for the FSCSR (P= 0.71) is outside the chosen level of significance. The confidence intervals for the OAS are at zero (CI= 0.10 – 0.13). The confidence intervals for the FSCSR (CI= 0.15 — 0.17) and the SCS (CI= -0.25–0.17) are at zero with each possessing a negative anchor. Overall, controlling for age, gender and centre there is a very weak but significant association between the OAS and severity measured on the PHQ-9 and no association with the FSCSR and SCS.
Chapter 5 Qualitative results
This chapter presents the results of the qualitative data analysis which addresses the third question posed in this thesis:
How do participants diagnosed with persistent, treatment resistant depression experience about shame, self-criticism and self-compassion?
As described in chapter 3 of this thesis, research data can be categorised as quantities (expressed in numbers) and qualities (expressed in words) and in the mixed methods approach these are viewed as two forms of information and two modes of representation (Biesta, 2010). This chapter is concerned with data as qualities expressed in words and text, which was analysed using Interpretative Phenomenological Analysis (IPA), (Smith, Flowers and Larkin, 2009).
The steps of data analysis are described in chapter 3 of this thesis. In appendix XXXI there is an example of a section of the steps in data analysis from transcription to round one of the analysis of descriptive, conceptual and linguistic observations from each transcript. These were then converted into a mind map for each participant an example of which is shown in appendix XXXII. In keeping with the ‘interpretative’ component of IPA (Smith 2004) the researcher is encouraged to go beyond analyses that merely describe the content of a transcript but to consider deeper levels of interpretation. With this in mind, the author attempted to excavate further and examine the meaning behind the language, idioms and metaphors used by the participants. In addition, as part of the analysis process, adjectives, idioms and metaphors that were triggered in the mind of the author of this thesis whilst engaging with each transcript were also considered as part of the interpretation and analysis of text data. These are cited at relevant points in this chapter. A theoretical rationale for taking this approach is given in the reflexivity section below. Throughout this chapter the person referred to as interviewer is the author of this PhD thesis.
Reflexivity
In any research endeavour, it is important to give heed to the context, language and culture which function as frameworks for the construction of meaning. As Wright, Callaghan and Bartlett (2011) observe the context of an interview is not a neutral data collection tool but an interaction ultimately bound by context. In discussing the concept of reflexivity in qualitative research Malterud (2001) observes:
‘a researchers background and position will affect what they choose to investigate, the angle of investigation, the methods judged most adequate for this purpose, the findings considered most appropriate and, the framing and communication of conclusions’
(Malterud, 2001, p 483–484)
As a consequence the researcher is beholden to identify the preconceptions that are brought to the research endeavour which, as Malterud describes, are an amalgamation of the researchers previous personal and professional experiences, ideas and preconceptions about the chosen area of study, motivation for exploration in this field and theoretical and clinical focus of the researcher. Malterud argues that preconceptions are not the same as biases if they are identified from the outset of the research endeavour and reflexivity is used proactively to manage these preconceptions throughout the research process.
Brookfield’s Critically Reflective Practice Model (Brookfield, 1998), which is derived from education, was adapted to focus and structure the process of reflexivity in a research setting. Brookfield encourages the use of four critically reflective lenses to examine the assumptions which underpin our investigations. The adaptation made in this thesis was to change the focus of one lens (the second) from ‘Our Learners Eyes’ (Brookfield, 1998, p 199) to ‘Our Research Supervisors Eyes’. As Brookfield observes building an awareness of our assumptions ‘is a puzzling and contradictory task’ and he likens the process to a person trying to see the back of their head whilst looking in a mirror. (Brookfield, 1998, p 197).
The reflective lenses used were:
-
Our Autobiography: our own individual experiences and the meanings we derive from these and how these shape our intellectual and practical research pursuits
-
Our research supervisors’ Eyes: Seeing our research practice through the eyes of our research supervisors
-
Our Colleagues’ Experiences: Engagement in critical conversation with peers
-
Theoretical, Philosophical and Research literature: Using theory, philosophy and academic literature to explore perspectives and interpretative frames
In terms of ‘autobiography’ (lens 1) personal experiences of family mental illness in childhood have shaped my view of depression. Experience has led me to view depression as an illness which, whilst for some it waxes and wanes, for others it persists, others it remits and yet for others it is fatal. Further, for both self and other(s) (be this the sufferer themselves, their family member, friends, professionals involved in their care, the bystander) depression has both an objective reality and a subjective experience. For example, objectively, there are observable changes in the person, which can be labelled signs and symptoms which impact both self and other(s), interfering significantly with day to day functioning. Equally there is the subjective experience, manifest in both self and other(s), the way in which the internal world is constructed and construed through the depressive experience of self or other(s). I am trained as a mental health nurse. I was educated in both the signs and symptoms of mental illness and their treatment using pharmacotherapy, ECT and in the role of counselling (person -centred) and psychotherapy ( behaviour therapy, psychodynamic psychotherapy and gestalt therapy) , in the treatment of mental illness and alleviation of psychological distress. Over the course of my career, in conversation with my psychotherapy colleagues I have learned that these childhood experiences and my chosen profession are not coincidental.
Undoubtedly my two PhD supervisors (lens 2) (a professor of mental health nursing and a professor of psychiatry) have greatly influenced my perspective regarding the research process. We have examined and debated assumptions and beliefs about the nature of reality and through discourse and interrogation of the literature the ‘Primacy of Practice’ (Biesta, 2010; Hookway, 2006; Dewey, 1938) forms the epistemological foundation of this thesis.
In the context of this PhD I have engaged in critical debate with three specific colleagues (lens 3). A mental health nurse who qualified in 1976, with training in cognitive behavioural psychotherapy working in this field for thirty years; a social worker who qualified in 1995 with training in psychodynamic psychotherapy, working in this field for twenty years and a person with 25 years lived experience of depression who has never undertaken psychological treatment for the problem.
In terms of my own interpretative frame (Lens 4) this has been shaped by several educational experiences. I studied philosophy and politics at university (prior to my undertaking my professional training) and it is here I was introduced to the philosophy of Pragmatism (Hookway, 2006; 2002). Equally, as a practitioner of cognitive therapy for twenty-seven years, inevitably the theoretical and clinical principles of Beckian cognitive theory and therapy (Moore and Garland, 2003; Beck, Rush, Shaw and Emery, 1979) underpinned the author’s analytic processes when interrogating the qualitative data. This includes the conceptualisation of depression as a diagnosable illness, as well constructing meaning from the data and as part of the decision-making process in defining the descriptors for themes identified in this IPA analysis. Interpretative Phenomenological Analysis is described as an ‘integrative approach’ (Smith, Flowers and Larkin, 2009), where ‘integrative’ is defined with reference to the caveat that, provided the three core theoretical principles of IPA are honoured in data collection and analysis, then IPA researchers may draw on theoretical frameworks across the spectrum of mainstream psychology as part of the process of interpretative analysis.
These three core principles are (Smith, Flowers and Larkin 2009 p 186):
-
The study focus examines the phenomenological experience of the participants
-
The researcher embarks upon a process of ‘intense interpretative engagement’ with the verbal account provided by the study participants
-
Each case is subjected to a detailed analysis
Ensuring adherence to these three principles involved the following. Firstly, maintaining a focus on the phenomenological experiences of the client was ensured by recording and transcribing the interviews. Each recording was reviewed twice. Each transcript was read and re-read at least three times. Notes were made in accordance with the data analysis phases of IPA (Smith, Flowers and Larkin 2009) (see chapter 3 for a description of these phases and appendices XXXI and XXXII for examples of data collection and analysis). During the review of recordings specific attention was paid to the form and content of language (i.e. use of idioms and slang) and paralanguage and to voice tone and sections of recording where active affect was present. The purpose in listening to each recording on two separate occasions was part of reflexivity. Noticing and noting similarities and differences in my interpretation on each occasion and discussing these observations with the colleagues identified above. This also contributed towards conforming to the second principle of ‘intense interpretive engagement’. In addition, the data derived from each interview was recorded in written form using the format described by Smith, Flowers and Larkin (2009) (see appendix XXXI for an example). Given the volume and richness of the data collected and the multifaceted focus of investigation (shame, self-criticism, self-compassion and depression) the organised and linear nature of the recommended process felt flat and restrictive and so a decision was taken to also draw a mind map for each participant (see appendix XXXII for an example). This assisted significantly in giving a visual representation of the data with potential interconnected themes (i.e. shame and pride). Further, this enabled a distilling of the data leading to the emergence of the themes and sub-themes reported here. The reported speech of each participant formed the heart of the data analysis process and this reported speech is cited verbatim to exemplify the emergent themes and sub-themes. Reflexivity was also used to maintain the integrity of adherence to the IPA process.
Further, Smith and colleagues identify ‘cognition’ as being a central aspect of the IPA approach. Their definition of cognition in the context of IPA for both researcher and participant are summarised in table? below (from Smith, Flowers and Larkin, 2009 p 193):
TABLE 59: DEFINITION OF ‘COGNITION’ WITHIN IPA
Cognition and IPA
-
Everyday cognition as ‘subject’ for IPA:
pre-reflective reflexivity; Intuitive reflection; awareness; consciousness; hot cognition; rumination; sense making, meaning making
-
Self-conscious cognition as ‘process’ of doing IPA
Analysis; interpretation; sense-making; formal connecting with theory | This definition of cognition has been criticised (see Willig, 2001 and Langdridge, 2008) on the grounds it is not consonant with how cognition is defined within cognitive psychology, which in turn, is at odds with the hermeneutic philosophy which underpins IPA. Smith, Flowers and Larkin, (2009) aim to counter this criticism by stating: ‘We don’t see this cognition as a compartmentalised activity-it is dynamic, emotional and embodied’. The purpose of IPA being ‘sense-making’ and ‘meaning-making’ as a mechanism for learning about how participants relate to the world. They conclude by arguing that IPA research can ‘clearly ‘speak to’ cognitive psychology’ by relating accounts of participants ‘identifiable experience’ back to psychological theories (Smith, Flowers and Larkin, 2009, p 194).
This definition of cognition as ‘dynamic, emotional and embodied’ (Smith, Flowers and Larkin, (2009) is consonant with the authors own conceptualisation of cognition and emotion within a cognitive psychotherapy frame and is shaped by Teasdale’s Interacting Cognitive Subsystems (ICS) model of memory in depression (Teasdale, 1999; Teasdale and Barnard, 1993). In this regard, Teasdale defines two distinct forms of meaning, propositional and implicational, each representing different aspects of experience. Propositional meaning refers to specific concepts and their relationship to one another e.g. ‘the cat sat on the mat’ (Teasdale, 1999, p 147). Meaning at this propositional level is explicit and readily understood and corresponds to the meaning conveyed by single sentences in everyday language. This from of meaning can be assessed and examined by the scrutiny of data and collection of evidence. Importantly this level of meaning has no direct connection to emotion. Meanwhile, implicational meaning represents prototypical features, themes and complex interrelationships derived from the patterns of propositional meaning and sensory events that recur across experiences and which share profound similarities, even though at a surface level this may not appear so. These meanings are implicit and do not have a truth value that can be tested. Sensory experiences such as voice tone or smell, alongside proprioceptive experiences derived from bodily sensations related to facial expression or posture or touch can directly contribute to implicational meaning. Implicational meaning is not easily or readily conveyed and its synthesis is associated with ‘felt senses’ (Teasdale, 1999). Felt senses are defined as feelings with implicit meaning content and only this level is directly related to the generation of emotion. Propositional meanings only indirectly contribute to the generation of emotion through feeding into emotion-related implicational meanings. Teasdale and Barnard (1993) use poetry to exemplify their definition of implicational meanings as defined by Teasdale (1999):
‘The relationship between specific and generic meanings is analogous to the relationship between the letters that make up a sentence and the meaning of the sentence. A sentence conveys a specific meaning that is qualitatively different from and greater than the sum of its individual letters. In the same way, the generic meaning of a schematic model is qualitatively different from and greater than the sum of the patterns of specific meaning
that contribute towards it. Poetry illustrates this relationship…. the total effect of the poem
cannot be conveyed by a single specific meaning, nor can it be reduced to the sum of the components contributing towards it’
(Teasdale, 1999, p 148).
The author of this PhD thesis has published work examining the use of poetry in the construction of meaning in mental health practice (Roe and Garland, 2011). This paper gives a more detailed clinical illustration of Teasdale’s’ model in which the two authors used poetry and songs (lyrics and music) to construct a shared understanding and engage in the endeavour of cognitive therapy. In this chapter of this thesis I have drawn on the participants’ use of metaphors and idioms, dialectical terms and slang as a foundation for understanding the meanings they convey when speaking about depression, shame, self-criticism and selfcompassion. This process of analysis is underpinned by Teasdale’s model which is a revision of Beckian cognitive theory, informed by research in the field of cognitive science of depression (Harvey, Watkins, Mansell and Shafran, 2004; Williams, Watts, MacLeod and Mathews, 1997).
The cohort
Participants in the qualitative interviews were recruited from the control arm of the RCT cohort (n= 94) by the research associates who collected the quantitative data in the trial. The rationale for only recruiting from the control arm of the trial is given in the methods chapter of this thesis. The research associates were instructed to recruit a representative sample that reflected the demographic range of the trial cohort. This is described in the introduction to the quantitative results chapter. At the author’s request the research associates were asked to also consider which participants would be able to engage in an interview of 90 minutes duration and answer questions regarding their experience of depression, shame, selfcriticism and self-compassion. At the point of recruiting to the qualitative arm, the RCT research team were already aware that some participants found completing the measures tested in this PhD thesis aversive and this was taken into consideration as part of the selection process. The implications of this observation and its possible influence on the recruitment process and therefore the results presented is examined more fully in the discussion chapter.
Ten participants from the control arm of the RCT were recruited, informed consent obtained (see appendix XI for an example of the consent form which was amended for the purpose of obtaining consent for qualitative data collection) and interviewed. The sample was 50% male and female. The age range was 25 to 64 years with a mean of 51 years. Regarding employment status 40% were employed on a full-time basis (4 men), 40% were retired on grounds of ill health (2 as a result of depression (1 male and 1 female) and 2 (1 male and 1 female) as a result of physical health problems and 20% engaged in other employment (2 (female) voluntary work) and 60% were in receipt of benefits (3 males and 3 females). Regarding relationships, 40% of the cohort were married (1 male and 3 females), 20% were divorced (2 males) and 40% were single (2 males and 2 females) and 50% had one or more children (2 males and 3 females). Regarding education 40% left school at age 16 (2 males and 2 females), 40% were educated until age 18 or apprenticeship (2 male and 2 female) and 20% were university educated (1 male and 1 female). Nine participants described their ethnicity as white British and one as Black British of Afro-Caribbean heritage. A brief biography of each participant can be found in appendix
Emergent themes and sub-themes in the qualitative data
The following emergent themes and sub-themes were identified:
1. Childhood adversity and social milieu
i. No expectation
ii. Every expectation iii. Behind closed doors iv.
Reluctance to speak
about childhood
2. Sense of self
i. not good enough/inferior/failure- self-criticism ii. unimportant/not counting/not worthy-self-blame iii.
Bad//inadequate/insignificant/worthless-self-hate/loathing
3. The function of self-criticism 4. Absence of self-compassion
i. Incomprehension
ii. Risky iii. Not deserved
5. Avoidant coping 6. Memory biases and information processing biases in depression
1. Childhood adversity and the social milieu
All ten participants referred to their childhood as contributing to their experience of depression and their sense of self and self in relation to others. The memories of childhood were, by some participants, painfully recalled within the interview and the sense of fear, shame, humiliation, rejection and not only the absence of parental affection and care, but the overt antipathy exhibited towards them was at times palpable in the room. Their subjective reports of childhood can be seen to exist on a continuum of experiences that are defined in academic and clinical terms as emotional, physical and sexual abuse or neglect (Andrews, 1998).
(i) No expectation
Participant 8, (a man age 48), described, since childhood, always being ‘very fearful of things’ ( transcript 6, p 7, line 164) describing the area in which he was raised (an ex-mining community) as ‘rough’ …’you have always got to watch your back all the time’ (p 7, line 168170). He describes his parents as ‘my parents have always cost me’ (emotionally) (p 8, line 155). He went on to recall a childhood memory of his dad as follows:
‘I remember once when I was with my dad, before they got divorced, so I was ten and I said something like, ‘I can count to ten in French dad’ and he said (participant mimics his father’s sarcastic, gruff, ridiculing and dismissive voice tone and recreates his derisory and disgusted facial expression) ‘you want to learn to count to ten in English first’, something like that, not encouraged you know and that is my life, it is my parents, never well done or anything like
that’ (P 12, lines 263–267)…. I look back on it now and it affects me now, it does, that is the
end of your conversations with your dad, don’t go anymore into it’
(p 13, lines 287–288).
In another example from participant 8, speaking about the memory of counting to ten in French, feelings of sadness were resurrected (conveyed in a tone that was infused with sadness, anxiety and a hint of anger) and when asked how he felt at recalling the memory he observed the following, by the end of which he was crying and his facial expression one of sad bemusement:
‘disappointment again at my father, you know in the nineties I used to work on a summer camp in the States, so I know about children and how to encourage them and get the best
out of them and make them feel a bit better about themselves, but they (his parents) never
had any of these skills. They weren’t nasty people by any account, they weren’t horrible, they never did anything wrong, but you know maybe my personality just would not fit within that family environment ever, so I curbed my personality, to such an extent now where I don’t
have anything, I think I could have been something, I really do I think, but you know, I’m a
taxi driver, unbelievable, I could have done anything I am sure’
(transcript 6, p 13, lines 294–302)
Participant 136, (a man aged 54), described up to age 11 as being raised in a similar community:
‘brought up rough and ready….we all were where we used to live….I think it was where we lived (an ex-mining community)…I think in a way we had our own little world down there’ (participant 136, transcript 3, p 9 lines 286–293).
He described how as children the families in the community (not just his) functioned:
‘fight a lot…. we just went wild really…the parents would be at the pub…we would be on the
streets, it was normal for us’
(participant 136, transcript 3, p 9 lines 297–306).
He described his experience of being parented as follows:
‘No hugs from mum, she was not the type, born and bred down there…. never saw dad, either working or at the pub’
(transcript 3, participant 136, p 17, lines 450 and 462)
Interestingly, at age 11 the parents of participant 136 were divorced and his mother moved him and his siblings to a more affluent community and he observed the following:
‘mum left dad and moved to **** I was out of my depth…oh I had the posh uniform on…if
I’d had a **** upbringing (naming the area of the city the family moved to)I would be kinder
to myself’
(transcript 3, participant 136, p 10, 276–287).
Both participants 8 and 136 describe childhood environments where they were physically provided for (food, clothes and shelter) but were subjected to emotional neglect and an absence of parental affection and care, which in turn impacted on sense of self and sense of self in the mind of the other. This sense of self and sense of self in the mind of the other is reflected in their testimony in the other themes observed in this chapter.
(ii) Every expectation
Three of the participants (participants 9, (a woman age 25), 16, (a man aged 56) and 28, (a woman aged 51) described childhood environments (both home and school) where there was an imperative to perform to a certain standard or to meet a certain set of expectations. All described varying degrees of a sense of self as ‘not having met the mark’ and thus in some way disappointing significant others, their sense of self being shaped by this and feelings of shame at having not met expectation. This is reflected in their testimony in the other themes observed in this chapter.
Participant 9 articulated a range of ‘should statements’ often in relation to depressed mood such as: ‘I should be able to control my depression’ ‘I should be able to control my thinking and not think like this’ (referring to self-critical thinking) and ‘there should be something I should be able to do to get myself out of it (depression) it is something I have done to get in to it’ and a more global demand of self ‘I should be perfect’. Many of her ‘should statements’ were connected to her upbringing and her interpretation of her Christian faith and a strong sense of being a disappointment in the eyes of God.
Participant 28 described her own expectations to be productive as follows:
‘I love sitting in the garden and you know I have told myself, I have talked to myself about something, I have battled and I thought, if I go outside and sit on the chair on the patio and I might even go out and sit and I will wait about two minutes and then I will get up because in my head I start thinking I have got things to do… my thoughts just go I have got things to do,
you can’t’
(participant 28, p 8, lines 184–188)
and whilst reflecting on allowing time for herself she observed:
‘I should be doing things, in my head, in my heart I don’t have to do other things, but in my head, it is, yes, you have got to do this, you have got to shampoo the carpet, you have got to
do the washing, you know, and normally this is me’
(participant 28, p 11, lines 260–262).
and a sense ‘I don’t think I should enjoy things, not really enjoy things in life’ (participant 28,
p 13, line 294).
(iii) Behind closed doors
Participants 28 (a woman age 51) and 88 (a woman age 43) disclosed family secrets which they knew to be shameful from an early age and which they perceived had significantly shaped their sense of self. This sense of self is reflected in their testimony in the other themes observed in this chapter.
Participant 28 spoke about her fathers’ alcoholism:
‘I think shame originally came from my dad, he was an alcoholic and my mum was very strong and she got on with things and I think the shame was kind of there as a child because
I recognised what my dad was and he wasn’t like the fathers in the street and I think that is
where the shame originally came’
(transcript 5, participant 28, page 4–5 lines 94–97).
Participant 88: disclosed childhood sexual abuse by a (now deceased) family member:
‘It was totally different in them days, until I was actually 16 and reading a magazine article before I realised it had happened to anyone else in the world….I was shocked, I thought I was the only one right up until that age I thought I was the biggest freak in this world…..I knew it
was wrong, even at a young age I knew it was wrong…..it was always a big secret and well it
was horrible…..why are you doing this to me?…I knew it was wrong, you have nowhere to
go….’
(transcript 1, page 15, lines 359–369)
She continues by giving poignant account of her mother finding out about the sexual abuse using language imbued with a sense of shame:
‘my brother told her because it happened to him as well and I did not know but we found out when he got drunk and he blurted it out, well I was mortified, I would have taken the secret
to my grave’.
(transcript 1, p 16 lines 398–401)
In examining the language used by participant 88 The word ‘mortified’ means being made to feel uncomfortable because of shame. The idiom ‘taking a secret to the grave’ can refer to the concealment of an act that is shameful or would be if it became public knowledge and would have devastating repercussions. This is how participant 88 described her sense of shame, which continues to the present day, but to a lesser degree since its disclosure:
‘I am ashamed that it happened and ashamed of myself for not telling, ashamed of my family, I did not want people to know because it was too shameful. Now, since I’ve been volunteering at Mind….and finding out more about it and I feel at home there you see, as I feel safe there, because I am among people who understand and you know people come there who have been abused and I can help them as well and so it feels quite, it is quite a
safe place there, so I don’t feel so ashamed now than I used to, before it was like ‘oh it’s too
shameful to mention’ but I don’t mind talking about it to anybody.’
(transcript 1, p 17- 18, lines 432–440).
Participant 88 also shared how her abuser ensured her silence and she conveyed eloquently in both words and voice tone the helplessness and powerlessness of her childhood:
‘I was scared he was going to kill me…..he was big and it was like this big monster laid on top of me and my head used to be under his belly while he was on top of me and I thought oh he is going to suffocate me and kill me and he used to drag me downstairs and hurt me and thump me in the stomach and I thought he was going to kill us all because he used to hit her (her mother) as well you see so that’s why I could not really tell my mum because I think he would have murdered us all.’
(transcript 1, p 17 lines 416–424)
This testimony conveys the extreme nature of the devaluing and shaming experiences perpetrated against participant 88 from a young age and the abusers use of fear, intimidation and violence to ensure her silence and compliance.
Reluctance to speak about childhood
Three participants 15, (a man age 59), 20, (a man, aged 52) and a participant 11 (a woman, aged 52) were to varying degrees guarded throughout the interview and made only passing references to their childhoods. In each of these interviews feelings of shame felt present in the room during the interview as each participant engaged in conversation. For participants 11 and 20, this was conveyed in their parsimonious use of language and their clipped and subdued voice tone.
For example:
Participant 20 made only one statement (perhaps understatement is a more accurate description) about his family environment:
‘I have had bad things in my childhood, I had a dad that was less than a perfect father’ (transcript 2, page 11, line 277).
Whilst recounting this his voice tone became low, his words trembled as he spoke and the content changed to a more self-critical stance (criticising himself for beating himself up) which eventually petered out to silence and a downcast gaze as, as if caught up in a painful recollection as follows:
‘all of these things, I am sure other people, I think, and I can’t help but think, well they got
over it, they don’t continue to beat themselves up over things….’
(transcript 2, page 12, lines 278–280).
Participant 11 was of Afro-Caribbean heritage which may have impacted how comfortable she felt in the interview. It is highly likely, given her age and the environment in which she was raised, she had, throughout her life (including childhood) been subjected to racial discrimination, bullying and harassment. Thus, there was potential for her to implicitly fear judgement in the interview which may have in turn have activated feelings of shame and avoidant coping strategies in situ. She made the following observation regarding her childhood:
‘I was always insecure as a child, you know going back (in her mind not in this interview) to mother, I was very close to my mum and still am now and I was-when I went to school it traumatised me that I had got to leave my mum and I think it went on from there…those years of insecurity because I always felt sheltered’
(transcript 10, p 11, lines 200–206).
The interview with participant 15 was challenging. The interview took place at home and he remained dominant and in charge in the room. Throughout, his voice tone was measured and controlled, but with a sense that anger and shame simmering beneath. His speech was often hesitant, he was over inclusive in his self-report and frequently changed the subject, sometimes mid-sentence. These behaviours can be markers of avoidant coping, which in turn may have been a marker for shame being present in the interaction (this concept, inherent in Gilbert’s formulation of shame (Gilbert, 2017a; 2007a) is discussed more fully in the final chapter of this thesis). He made a single reference to his childhood and a sense of not having met his father’s expectations which he spontaneously updated with a present-day example where he perceived he continued not to meet expectation. The link between the childhood memory and current experience is, sense of self as a failure:
‘feeling a failure, feeling as if you have not lived your life to the expectance of what you are supposed to and at times I look back and I blame my dad for my upbringing, he was very strict…mum was soft if you put it that way, my dad was strict, it was because of him I left home at 18 and went in to the forces. The trouble I have is at times I think, well I can do that and I will go and do that, like cut the grass. I can get so far and then because I start and then my head starts, I sweat so badly, I get out of breath and I have to sit down and somebody else has to finish it, so I’ve failed again at something else I have tried’.
(transcript 9, p 5–6 lines 119–128).
3. Sense of self
I. Not good enough/inferior/failure-self-criticism
Participant 9, 16 and 28, each expressed a sense of self as ‘inferior’ or ‘not good enough’ in which they voiced concerns regarding not meeting expectations in some way and therefore they are held as a disappointment in the mind of others. There was an absence of global condemnation of self and more a focus on behaviours rather than personal attributes which signify ‘not meeting the mark’ i.e. how they ‘should be’ or what they ‘should be doing’.
For example: participant 9 uses the word ‘inferior’ to describe how she sees herself in relation to colleagues at work:
‘It makes me really upset because I feel as though I can’t do it. A massive aspect is sort of feeling of being found out or if they knew what I was doing. Something to uncover, so I suppose it makes me feel inferior to my colleagues when you experience those kinds of thoughts, physically I often find I suppose, like I am nervous now and I struggle for words’
(transcript 4, page 2, lines 31–36)
For example: participant 16 described his perceived inability to meet expectations due to his recurring depression:
‘I sometimes think to myself, well I used to be a Civil Engineer, that was my profession, I studied a long time to get there and there is no way I can go back there now. I just could not take the pressure basically and I think to myself, erm, I am a bit useless. I know I can’t do
anything about the fact I am always going to have this (depression) but I feel I am a bit like, I am not sort of fulfilling what I should be doing, could be doing and I should I suppose’
(transcript 7, p 4, lines 79–85)
And ‘I have always thought to myself I could probably do better…I have never been one that sort of comes to the forefront and I have always been a bit down on myself’
(transcript 7, p 11, lines 263–267)
Participant 9, expressed similar sentiments when discussing her experience of depression:
‘I do feel like it is something you suffer from…suffering is a funny thing to talk about in a sense that I know if I spoke to somebody else in that situation (experiencing depression) then I would see it as they are suffering. It is harder to accept it yourself …there are feelings, like you feel like I should be able to do something about it’
(transcript 4, page 6, lines 164–168).
Meanwhile, participant 28, reflecting on allowing time for herself observed:
‘I should be doing things, in my head, in my heart I don’t have to do other things, but in my head, it is, yes, you have got to do this, you have got to shampoo the carpet, you have got to
do the washing, you know, and normally this is me’
(transcript 4, p 11, lines 260–262).
alongside a sense ‘I don’t think I should enjoy things, not really enjoy things in life’ (because
they have not been earned).
(transcript 4, p 13, line, 294)
Participant 9 made reference to a fear of not meeting expectations in the eyes of God:
‘’when I was really low, I felt really really distant from God and I think it is something that I still feel like I am trying to work out. I don’t think, so, the fearfulness of God and the feelings like heart pounding are less now but some of the feelings connected to God, hasn’t come back…’(her voice trails off and she changes the subject quickly, as if it is a topic she does not
wish to delve too deeply in to).
(transcript 4, page, 9, Lines, 249–252).
Self-criticism was situation specific and always referred to the concept of not meeting expectations. This was reflected in their use of the terms ‘should’ and ‘could’, whereby the respondent identified a discrepancy between how they perceived they had performed in a certain context and how they perceived they should have performed i.e. the standards they perceive they ‘should’ or ‘could’ have met. The use of the term ‘should’ evoke a sense of obligation, duty or correctness. The term ‘could’ conveys the idea of degrees of possibility of what might be done or achieved and for participants 9, 16 and 28 there was a sense the fuel for self-criticism was a perception of having failed through some action of omission. There was a sense in their description of self-criticism of admonishing self, but without the contempt for self and personal debasement that came through in the transcripts of other participants.
Participant 28 described a strident commentary in her head with what she describes as ‘the nurse voice’ (transcript 5, p 7, line, 150) (she was a mental health nurse by profession). She defined this voice as:
‘it has a bit of authority about it in that it can guide you, but it can tell you off, make things very plain and quite stern….as necessary quite chatty and I try to talk to myself like that’.
(p 7 lines 162–167).
An example of the focus of this self-criticism spoken in ‘the nurse voice’ tone is as follows:
’well when I do things I do them wrong, so I will be vacuuming and I will have left the vacuum up and I will bang my led or, you know, oh no, I have got to plug it over there, instead of over there and so I criticise myself then’
(transcript 5, lines 223–226, p 10)
Similarly, participant 16 recognised he had always been ‘fairly self-critical’ and even though he was not depressed at the time of the interview recognised that he had a low tolerance for making mistakes and would criticise himself if he made an error. However, he laughed in a jocular way at the end of this statement conveying a sense that this aspect of self was perhaps forgivable:
‘Yeah its fairly low tolerance, I’m not a particular patient person and I am a bit of a perfectionist….(the interviewer enquires if he would criticise himself if he made a mistake)..most definitely, yeah, I still do that now feeling good, I still ‘oh you silly idiot or
something worse’
(transcript 7, p 12, lines, 285–293)
ii. unimportant/not counting/not worthy-self-blame
Participant 8, 12, 28 and 136 each expressed a sense of self as unimportant/not counting/not worthy, often accompanied by a perception ‘out of sight is out of mind’ i.e. due to their perceived status as unimportant and not worthy, they were not held at all in the mind of others. This was accompanied by a sense of being undeserving of care, praise, love or encouragement and therefore a lack of expectation that this would be forthcoming. There was a sense of the importance of ‘knowing your place’ and a fear non-compliance will result in intimidation, punishment or simply disregarded. A degree of subjugation was apparent in various guises. Subjugation in the cognitive therapy literature is defined as:
‘voluntarily meeting the needs of others at the expense of your own needs, submitting to others to avoid real or perceived consequences, or to surrendering control to others due to
real or perceived coercion’ (Young, 2003)
For example, participant 12, speaking about her father and how she perceived he viewed her:
‘brought up that I could never do anything totally properly….(transcript 8, p 2, lines 37-
47)….not feeling good enough (dad), part of start of depression (p 4, lines, 64–73)…..dad physically violent, lock me in cupboards….I was never good enough, this is where depression
started…(p 4, lines 74–91)…hated my sister she would be rebellious, do things to upset others and I got hit….(p 9, lines 210–221) …..message ‘not worthy’ (transcript 8, participant 12, p 10
line 222).
Whilst on face value this appeared an articulation of a sense of self as not good enough or inferior (as defined above) as the interview progressed participant 12 went on to voice a more subjugated position. She described how from her childhood it was decided for her by her father, that she would be ‘a carer’ something which, for her, conferred on her a lower status than her academically high achieving sister. This caring role was carried on throughout her life. She raised three children of her own, her grandson, cared for her mother in old age and a friend who was seriously ill. Indeed, she did not experience a depressive episode until the loss of her caring role occurred.
‘yes, I was to be a carer, that was decided for me as my mother was often ill and my father
did not want to know and so I was there to be a carer’
(transcript 8, page 4, lines 84–87)
Then later in the interview participant 12, discussing the personal impact of receiving a compliment stated how uncomfortable this used to feel prior to recovering from cancer and taking a decision to view herself differently. This example captures the self-blame (see below) and sense of being not worthy in some way:
‘you are not worthy of compliments, but now, better you know…. You want to hide.
Everybody, everything, everybody is looking at you. I know now they are not, but that is how you actually feel. They know that you are a dreadful, awful person and something you have
done wrong.’
(transcript 8, page 9, lines 205–221)
Self-blame marked the dialogues of participants 8, 12 and 136 which seemed subjectively, more insidious in its manifestation than the self-criticism described above, taking on a deferential or punitive tone. Blame confers a sense that an individual did something wrong or is responsible for something bad happening.
For example, participant 12, whose childhood was characterised by a very violent and blaming father, reflected on how she viewed herself when she first developed depression and contrasted this with how she felt in the here and now having undergone treatment for cancer: ‘it was all my fault. I had hurt everybody and not the other way round. Everything was my fault, not being a good enough human being to look after everybody else (the interviewer asked if she still feels this way now her depression has remitted) I still have it, but no way near as I did, for me to be able to finally, make a decision at 64, it is not all my fault
anymore’
(transcript 8, page 5, lines 102–115).
Here there is a sense in which the finger of blame has been turned upon self and this is imbued with a mocking, stance towards self. For example, Participant 8, when the interviewer asked if he recognised that he was chastising himself, what its purpose might be and was it deserved he stated (his voice tone was impatient and dismissive of self):
‘I know I am doing it, I am punishing myself, should have done that you idiot, why have you done that? Why did you get yourself into this situation?...there is no purpose I would say. So, it is just an outlet to let the steam go. Nobody is there at the time…. when I’m driving the taxi…. not got to the right house and I think ‘what are you doing?...’. (transcript 6, p21-22,
lines 470–479).
Similarly, participant 12 described how when she first became depressed, she did not view this as an illness but rather as ‘it’s you’. The interviewer reflected this statement back to her and she observed:
‘oh yes, definitely. You are not nice enough to people. Don’t stand and talk to anybody in case you say the wrong thing. You are not good enough to be in their company. ‘Oh dear, am I intelligent enough?’
(transcript 8, pages 6–7, lines 147–152).
For this subgroup of the cohort praise was an aversive experience and is met with incomprehension or elicited tearfulness as it is experienced as undeserved. This is illustrated in the following example from participant 12 who observed that several people had praised her for raising ‘three intelligent, caring daughters’. As she spoke, she became tearful. The interviewer enquired as to what it was about receiving praise that made her tearful. She replied:
‘at the time very uncomfortable, you are not worthy of compliments…you want to hide. Everybody, everything, everybody is looking at you, they know…that you are a dreadful, awful person and you have done something wrong’
(transcript 8, page 9, lines 205–221).
Meanwhile, Participant 28, described herself thus:
‘I am not a worthy person’
(transcript 5, page 14, line 315)
and observed:
‘I never felt and never thought I was worthy of friendship’
(transcript 5, page 4, lines 81–82).
As well as articulating feelings of shame linked to this sense of self as not worthy:
‘I want to cry deep down inside me and it is like a little ball of shame and it is a feeling that starts inside me and then it sort of grows and I recognise what it is and then you know I always sort of put myself at the back and try not to engage with people because they are not
going to like me and don’t want to be with me’ (transcript 5, page 3, lies 62–65).
Similarly, Participant 8, made reference to ‘self-chastising’ (a form of self-criticism) and early in his interview described the following when attending a support group at a local community mental health team:
‘there was a couple of us and we had got this self-chastising to a fine art. You know, we could not take a compliment, not a chance. I could not give a compliment to somebody
either, but I think yeah, I have got that (self-chastising) to a fine art’
(transcript 6, page 12, lines 256–259).
He observed not only difficulty with accepting compliments but also giving them.
Participant 8 continued:
‘I am used to people taking the piss out of me and I taking the piss out of them, so handling a
compliment is just something I can’t do very well at all’
(transcript 6, page 14, lines 322–323)
‘Taking the piss’ is a British idiomatic term which can be defined as ‘mocking someone or something’ (Ayto, 2009). The use of this by participant 8 seemed to mark not only how he interacted with others but his own internal commentary with himself (see the example above from participant 8 in the quote where he describes punishing himself (transcript 6, p21-22, lines 470–479). Mocking is a facet of shaming behaviour. This ‘taking the piss’ and inability to take or give a compliment is an example of the internalisation of how participant 8 experienced interacting with his own father (see example the example of telling his father he can count to ten in French), although he did not recognise this in the moment in the interview.
Participant 136, speaking about his experience of depression and anxiety and his tendency to avoid or leave situations is predicated upon his sense he would ‘need to explain himself’. He does not hold a sense he has a right not to explain if he wishes not to do so (i.e. a subjugated position):
‘‘I feel once it was over I would feel as though I would need to explain and I don’t like to do that..you have to go in to what happened to you, your depression..I just feel it is not something I always want to go in to…it is difficult…it is in my nature as well to keep things to
myself’
(transcript 3, pages 11–12, lines 240- 262).
Participant 136 also spoke about experiencing panic attacks whilst out of the house and a sense of others not only judging him but ignoring him too:
‘having a panic attack, you sit down in town because you can’t stand and people look at you gone out. I don’t know if they think that you are drunk or what…its hard (the interviewer asked him what is hard about this experience and he stated) being ignored…(people think)
that you are on drugs’
(transcript 3, page 6–7, lines 203–216)
Throughout the interview with participant 136 there was a sense of insignificance in his interaction. His eyes were downcast and his voice tone quiet and hesitant and his manner passive with an air of resignation and defeat. This participant used the phrase ‘gone out’ to express how he perceived others judged him. This is a colloquialism which has a variety of interpretations from appearing to lack intelligence to displaying signs of madness. He also describes being ‘ignored’ (‘refuse to take notice of or acknowledge; disregard intentionally’ (Cambridge online dictionary, 2020)) which possibly indicates a sense of insignificance and worthlessness.
iii. Bad/inadequate/insignificant/worthless: self-hate/loathing
Participants 11, 15, 20 and 88 each expressed a sense of self held as bad inadequate, insignificant or worthless and anticipated ridicule, humiliation, punishment and ostracism from others. Their dialogue, language, voice tone and behaviour in the interview expressed varying degrees of self-hate and/or self-loathing with a visceral tone. This appeared more closely aligned to a global condemnation of self which operated across time (i.e. from childhood to the present day) and situations.
Participant 88, (who disclosed sexual abuse) articulated her sense of self -hate/loathing as follows:
‘I am a bad, horrible person, just useless, that is what I suppose I mean, useless, just not nice….I feel bad about the way, I just feel, I don’t like the way I look, I just feel bad about
that. I just feel I am a waste of space that I’m not worthy to be in people’s company or they
should not be around me. They should not be near me because I am horrible, waste of time
person that’s just not worth anything’
(transcript 1, p10, lines 248–251)
The interviewer observed participant 88 use the phrase ‘loathe myself’ and asked for clarification. She continued:
‘Oh God and the feeling is pure, it is pure loathing myself…it’s just loathing when you really don’t want that person near you, yet that person is you and you want to rip it off and take it off and that is why I numb myself, I don’t know how I do, I just do and it goes away’ (transcript 1, p 11, lines 262–267)
She continued:
‘I literally cringe and my body and you know like you know when you cringe it tingles, it’s like, ugh, God, get it away, its repulsive, its near me but it’s me that’s near me and its making me feel it now actually make it go away, yeah its, yeah talking about it is bringing it’
(transcript 1, p 11, lines 270–273)
This description of self was accompanied by paralanguage and facial expressions imbued with a visceral sense of self-hate and self-disgust which she experienced in the moment of describing it. For example, she voiced ‘ugh’ (a manifestation of a strong feeling of disgust) and used the word ‘Cringe’ (to suddenly move away from someone or something because you are repulsed) and this was accompanied by the universally recognised facial expression for disgust (Tracy and Robins 2007a). Further, Participant 88, articulated this sense of selfhate and self-loathing using the following labels to describe herself: ‘an oaf’: (a stupid, rude or awkward person), ‘a Freak’ (someone who looks strange or behaves in a strange way, not normal), ‘vile’ (unpleasant, immoral, unacceptable) and ‘repulsive’ (extremely unpleasant or unacceptable). In this paragraph, the bracketed definitions of the words participant 88 used are taken from the Cambridge online Dictionary (2020).
Participant 20 disclosed that he had a severe stammer as a child, which had remained with him and which worsened if he became tired or stressed. He recounted experiences at school of being shamed and humiliated by both adults and his peers. These were recounted in a factual way. Whilst speaking, his voice was loaded with anger and contempt directed at both his persecutors and himself. Throughout the interview he referred to the stammer in several contexts i.e. ‘it is my nightmare’ (transcript 2, p 6, line 40) and as something that has always marked him as not part of the in-group i.e. (since being small) ‘felt I am different’ (transcript 2, p 12, line 298) and ‘not being able to do something that others could do (speak in public), looking stupid, looking different, fear, anxiety’ (transcript 2, p7 line 1690. He shared the following:
(at primary school) ‘consider this is the early 1960’s when people were less PC (politically correct), I can distinctly remember the entire class laughing at me and the teacher
laughing…..it just makes me clam up. Things got worse when I went to senior school because people, not people I was friends with, but there is always a group of kids at school and they decided it was hilarious to volunteer me to read out in class and things like that which was quite upsetting as you can imagine’ . He links this to the present day when the interviewer observes ‘it sounds like all that is still with you today? And he states: ‘yeah, yeah, a fool’ (transcript 20, p6, lines 142–154).
Participant 20 spoke of himself in disparaging terms, inherent to which was a lack of respect for self and an anticipation of ridicule and humiliation from others. This was articulated in a variety of ways throughout the interview. He used terms such as ‘fool’ and described ‘being made a fool of’ inferring another is trying to make him look stupid in some way and ‘clam up’ which can be defined as a person suddenly becoming silent due to embarrassment.
For example, he voiced a sense of inadequacy whilst recollecting emotional memories from childhood and stammering:
‘not being able to do something that others could do, looking stupid, looking different, fear,
anxiety’
(transcript 2, page 7, lines 170–171).
And later speaking about his experience of depression:
‘it just tells you what I already knew, I am not like everyone else, I can’t do things that everyone else finds natural and normal (with reference to his stammer)’
(transcript 2, page 11, lines 254–255).
Participant 20 continued:
‘I suppose at the middle of it all is I don’t really like myself so my understanding is I don’t know why other people would, I just don’t think I am very good’
(transcript 2, page 11, lines 266–268).
And participant 20 again:
‘well I know it sounds crazy and I know it’s not happening, but I can’t change the feeling that people are looking at me, talking about me, don’t approve’
(transcript 2, page 5, lines 104–105).
Towards the end of the interview participant 20 gave the following definition of self in which he describes himself as having what he sees as characterological flaws:
‘I think in the sense that I do feel ashamed because I am weak, because I have been a failure. I mean I was a failure as a husband, obviously, I think I have probably been a failure as a parent, whether my kids would disagree with that’
(transcript 2, page 14, lines 345–347)
Participant 15 described a sense of inadequacy in the context of the physical limitations he experienced due to his heart condition and the fact he had not worked for the past twentyfour years and in his words ‘provided for his family’, which within the community in which he was raised is considered shameful:
‘’do I feel as if I have had a full life? No. Do I feel I’ve had a lovely life? In a way yes, because I have got me wife and I have got me grandchildren. I have not achieved the things I would
have liked to have achieved. Probably I would have loved to have been able to buy my own
house. Because I can’t work, I can’t buy a house, the only way I would do that if I won the
lottery’
(transcript 9, pages 11–12, liens 267–271)
He continues a few minutes later:
‘you don’t feel as if you are being a man. I haven’t been a person. You look around at what
other people have done and even younger people than yourself and you see them with cars, you see them going out socialising and they have got their own houses, I don’t begrudge it, they have worked for it to get it, what they have got, I just wish I could (that is work).
(transcript 9, page 12, lines 285–289).
Participant 11 gave the following reasons for her self-hate:
‘I don’t like what I have become physically or mentally, I don’t like the person I am….I don’t feel I have made myself this way, I think it is genetic or mental, chemical defect in my brain. I am aware that it isn’t just natural self-loathing or self-inflicted. I don’t feel it’s that, but my frustration makes me hate myself, what I am, you know I used to be warm and happy and easy, I am not that person I was, I do not recognise myself anymore as the person I used to be’
(transcript 10, pages 3–5, lines 48–78)
There was a great deal of seeming contradiction throughout the interview with participant 11. In the extract above she states she does not blame herself for her depression but hates herself because of the impact it has had on her ability to function and how this has impacted on her personhood. However, she used the word ‘defect’ to account for her depression, which can be defined as something lacking in someone (Cambridge, 2020).
Participant 15 seemed filled with shame throughout the interview. His voice tone was often contemptuous of self and he frequently expressed anger at himself for what he perceived as inherent ‘weakness’ (a fault in someone’s character (Cambridge, 2020)), which can be seen as a marker for a sense of self as inadequate. For example:
‘I am not a man, I haven’t felt like a man for a long time, I feel a total failure’
(transcript 9, p 2, line 38)
The following excerpt from the interview with participant 15, who had a serious heart condition illustrates his fear of appearing inadequate. In the context of the long-standing uncertainty regarding his physical health (20 years) the interviewer observed he had perhaps shown courage. His response below, which towards the end becomes slightly garbled (the possible theoretical significance of this is explored in the discussion chapter of this thesis) is an apt illustration of the interplay between shame and pride:
‘I haven’t got no courage. No, it frightens me, but you put it like that, it’s like when I had my two heart attacks in two days, I just refused to hit the ground. Everything went dead on my
left side. I actually had me paper in me hand and I picked my arm up and put it in me pocket.
I got home because I did not have the, I had the sense of, if you asked yourself I had the sense to go down but the pride would not let me, until I walked through the door and I fell
and hit this face’
(transcript 9, p 19, lines 364–369)
Name calling was cited by participant 8 and 136. These are detailed below. The definitions cited are taken from the Cambridge Online Dictionary (2020).
Participant 8: described speaking to himself in an angry tone. The interviewer observed he was becoming animated and expressing anger at other people’s behaviour and asks: ‘do you ever get angry at yourself?’ He states:
‘yeah, all the time. I am angry permanently at myself, when I’m chastising myself, ‘you idiot,
why?’
(transcript 8, page 11, lines 251–252)
Participant 136, at two different points in the interview, referred to himself as ‘an idiot’ in the context of potentially needing help when his mood is depressed and anxious. His voice tone whilst using the word was clipped and dismissive of himself and he was looking at the floor.
‘It is in my nature to keep things to myself… I find it difficult (needing help), I have got to deal with it myself (the interviewer asks if it say anything about him needing help) yeah, an
idiot’
(transcript 3, page 12, lines 262–278)
Further, whilst talking about having a panic attack in public and his fear of others judging him, the interviewer asks how he dealt with this and how he feels:
‘Usually just walk away…I just feel an idiot’
(transcript 3, p 7, lines 237–239)
3. The function of self-criticism/self-hating
Participants 8, 9, 20 and 28 expressed the idea that self-criticism served a positive function.
For participant 9 self-criticism served the purpose of helping her to maintain high standards:
‘’If I criticise myself there is a reason that I’m doing it and so it is not just for the sake of it…..(she illustrates her point with an example) so if a parent has called me at work I feel bad if I don’t get in touch with them and perhaps I will feel I have not done my job well because the parent has not had a return call and that’s bad…. I don’t naturally think, well I have not called them back because I have been doing x,y and z….I don’t suddenly want to say to myself, ‘oh, you are okay at your job’ for the sake of it…..I do think I see it (self-criticism) as
useful in that sense’
(transcript 4, page 9–10, lines 259–274)
Whilst participant 28 expressed the idea that self-criticism drove her to work to meet high standards and achieve. Thus, it protected her from others looking down on her and judging her. She went on to describe her fears about what might happen if she did not criticise herself:
‘I would expose myself to others and my emotions to other people and that they would look
down on me or they think that I failed and I am not a worthy person’
(transcript 5, p 14, lines 312–315)
Participant 8 expressed the view that self-criticism was harmless and indeed perhaps served a purpose in preventing him making the same mistake twice:
I don’t think it does you any harm…to deserve or not deserve it, you know, well actually everybody must do that don’t they? ……. yes, I am critical of everything…it makes me think,
well, I won’t do the same mistake twice’
(transcript 6, p21-22, lines 480–492).
Participant 20 observed the importance of his self-hating stance as not only a guard against self-indulgence but a protection against others finding out your true nature. The word indulgence can be defined as allowing someone to have or do whatever they want, with the implication this is not good for you.
‘I think up to a point everybody has got to be a little bit critical of themselves otherwise you
just become self-indulgent….’
(transcript 2, lines 235–236, p 13).
As he was speaking his eyes were downcast and his voice trailed off. When the interviewer asked for clarification, he made an oblique reference to his childhood and then he stated:
‘it is difficult, I just thought I had got a handle on it, but it has gone again…..it (self-hating) makes it easier for me to be a bit of a loner and not have to deal with other people too much because if I deal with other people too much, they are going to find out that I am not a good person’
(transcript 2, page 14, lines 336–339).
4. Absence of self-compassion
None of the ten participants had a sense of self-compassion.
i. Intellectual appreciation with good intentions
Participants 28 and 88 had been exposed to the concept of compassion and self-compassion through therapy and self-help books. As a consequence, they were able to define it, endorsed it as a good idea and attempt to use it but struggled to emotionally engage with its practices.
For example, participant 28 describes how self-compassion feels and is unable to observe her own self-criticism of her perceived inadequate attempts to use it:
‘they are quite calming feelings, they are sort of nice, floaty feelings, but they don’t sort of spread out very far…sort of encased good feelings and I try to do a good thing but at the moment I am really failing…. something that I would like that would help me..something
that links in with those nice thoughts and make them bigger hopefully’
(transcript 4, lines 232–240, p 10)
Early in the interview participant 88, when speaking about her approach to herself when depressed, her immediate response was, spoken in a shrill, impatient voice tone: ‘oh, it’s like for God’s sake pull yourself together’ (transcript 1, p 2, line 45). Mid-sentence she then corrected herself:
‘well actually no, you don’t have to pull yourself together-look I am better to myself-being self-compassionate because I used to call myself a lot….oh God I have been my own worst
enemy for years and years and probably the last couple of years I have been reading a few
books and I have started to say nice things to myself and actually if you are depressed it is
not a problem, don’t fight, go with it and wait for it to go’
(transcript 1, p 2–3 line 45–52)
Participant 88 is the only participant who spoke towards herself in vivo in the interview in a warm and gentle voice tone. This was in the context of describing some of her self-soothing strategies aimed at tackling here intense sense of self-loathing. She observed:
‘Yeah, having a cup of tea is my thing and if somebody makes me a cup of tea it makes me feel really nice. I have got this thing about people making me tea, it is such a homely, lovely
thing. And the dogs and just allowing myself to sit down and be-if I can do that, that’s; nice, in silence and just be and just say (speaking in a soft, warm voice tone) ‘look it’s all fine’. I can learn now to say, ‘right I am here and now look its over’ and that actually does work.
You have to keep it going though and once the thoughts come you have got to keep saying it. I can do that until I am feeling a little better now and the dogs, my dogs have always been there for me and they are a big help….they just love you don’t they, unconditionally, they are
just there for you, not nasty to you’
(transcript 1, p 12, lines 289–298)
During the interview with Participant 16 he was talking about showing kindness to others when they are experiencing an episode of depression and the interviewer asked for his view on compassion he replied:
‘oh lord, to be honest I have never used the word, I have never really, I don’t completely understand what it means’
(transcript 7, page 15–16, lines 365–368)
As participant 16 reflected further, once the interviewer had given a definition of selfcompassion:
‘right, oh yeah, so I think, I like to think, that I can have empathy for other people but it is hard to have..how do you have empathy for yourself when you are?..(the interviewer asks what gets in the way of empathy for self) my negative thoughts, I suppose, those hating
myself thoughts…I imagine….(the interviewer asks how the idea of being compassionate towards himself sits) ‘in theory quite well, how I would go about it I am not sure…just getting past this sense of negativeness for oneself perhaps if I could sort of get passed that
then
perhaps I could be a little more compassionate towards myself…..I suppose it is just that selfhating thing, that I am completely useless and a complete waste of space type of thing
and if I could sort of get that into my head, that I am not a complete waste of space, even though at the time, I know I am not…it’s just hard to make myself believe it I suppose’
(transcript 7, pages 380–406)
ii. Not understood/incomprehension
Participants 8, 12, 16 and 136 struggled to comprehend the concept of self-compassion when this was raised by the interviewer.
Participant 12, when asked to consider the idea of taking a compassionate stance towards her own suffering stated:
‘Not something I think about’
(transcript 8, line 257, p 15)
During the interview with participant 136 the interviewer asked if he ever considered being kinder to himself when he was struggling with his mood and panic attacks. His response is indicative of a lack of understanding of the possibility of self-compassion. On the first occasion (discussing his depressed mood) he gave a monosyllabic reply ‘no’ (transcript 3, line 167, p 5) and laughed in a way that suggested this was an incomprehensible idea. On a further occasion (discussing his panic attacks whilst out of the house) the interviewer asked the same question and he gave another monosyllabic reply. He then fell silent looking puzzled and confused:
‘no, not really….(after a few moments silence the interviewer asked a leading question ‘does it seem a bit of a bizarre idea to be kind to yourself?) he replied: ‘Yeah it does…(he then went on to describe: ‘you just try and do nothing or think of anything…you just try to get through it…..pull myself together’
(transcript 3, lines 180–195, p 6)
Similarly, participant 8, when the idea of self-compassion was raised in the context of depression replied:
‘that (self-compassion) is a sort of panacea of…how do you do that? How could you be compassionate to yourself when you are not trained to be compassionate? (his voice tone is slightly scathing and the interviewer clarifies the concept by asking him to consider the idea of being more compassionate to himself) he continues: ‘I am trying to be compassionate to myself now and thinking about how I feel…I am saying yes you did well John (not his actual name) and it kind of does lift you a little bit. Again, it is short term, I have not been depressed that long, I don’t know I am depressed anymore, I know what you are saying and it does sound good doesn’t it?’
(transcript, 6, p 23–24, lines 533–542)
iii. Risky
Participants 11, 12 and 20 each viewed self-compassion as carrying some form of risk.
Participant 11 uses the word compassion very early in the interview to describe how her son is towards her. The interviewer asked her if she ever tried to show compassion towards herself. Her response:
‘No because I don’t like the person I am, so I am not compassionate towards myself’
(transcript, 10, p 3, lines 50–51)
Later she likens self-compassion to self-pity:
‘because if I start to feel sorry for myself, I start becoming overly compassionate (towards self) I won’t get out of bed because I would give in to how I feel. Particularly mentally you know. Like I say mornings are bad mentally and in turn they are bad physically..and if I was kind or compassionate to myself I would think, ‘I’m not going to get dressed today….I have to be hard on myself, I have to tell myself ‘right, snap out of it, get up, get showered, get dressed and that is why I have to be firm or hard with myself…quite abrupt’
(transcript 10, p 7–9, lines 137–159)
The voice tone of participant 11 towards herself at this juncture is harsh, cold and scolding. The interviewer enquired as to what would happen if she adopted a gentler voice tone towards self, she replied:
‘I would leave it an hour or two longer if it was gentler, I would think, alright then in a bit and before you knew it the day would be gone, because the day goes anyway, it takes me a long while to get moving (the interviewer asks if there are any situations where a gentle
stance towards self would be allowed) ‘no, really, no’
(transcript 10, p 9–10, lines 166–179)
Participant 12, describes self-compassion as:
‘that you are blowing your own trumpet, you know, if you told yourself you were good’
(transcript 8, line 366, p 15)
This analogy with the idiom ‘blowing your own trumpet’ which is defined by Ayto (2009) as: ‘to talk openly and boastfully about your achievements’ (P 364) infers a sense of risk in being compassionate to self and in the citation from participant 12 giving yourself credit for her hard work helping others. Reflection on what the participant means by this statement invokes another idiom ‘pride comes before a fall’ which conveys the idea that if you are too full of conceit or self-importance something will happen which will lead you to look foolish (Ayto, 2009, p 274). This is an illustration of the interplay between pride and shame.
Participant 20 also had a sense self-compassion might be potentially risky, whilst also admonishing himself:
‘well I know it is going to sound daft, but it might be difficult to know where to draw the line’ (transcript, 2, line 322, p13)
iv. Not deserved
Participants 15 and 20 expressed a view that they were undeserving of self-compassion due to the characterological flaws they observed in themselves.
Participant 20:
‘If I were hearing this from another person, I would probably think they were worth compassion, but I don’t like myself, I don’t think I deserve it’
(transcript 2, p 12, line 285–287)
Participant 15 was strident in stating the reason he was not allowed self-compassion:
‘no because I am not happy with the way I am. I have not been happy with the way I am for
a long time……I think it is too late, I am in this dark place and bad place’
(transcript, 9, p 13 lines 307–308 and page 16, line 374)
5. Avoidant coping
Four participants (15, 20, 8, 136) all engaged in cognitive, emotional and behavioural avoidance as a means of coping.
For example, participant 15, despite serious health issues smoked and drank 1–2 litres of whisky a week as a means of managing his mood and his self-hating internal dialogue. Thus, he observed:
‘my life it’s like living on a knife edge. I could go one way or the other (referring to taking his own life) as the way I am now, it’s comfortable and I still have the questions every night when I can’t sleep and that’s where the whisky came in because I could not sleep and I
wanted to sleep….I never knew when enough was enough, I just drunk more and more……I
would drink from eleven o’clock in the morning to eleven o’clock in the evening (this would
be his preference but he curtails this for the sake of his family) as the only time I feel at peace and I’m not arguing with myself , I am at that floating zone, I haven’t got this happening, I haven’t got that happening’
(transcript 9, page 22, lines 440–453)
In addition, he avoids acknowledging the contribution his smoking and alcohol consumption makes to his physical and mental health problems:
‘I ask myself that question a lot, have I done things that hurt, I should not have done, made
myself worse, I don’t know, I honestly don’t know’ (transcript 9, page 7, lines 165–168)
And:
‘I came off smoking for seven years, did feel better for it at times but it was then I had the two heart attacks in two days and when I got out of hospital I needed something in my hand so I started smoking and I have been smoking ever since’
(transcript 9, page 7, lines 173–176)
Participant 8 also articulated avoidant coping in the form of alcohol consumption and working long hours:
‘as of yesterday, I stopped drinking alcohol. But for three years before that I got drunk every night, in bed, alone and I just worked and went to bed and that was it really and I ate in bed.
I always took the dog a walk, I just felt I had been let down by everything in life’ (transcript 6, page 1, lines 5–10)
Participant 28 describes engaging in cognitive and emotional avoidance both in terms of trying to deal with a perceived failure and in trying to deal with negative thoughts as follows:
‘I just don’t want to think about whatever I have failed at and my feelings are sort of irrelevant and I just kind of shut down and forget about it, cutting off and its always an embarrassment now, and I think about it for ages, but now I block that out (self-critical thoughts)’
(transcript 5, p15, lines 326–331)
Similarly, participant 136 described how he deals with panic attacks:
‘you just try and do nothing or think of anything…. you just try and get through it…. I think
‘pull myself together’ (transcript 3, p 6, lines 185–195)
Similarly, if his mood is depressed, he would cope by:
‘well usually if it is quite bad I usually just sit there for a few days or more….I’ve been through it before, so I think once it passes….I know it is meant to go away…and I try to watch TV, which does not last long, it is usually the radio’
(transcript 3, p 5, lines 140–161)
Participant 88 gives a vivid description of avoidant coping which is consonant with clinical definitions of dissociation:
‘I have learnt somehow, I don’t know how, I have to learn to switch off. Many years ago, I had to learn to switch off and like I can kill myself and make myself die inside and you can
just go around like a zombie, like a robot. I have done that a lot as well’
(transcript 1, p 3–4, lines 71–74)
7. Memory and information processing biases in depression
All ten participants spontaneously reported the memory biases cited in the cognitive science of depression literature (Harvey, Watkins, Mansell, and Shafran, 2004; Williams, Watts, MacLeod and Mathews, 1997). These include negativity of thought content (Disner, Shumake and Beevers, 2017; Gotlib, Krasnoperova, Yue, and Joormann, 2004; Beevers and Carver,
2003; Bradley, Mogg, and Lee, 1997; Beck, Brown, Steer, Eidelson and Riskind, 1987; Beck, 1967), autobiographical memory (Williams, Barnhofer, Crane, Herman, Raes, Watkins and
Dalgleish, 2007) and intrusive autobiographical depressive memories (Mihailova and Jobson, 2018), rumination (Watkins and Teasdale, 2001) and dichotomous information processing (Teasdale, Moore, Hayhurst, Pope, Williams, and Segal 2002).
For example, Participant 16, responded to the first question in the interview (‘can you tell me how depression affects you on a day to day basis?) with the response: ‘right, which is difficult as I am completely not depressed at the minute’ (transcript 7 p 1, line 3). He then proceeded to speak with clarity about the difference between his sense of self and his approach to life when his mood is depressed versus when his mood is not depressed, ‘a hell of a lot different’
(transcript 7, p 1 line 16). He recognised that when his mood was depressed, he experienced intense and at times extreme, self-hating negative thoughts about himself, which in the interview he stated he does not believe when his mood is not depressed. Examples of this negativity of thought content when mood is depressed (see Disner, Shumake, and Beevers, 2017) he shared in the interview:
‘Well I completely hate myself…I think what is the point of being me, being alive and I have been quite suicidal on several occasions to be honest….. I hate being alive, hate the way I think, hate the things that I do or don’t do, depending on what its is’ (transcript 7, p 2 lines 42–46) ‘self-loathing kicks in, don’t allow myself nice things’
(transcript 7, p 7 162–171) ‘self-criticism becomes ruminative’
(transcript 7, p12, lines 294–308) ‘If I’m sort of in between and I’m not really very low, then I can sort of try a little bit, you know try and talk myself out of these negative thoughts’
(transcript 7, p 3 lines 67–68)
Similarly, participant 88 recognised that when her mood was depressed she experienced not only an increase in the frequency of self-critical thoughts but also their intensity changed, taking on a tenor of self-loathing (transcript 1, p 7, lines 164–175) and that her sense of self as ‘vile’ and ‘ugly’ intensified as her mood deteriorated. She vividly described how, when her mood was very depressed, she was ‘haunted by the memories’ of the sexual and physical abuse perpetrated against her as a child, (transcript 1, pp 24–25 lines 611–618). This is an example of intrusive depressive autobiographical memories emerging as level of depression increases (see Mihailova and Jobson, 2018). She contrasted this later in the interview reflecting that on a ‘good day’ i.e. when mood is less depressed ‘I think, oh you are really good’ (p 28, line 700–707). These two contrasting positions exemplifies the dichotomous information processing that characterises the depressive state and which Teasdale and colleagues argue is predictive of a vulnerability to depressive relapse (see Teasdale, Moore, Hayhurst, et al 2002).
Participant 15 gave a classic account of his experience of autobiographical memory recall and depressive rumination (see Williams, Barnhofer, Crane, et al 2007; Watkins and Teasdale, 2001):
‘you lie in bed on a night and you can’t sleep and you see it like it is living it again, what would I be like if I hadn’t done this and I hadn’t done that or I wasn’t this way or that….the
same questions go round and round again’
(participant 15, p 11, lines 245–2448)
Participant 28, recognised that her sense of shame intensifies when her mood is more depressed:
‘I think shame was kind of there as a child……and it is actually when I’m depressed it sort of makes it worse…..(the shame)….it sort of comes out more….I just wallow in it….when it is bad (depression) I just wallow in it (shame)’
(transcript 5, pages 4- 5, lines 95–106)
Participant 136 recognised an increase in the intensity of his feelings of anger towards depression as his mood worsens:
‘’well it is usually when I am quite bad then, that is when I get angry with it (interviewer asks what he says to it and he replies) you do not want to know (he laughs, implying he swears at it), it’s all in your head, wanting it to go away and everything’
(transcript 3, page 4, lines 128–134)
Several participants (16, 28, 88) also recognised that the frequency, intensity and duration of self-criticism reflected the intensity of their depressed mood and for some, but not all, that self-criticism moved to self-hating and self-loathing as depressed mood intensified. This observation is discussed more fully in the discussion chapter of this thesis.
Summary
The overall aim in this qualitative arm of the study was to address the question ‘How do participants diagnosed with persistent, treatment resistant depression experience shame, self-criticism and self-compassion?’ in the context of Gilbert’s formulation of the role of shame, self-criticism and self-compassion, in a cohort of patients diagnosed with persistent, treatment resistant depression. This question will be addressed more comprehensively in the discussion chapter of this thesis. However, to summarise, the data from this group of participants, whilst generating evidence to support some of Gilbert’s theory it also identifies some aspects of the experience of depression that Gilbert’s model does not consider. In interpreting the data through the lens of cognition what has emerged from the themes and sub-themes is a continuum of shame experiences from sense of self as not good enough/inferior/failure associated with self-criticism),through unimportant/not counting/not worthy worthless, associated with self-blame, to sense of self as bad/inadequate/insignificant/worthless, associated with self-hate and self-loathing. Whilst each of these constructs and their relationship to shame are articulated in Gilbert’s model (i.e. Gilbert and Irons, 2005), these are formulated in the context of an evolutionary definition of shame, without reference to attributional models of shame and depression (Abramson, Seligman and Teasdale, 1978; Abramson and Sackheim, 1977). The data presented in this chapter provides evidence for the manifestation of varying degrees of shame in persistent, treatment resistant depression, which also seem to parallel the childhood experiences and environments described by the participants. The impact of childhood environment on the emergence of shame, self-criticism and self-compassion is at the heart of Gilbert’s model of shame (Gilbert, 2007a; Gilbert, Cheung, Grandfield, Campey and Irons, 2003).
In addition, in terms of clinical interventions for targeting self-criticism Gilbert’s model does address the function of self-criticism (Gilbert and Irons, 2005) and this is something that emerged from the qualitative data in this study. Similarly, Gilbert discusses in his clinical interventions the concepts of fear of self-compassion and avoidant coping (Kirby and Gilbert, 2017) Themes relevant to the concept of fear of self-compassion were identified within the cohort studied here. Three descriptors emerged; the incomprehension of self-compassion, self-compassion as risky and self-compassion as not deserved. Avoidant coping also emerged as a theme both spoken by the participants and observed by the interviewer. Avoidant coping is a central tenant of Gilbert’s model discussed in the context of safety strategies (Gilbert, 2017a; 2016; Gilbert, 2010a; Gilbert, 2001).
A theme that emerged from this data set and which is well documented in the cognitive science literature and which is not referred to in any of Gilbert’s work are the memory and information processing biases in depression (Garland, 2016; Harvey, Watkins, Mansell and Shafran, 2004). These have a significant impact in terms of the subjective experience of depression and implications for treatment. In the author’s own clinical experience of using compassion focused CBT as a group intervention, these memory and information processing biases unless targeted exert a significant, detrimental impact on attempts to engage with the principles and practices of self-compassion. These emergent themes and their theoretical and clinical implications will be discussed more fully in the final chapter of this thesis where the quantitative and qualitative results will be synthesised within the convergent parallel mixed methods design described in the methods chapter of this thesis.
Chapter 6 Discussion
Introduction
The chapter begins with a summary of the findings of this PhD study in relation to each of the research objectives. This is followed by an integration of the quantitative and qualitative data collected to summarise the reliability and validity of each of the measures tested (OAS, FSCSR and SCS). These results are discussed in the context of other studies which have tested the psychometric properties of these measures. This is followed by a summary of the results from this PhD thesis examined through the lens of Gilberts model of shame (Gilbert, 2007a) in a cohort of patients diagnosed with persistent, treatment resistant depression. This includes discussion of the limitations of Gilberts theory in relation to the cohort studied, with reference to other research in the field of depression, notably attributional theory (Bernstein, Evan, Van Bork, Moriarty, Giollabhui, Abramson and Alloy, (2019) and the cognitive science of depression (Harvey, Watkins, Mansell, and Shafran, 2004) and recent research in shame and autobiographical memory (Matos, Pinto-Gouveia and Duarte, 2012; Matos and PintoGouveia, 2010). Based on this critique a model is proposed for conceptualising shame, selfcriticism and absence of self-compassion in persistent, treatment resistant depression integrating Gilbert’s psychobiosocial evolutionary formulation of shame with attributional theory, taking into consideration the clinical features of autobiographical memory, rumination and thought suppression that characterise depression. From this, suggestions will be made as to how psychological treatments might better target shame, self-criticism and absence of self-compassion in patients diagnosed with persistent, treatment resistant depression, with recommendations for further areas of research. Finally, the strengths and limitations of this PhD study are discussed and overall conclusions presented.
Summary of Findings
In this study the psychometric properties of the OAS, FSCSR and SCS were tested on a cohort of participants diagnosed with persistent, treatment resistant depression. The OAS and FSCSR were found to be reliable and valid measures in this population with CFA supporting the three factor model for each measure (see OAS: Goss, Gilbert and Allan, 1994; Allan, Gilbert and Goss, 1994; FSCSR: Gilbert, Clarke, Hempel, Miles and Irons, 2004). These findings, when integrated with aspects of the qualitative data support the theoretical formulation of shame and self-criticism which underpin the OAS and FSCSR as tested on this cohort of participants. However, regarding the OAS the construct emptiness did not perform as well as the inferior and mistakes sub-scales. A possible explanation for this finding in this cohort and a suggested revision of the OAS for use with this population is discussed below. The qualitative data also reveals findings that highlight aspects of the lived experience of depression, supported by the cognitive science of depression that Gilbert’s formulation does not consider. These issues are discussed more fully later in this chapter.
Meanwhile the SCS, whilst demonstrating reliability, did not prove to be a valid measure in the population under investigation. The SCS showed poor discriminant validity which is indicative of multicollinearity. This finding raises the question of multidimensionality in the development and validation of psychometric measures (Reise, Bonifay and Haviland, 2013). Thus, in a in a cohort of patients diagnosed with persistent, treatment resistant depression the findings in this PhD study do not support the theory which underpins the SCS (Neff, 2003a; 2003b). This replicates findings in previous studies (i.e. Muris and Petrocchi, 2017), which are discussed in greater depth later in this chapter. These findings were also reflected in the qualitative data analysis.
In the examination of variance at baseline, scores on the OAS, FSCSR and SCS were only minimally affected by severity of depression as rated on the HDRS-17, BDI-I and PHQ-9. Only the OAS revealed a weak association with measures of severity of depression on the two selfrated measures of depression (BDI-I and PHQ-9). This suggests that whilst levels of shame to some extent may vary with severity of depression, this is not the case with self-criticism and self-compassion as measured on the FSCSR and SCS. The qualitative data analysis generated evidence that contradicts these finding in the quantitative analysis. This is discussed more fully later in this chapter. An interesting observation emerged in testing variance on the healthy controls whereby although the FSCSR and SCS demonstrated statistically significant differences with the study cohort, the former scored moderately highly on these two measures. This may suggest self-criticism and self-compassion are reflected in the concerns of the population in general.
Examination of the psychometric properties of the OAS, FSCSR and SCS in the study cohort
Steinmetz, (2015) states, when discussing factor loading coefficients in CFA, the strength of the factor loadings depends on the assumed theoretical relationship between the latent variable and observed indicator, which in turn depends on the meaning of the latent variable as articulated in the theory underpinning the measure. Thus, it is possible to derive a good model fit in CFA, but the factor has no association with the phenomenon as observed in the cohort studied. Steinmetz urges scrutiny of the item wording within a psychometric measure to assess its suitability in the context of the cohort being studied and advises the ‘rule of thumb’ should be: ‘apply theoretical thinking and think what the latent should mean’
(Steinmetz, 2015). A more detailed examination of the item content of the sub-scales of the OAS, FSCSR and SCS with reference to the quantitative and qualitative data analysis, and their utility when used to study a cohort of participants diagnosed with persistent, treatment resistant depression is presented below.
Examination OAS by sub-scale
Overall, the OAS performs as a reliable and valid measure in a cohort of patients diagnosed with persistent treatment resistant depression. However, each sub-scale did not perform equally well in terms of face, content and construct validity. A breakdown of the OAS by subscale and items can be seen in appendix XXXIV. The following interpretation of the data reflects the observations of Steinmetz (2015).
Sub-scale inferior
The sub-scale inferior demonstrates face, content and construct validity in a cohort of patients diagnosed with persistent, treatment resistant depression. The distributions revealed in the quantitative data analysis (see appendix XIX) for the sub-scale inferior In the quantitative data analysis, is consonant with the cohort studied and the theory which underpins the measure (Gilbert, 2007a; Gilbert and Goss, 1994 and Gilbert, Goss and Allen, 1994).
In examining the face validity of the item content which comprises the construct inferior
(see appendix XXIV) the items capture either explicit (i.e. items 2,5,6,8) or implicit (i.e. items 1, 4) perceptions of inferiority. Both the quantitative and qualitative data show the strongest support for the inferior construct. As reported in chapter 4 of this thesis, a better model fit in CFA than that proposed by Gilbert and Goss (1994) and Gilbert, Goss and Allan, (1994) emerged in this study when item 12 (‘others are critical or punishing of me when I make a mistake’) and item 13 (‘people distance themselves from me when I make a mistake’) from the mistakes construct of the OAS were loaded onto the inferior construct, with the two items emerging with negative loading parameters. This revised model fit which emerged is above the recommended fit indices used in this study (Hu and Bentler, 1998).
This revised model fit with negative loading parameters is reflected in clinical practice. Patients diagnosed with persistent, treatment resistant depression often report a sense of shame with regards to mistake making and fear criticism and ridicule from others if a mistake is made (often informed by emotional memories from childhood) and will compare themselves unfavourably to others when they make a mistake. Equally, depressed individuals are more prone to report mistake making as an indication of perceived inferiority (Moore and Garland, 2003; Williams, 1992, Beck, Rush, Emery and Shaw, 1979). This revised fit is in keeping with Gilbert’s formulation of depression and social rank theory (Gilbert, 2016; Gilbert, 2001; Gilbert, Birchwood, Trower, Hay, Murry, Meaden, Olsen and Miles, 2001; Gilbert and Allan, 1994). i.e. (thesis authors italics): ‘if I make a mistake, others are more likely to criticise or punish me and distance themselves from me, which places me lower in the social rank which denotes a greater degree of inferiority compared to others’. The qualitative data showed strongest support for the inferior construct (for example: see participant 9 (transcript 4, page 4 p 2, lines 31–36, 223 of this thesis); participant 12, (transcript 8, page 4, lines 79–82, p 226 of this thesis and participant 28, (transcript 5, page 4, lines 84–87, p 228 pf this thesis).
Sub-scale emptiness
The emptiness sub-scale does not demonstrate face, content and construct validity in a cohort of patients diagnosed with persistent, treatment resistant depression. The distribution for the sub-scale emptiness can be seen in appendix XX. From a theoretical perspective in terms of the population being studied and the theory which underpins the measure (Gilbert, 2007a; Allan, Gilbert and Goss, 1994 and Goss, Gilbert and Allan, 1994) this distribution is indicative of several patterns of response to the items in this sub-scale. In addition, the emptiness subscale shows weak item to item correlation for items 15 (‘others see me as fragile’) and Item 18 (‘other people feel I have lost control over my body and feelings’) showed a weak, test-retest reliability. The confirmatory factor analysis conducted on the OAS also reveals item 15 showing a weaker association with the construct emptiness and this item correlates poorly with the other items in this construct (16, 17, 18).
The construct emptiness does not appear to hold face validity in terms of item content in relation to this cohort. In the original validation of the OAS (Goss, Gilbert and Allan, 1994) the emptiness sub-scale was shown to have a stronger association with measures of depression than the other two sub-scales and this was replicated in one Italian study conducted on a cohort of undergraduate students (Balsamo, Macchia, Carlucci, Picconi, Tommassi, Gilbert and Saggino, 2015). This construct ‘emptiness’ is also consonant with the clinical observations described by Gilbert (Gilbert, 2010a) and is articulated in some of his research findings e.g. Gilbert, Cheung, Irons and McEwan (2005). However, given most of his studies are conducted on student populations the degree to which the results can be generalised to a clinical population diagnosed with persistent, treatment resistant depression is open to question. In terms of the content validity, the qualitative data supports these observations regarding the face validity of the emptiness construct. Only one participant gave an example that reflected the content of the emptiness construct. This was in relation to Item 18 (‘other people feel I have lost control over my body and feelings’) where participant 11 reflected on her perception of her own perceived lack of control over her thinking.
‘Would I say it (depression) was a weakness? Yes, I would. Because I have not got control. I like to have control over my thinking, but I don’t have control over my thinking’
(participant 11, transcript 10, page 11–12. Lines 214–218).
This is contrary to the theory which underpins the OAS, namely a focus on external shame, i.e. how self is experienced in the mind of the other.
This lack of face, content and construct validity in relation to the cohort studied here, may be accounted for in the fact, the items which constitute the OAS are derived from the clinical observations of Gilbert and his colleagues (Goss, Gilbert and Allan, 1994) when working with a range of patients presenting to an NHS clinical psychology service. Importantly Gilbert does not use diagnosis as a basis for clinical intervention and advocates what he terms a form of psychological formulation, evolutionary functional analysis (Gilbert, 2016). As identified in chapter 3, the OAS has never been tested on a clinical cohort diagnosed with persistent, treatment resistant depression. The clinical experience of the author of this thesis would indicate the construct emptiness is more in keeping with how patients meeting diagnostic criteria for Emotionally unstable Personality Disorder (EUPD) (ICD-10, 1994) or Borderline Personality Disorder (BPD) (APA, 2013) where patients often speak about their subjective sense of self as ‘fragile’ (item 15) and ‘empty’ and ‘unfulfilled’ (item 16) and item 18, ‘feeling out of control’ (see Whewell, 2002 for a useful summary). Within these self -descriptors there can be a sense of comparing self to others and these perceptions are often accompanied by intense feelings of shame. However, this differs from a sense that others view them in this way. Indeed Goss, Gilbert and Allan, (1994) when testing the OAS observed the following:
‘Certainly, in some theories of psychopathology issues of inferiority are believed to be more strongly associated with narcissism, whereas emptiness is seen as a more borderline phenomenon. Further, research is needed to explore this distinction’
(Goss, Gilbert and Allan, (1994) p 717.
Sub-scale mistakes
The sub-scale mistakes demonstrated face, content and construct validity in a cohort of patients diagnosed with persistent, treatment resistant depression. The distribution observed in the quantitative data analysis (see appendix XXI) is consonant with the cohort studied and the theory which underpins the measure (Gilbert, 2007a; Allan, Gilbert and Goss, 1994 and Gilbert, Goss and Allan, 1994).
In examining the face validity of the item content which comprises the construct mistakes the sub-scale contains items directly relating to mistake making and as a result others judging or punishing self in some way (items 12, 13, 14), items relating to others putting self down or looking for faults (items 3, 9,), one item referring to striving for perfection (item 10) and one item referring to defects (item 11). The construct mistakes has face validity in the context of the cohort studied, particularly in relation to items 3, 9, 12, 13, 14. This is supported by the qualitative data, for example participant 16, (transcript 7, page 12, lines 285–293 p 225 in this thesis).
As noted in chapter 4 (p 140) when the OAS was devised (Goss, Gilbert and Allan, 1994) item 10 in the mistakes sub-scale (‘people see me as striving for perfection but being unable to reach my own standards’) was retained and included in calculating the total score for the OAS but was not included in the sub-scale score as it failed to load above the cut off on any factor. This analysis was replicated in this PhD thesis. Item 10 was included here in the CFA to see how it performed. As can be seen in the CFA path diagram for the OAS (chapter 4, Figure 6, p 151) item 10 did not perform well which replicates the findings of Goss, Gilbert and Allan (1994) when the OAS was devised.
Suggested revisions to the OAS
Based on the interpretation of the data collected in this study the following modifications to the OAS are proposed which may improve its psychometric properties when administered to a cohort of patients diagnosed with persistent treatment resistant depression. As cited above, the CFA model fit for the OAS was improved by moving two of the items (12, 13) from the sub-scale mistakes to the sub-scale inferior and importantly this led to a strong association between these two sub-scales. Further, the qualitative data reveals most support for the inferior sub-scale and this is strengthened by the addition of items 12, 13 for which was also represented in the qualitative data. Rewording the poorly performing item 10 from the mistakes sub-scale in a way which better captures the essence of Gilberts’ formulation of external shame (i.e. sense of self in the mind of the other in relation to mistake making and depression), for example ‘People see me as trying very hard but I always get things wrong’ or ‘people see me trying hard to do my best but I always make a mistake’ may further strengthen the validity of the OAS in patients diagnosed with persistent, treatment resistant depression.
The theme defectiveness is present in two items on the OAS, item 7 (‘others see me as somehow defective as a person’) in the sub-scale inferior and item 11 (‘I think others are able to see my defects’) in the sub-scale mistakes. Both perform well in terms of factor loading (chapter 4, Figure 6, p 151). This theme of defectiveness did not emerge in the qualitative data but, in the authors experience it is a theme that emerges in therapy with patients diagnosed with persistent treatment resistant depression. In considering Gilbert’s shame theory which underpins the OAS (Gilbert, 2007a) it can be argued the theme defectiveness conveys a more fundamental sense of being at the bottom of a social rank. The clinical experience of the author of this thesis would argue that a sense of self as defective, is strongly associated with feelings of shame and to a sense of self as worthless in comparison to others. This theme of not worthy/worthlessness emerged strongly in the qualitative data (see chapter 5, e.g. participants 12 (transcript 8, p 10, line 222, p 201 of this thesis) , 28 ( transcript 5, p 4, lines 81–82, p 203 of this thesis) and 136 ( transcript 3, p 11–12, p 205 of this thesis) derived from childhood experiences characterised by ridicule and humiliation at the hands of others. This focus on childhood experiences in the context of current feelings of shame is central to Gilbert’s theory (Gilbert, 2016; Gilbert, Cheung, Grandfield, Campey and Irons, 2003; Gilbert, Allan and Goss, 1996).
The OAS may be improved as a measure of shame in a cohort such as the one studied here, if the sub-scale emptiness was replaced by a sub-scale aimed at tapping into sense of worthlessness of self in relation to others. It can be argued our sense of worth involves the concept of comparison and is conferred by socially proscribed constructs such as appearance, profession, salary, intelligence and the like and would therefore mesh well with the social rank theory in Gilbert’s model (Gilbert, 2007a). Such a sub-scale could incorporate Items 7 and 11 (defectiveness) alongside items which aim to tap into comparison of self to in relation to others i.e. ‘Others always view me as at the bottom of the pile’ and a judgement of worth i.e. ‘Others see me as having value as a person regardless of who I am’ or ‘others see me as a worthwhile person regardless of how well I do at things’. These three proposed interconnected constructs (inferior-mistakes-worthlessness) may more effectively capture shame in a cohort of patients diagnosed with persistent, treatment resistant depression as follows. Making mistakes denotes inferiority (in this testing of the OAS with this cohort mistake making items (12, 13) fitted more readily with the inferior sub-scale than the mistakes sub scale) and inferiority denotes worthlessness.
Previous studies of the psychometric properties of the OAS
To date this PhD thesis is the only study to test the OAS on a cohort of adults diagnosed with persistent, treatment resistant depression. A review of the literature up to 2019 (the chosen endpoint for inclusion of literature in this PhD thesis) revealed six publications investigating the psychometric properties of the OAS. Given most of these studies were conducted using a non-clinical sample and therefore are of limited value for comparison with the clinical cohort studied here, these studies are only reviewed briefly here.
Balsamo, Macchia, Carlucci, Picconi, Tommasi, Gilbert and Saggino, (2015) developed and tested an Italian version of the OAS on a sample of 687 undergraduate students and found evidence to support a hierarchical model with one higher order factor (external shame as reflected in total scores) and 3 first order factors, inferior, emptiness and mistakes. Matos, Pinto-Gouveia, Gilbert, Duarte and Figueiredo (2015) developed and tested a shortened (8 item) version of the OAS, (OAS-2), in an adult sample of 690 participants. The researchers report good internal validity (0.82) and state the OAS-2 shows good concurrent and divergent validity in comparison to the original OAS (0.91) and conclude the OAS-2 is a reliable and valid measure of external shame. Saggino, Carlucci, Sergi, D’Ambrosio, Fairfield, Cera and Balsamo, ( 2017) tested an Italian version of the OAS-2 using a cohort of 612, undergraduate students, which replicated the factor structure of the original OAS (Allan, Gilbert and Goss, 1994; Goss, Gilbert and Allan, 1994) and demonstrated good convergent and divergent validity and high correlation with measures of internal shame, anxiety and depression. Benevides, Da Motta, Sousa, Caldeira and Carvalho, (2016) developed a brief, adapted version of the OAS for use with children (OAS-C). The researchers tested this on a non-clinical sample of 127 children and using Exploratory Factor Analysis (EFA) found this to be an adequate measure of external shame in children. Vagos, Da Silva Ribeiro, Nelio, Rijo and Gilbert, (2016) tested the OAS and OAS-2 on three separate samples of Portuguese adolescents presenting with varying degrees of behavioural difficulties. Their results supported the three-factor model proposed by the OAS (inferior, emptiness, mistakes) and demonstrated the internal consistency and validity of both versions in relation to depressive, anxious and stress symptoms, self-criticism and selfreassurance, and experiential avoidance. Figueira, (2010) (unpublished manuscript) developed an adolescent version of the OAS (OAS-A) which Vagos, Da Silva Ribeiro, Nelio, et al, (2016) report as being a valid measure of external shame in this population. Cunha, De Jesus Xavier, Cherpe and Pinto Gouveia, (2017) tested a brief, 8 item version of the OAS for adolescents (OASB-A) on a non-clinical sample of 834 adolescents and demonstrated good internal consistency and adequate test retest reliability. Gouva, Paschou, Kaltsouda, Dragioti,
Paralikas, Mantzoukas and Kotrotsiou, (2016) developed and tested a Greek version of the OAS on a non-clinical sample of 294 adults drawn from the general population. The researchers demonstrated validity and reliability across a 3 factor model in keeping with the original OAS (Allan, Gilbert and Goss, 1994; Goss, Gilbert and Allan, 1994) and report good internal consistency (0.88) and test retest reliability and strong sub-scale associations (inferior
0.93, emptiness, 0.90 and mistakes 0.96).
Examination of the FSCSR and its sub-scales in relation to persistent treatment resistant depression
The FSCSR demonstrated good face, content and construct validity across all three subscales in a cohort of patients diagnosed with persistent, treatment resistant depression. The following interpretation of the data reflects the observations of Steinmetz (2015). A breakdown of the FSCSR by construct and associated items can be seen in appendix XXXV.
Subscale Inadequate self
The sub-scale inadequate self demonstrated good face validity in the context of the cohort studied. Items 1, 2, 6, 7, 14, 17, 18, in the sub-scale inadequate self are worded in a way that refers to social rank and to self not meeting the mark in some way and reflect how a selfcritical person may speak about self.
In the quantitative data analysis, (see Appendix XXII) the distribution is consonant with the cohort studied and the theory which underpins the measure (Gilbert, 2007a; Gilbert, Clarke, Hempel, Miles and Irons, 2004). In testing the psychometric properties of a measure handling outliers is a key factor, as how they are handled has implications for the conclusions drawn regarding the relationship between variables. Aguinis, Gottfredson and Joo (2013) observe the statistics literature lacks transparency in terms of how to manage outliers in a dataset. As an antidote to this they offer a comprehensive set of best practice principles for defining (14 definitions), identifying (39 statistical methods) and handling (20 statistical methods) outliers. The authors encourage the researcher to consider whether outliers provide new insights that may advance theory. With regards to the four outliers identified in the sub-scale inadequate self they all endorsed items at either ‘not at all like me’ or ‘slightly like me’ rendering an overall score that would indicate they did not assent to a sense of self as inadequate.
There may be a range of explanations for this including avoidant coping, namely, the questions were too distressing to engage with and therefore skimmed over leading to a misinterpretation of the Likert scale anchors. Avoidant coping being one of the emergent themes in the qualitative data in this PhD thesis. Equally, if mood was less depressed when these four participants completed the measure this may have lessened the negativity of their self-perceptions (this phenomenon from the cognitive science of depression is discussed later in this chapter) and thus lowered their scores. However, if this were the case it might be anticipated the same outliers would emerge in the sub-scale hated self, which they do not. Examining the content of the inadequate self a variety of descriptors are used to define sense of self (‘disappointment’ item 1; ‘not good enough’ item 6; ‘failure’ items 14 and 17 ‘inadequate’ item 17). The clinical experience of the author of this PhD thesis suggests that patients diagnosed with depression articulate perceptions of self that are idiosyncratic and nuanced. As such, it may be that for the four outliers the items in the sub scale inadequate did not tap into their core sense of self. This is a plausible explanation if, for example, their core sense of self is one of worthlessness which is not reflected in the FSCSR (or OAS, see previous discussion) but which is a prominent clinical feature in persistent, treatment resistant depression (see Moore and Garland, 2003; Williams, 1992; Fennell, 1989). In this regard, sense of self as worthless may be subsumed within the sub-scale hated self and hence the same outliers do not emerge in the sub-scale hated self.
Subscale Hated self
The sub-scale hated self demonstrated a degree of face validity in the context of the cohort studied. The items are worded in a way consonant with Gilbert’s theory (Gilbert and Irons, 2005) and reflect how some patients speak about themselves. In the quantitative data analysis (see appendix XXIII), the distribution observed is reflective of a range of responses to the items in this subscale. The authors clinical experience would indicate that the content of the item wording in the subscale hated self is most relevant when considering patients diagnosed with persistent, treatment resistant depression who have experienced sustained childhood trauma. Indeed participants 11, 20 and 88 in the qualitative data collected in this PhD study illustrates this point vividly (see chapter 5, pp. 206, 208 and 209). However, the intensity of self-hate and self-disgust captured in the item content is not representative across the board of how patients diagnosed with persistent, treatment resistant depression speak about themselves (see Luyten, Sabbe, Blatt, Meganck, Jansen, De Grave, Maes and Corveleyn, 2007; Haslam and Beck, 1994).
To elaborate on this observation, comparing items from the subscales inadequate self and hated self, item 4 in the subscale inadequate self, (‘I find it difficult to control my anger and frustration as myself’) and item 9, (‘I have become so angry with myself that I want to hurt myself’) in the subscale hated self both aim to capture a specific aspect of internal shame, anger towards self (see Gilbert, 2016; Gilbert and irons, 2005). Both perform poorly in item to item correlation and in CFA, suggesting a weaker relationship to their construct. However, in the qualitative data, examples of speaking both to self and about self with and in anger, in a voice tone that varied between hostile, contemptuous, ridiculing and self-hating was observed during the course of the interview whilst some participants were speaking (see chapter 5, pp. 207 and 210 for examples). To some extent the wording of items 2 and 4 may not capture how someone experiencing depression may characterise self-criticism/selfhating. The use of the phrases ‘difficult to control’ in item 4 and ‘I want to hurt myself’ in item 9 may reflect aspects of borderline personality traits which is a focus of Gilbert’s work (see discussion of this issue in OAS section above) rather than patients diagnosed with persistent treatment resistant depression.
This discrepancy between how the items perform in the quantitative and qualitative data analysis may also be a reflection of a frequent clinical observation when working with patients diagnosed with depression, namely, their self-criticism/self-hating is so habitual they do not recognise they are engaging in this and consequently do not endorse items 4 and 9 in a way that is consonant with Gilberts’ proposed model (Gilbert, 2016). The habitual nature of selfcriticism/self-hating was certainly borne out in the qualitative interviews in this study, where self-criticism and self-hating statements were spontaneously articulated as evidenced in both the content of language (including idioms) and voice tone (angry, contemptuous and dismissive of self) but passed unnoticed by the participant as they were spoken (e.g. see chapter 5 participant 28, p. 200 and participant 11, p 216).
Subscale Reassured self
In the quantitative data analysis (see appendix XXXIV) the distribution observed is consonant with Gilberts theory (Gilbert, 2007a) and would be expected in a cohort of patients diagnosed with persistent, treatment resistant depression.
In the item to item correlations the sub-scale reassured self does not perform well which may reflect the effect of a cohort of participants with depressed mood rating these items. Similarly, in the CFA for FSCSR (see chapter 4, figure 7, pp. 161), item 3 (‘I am able to remind myself of positive things I like about myself’) and item 16 (‘I am gentle and supportive of myself’) do not appear to fit well with the sub-scale. However, if these items are considered alongside two emergent themes in the qualitative data, the absence of self-compassion and the presence of memory and information processing biases that characterise depression, then it is possible that participants in the cohort studied here are less likely to positively endorse these items. As the cognitive science of depression literature indicates when mood is depressed thought processes are more negative (Disner, Shumake and Beevers, 2017) and information processing is more dichotomous (Teasdale, Moore, Hayhurst, Pope, Williams and Segal, 2002). Such mood dependent processing biases have potential to impact on how a questionnaire that asks the respondent to make ratings on a Likert scale (i.e. gradations of response from ‘very like me’ to not at all like me’) is endorsed. For example, item 3, (‘I am able to remind myself about positive things about myself’) will, (depending on level of depressed mood when completing the measure) be susceptible to mood dependent processing biases. Thus, if the respondents immediate response is ‘there is nothing positive about me’ which is a typical form of self-report noted in people with depressed mood, (Williams, Barnhofer, Crane, Herman, Raes, Watkins and Dalgleish, 2007; Moore and Garland, 2003) then this is likely to be negatively endorsed i.e. ‘not at all like me’. This negative bias in information processing and cognition content, which characterises depression, may in turn be further amplified in the context of dichotomous information processing when mood is depressed, (Teasdale, Moore, Hayhurst, Pope, Williams and Segal, 2002) by the fact all the items in the sub scale reassured self are positively worded. These dichotomous processing biases may play a role in accounting for the four outliers in this sub-scale, particularly if these respondents reacted adversely to the extremity of the language that comprise the items in the sub-scale hated self.
Previous studies of the psychometric properties of the FSCSR
The FSCSR has been tested in several previous studies, the majority of which have been conducted by the different combinations of members of a large group of researchers who collaborate with Gilbert, as is evidenced in the following summary of previous validation studies of the FSCSR. Kupeli, Chilcot, Schmidt, Campbell and Troop, (2012) tested the psychometric properties of the FSCSR on a non-clinical sample (n=346 undergraduate students and n=1,224 participants recruited online though social networking sites and health and wellbeing forums) conducting both Exploratory Factor Analysis (EFA) and CFA. Using EFA the researchers tested a one factor, two factor and three factor model and found the threefactor model demonstrated a superior model fit once they had removed items 4, 18 and 20 from the sub-scale inadequate self, (see appendix XXXV for the wording of these items) to enhance the factor structure. CFA conducted on this revised version showed the three-factor model of the FSCSR to be a reasonable fit. However, item 22 from the sub-scale hated self loaded onto to both reassured self and hated self, and the authors found both including and excluding item 22 derived an acceptable model fit. The authors (Kupeli, Chilcot, Schmidt, Campbell and Troop, 2012) conclude their results support the underlying theoretical model proposed by Gilbert (Gilbert, Clark, Hempel, Miles and Irons, 2004).
Castilho, Pinto-Gouveia and Duarte, (2015) tested the CFA of the Portuguese version of the FSCSR on a sample of 685 participants comprising a mixed clinical sample (n=304), consisting of axis I anxiety disorders, depression, PTSD and eating disorders with some co-morbid axis II features(n=381) and a non-clinical sample consisting of a community sample drawn from different regions of Portugal (n=111) and a student sample from the university where the research was conducted (n=270). The three-factor model of the FSCSR in each group showed the most acceptable fit and tests of construct and discriminant validity supported the theoretical model that underpins the FSCSR. Meanwhile, Baiao, Gilbert, McEwan and Carvalho, (2015) explored the psychometric properties of the FSCSR in a large sample (clinical sample n=167 of patients with mixed diagnoses and non- clinical sample n=887) drawn from the collated data from 12 different previous studies. The authors conducted CFA separately on the data from the clinical and non-clinical samples and conclude the FSCSR is a reliable measure of self-criticism and self-reassurance in both clinical and non-clinical populations. Halamova, Kanovsky, Gilbert, Troop, Zuroff, Hermanto, Petrocchi, Sommers-Spijkerman, Kirby, Shahar, Kreiger, Matos, Asano, Yu, Basran and Kupeli (2018) tested the factor structure of the FSCSR in thirteen non-clinical samples in 12 different countries (eight language versions of the FSCSR) testing two factor, three factor, bi-factor and two tier models using more advanced statistical analysis than the earlier studies cited above. An acceptable fit was found for the original three factor model proposed by Gilbert and colleagues (Gilbert, Clark, Hempel, Miles and Irons, 2004) but identified the best fit as being achieved by the two-tier model, with inadequate self and hated self loading on to self-criticism and reassuring self loading on to self -reassurance. The authors propose a modified use of the FSCSR in which the self-criticism and self-reassurance factor total scores are used as separate entities to assess changes in both domains during psychotherapy and experimental research. The authors also emphasise the potential relationship between self-criticism and psychopathology (Baiao, Gilbert, McEwan and Carvalho, 2015) and self-reassurance and wellbeing (Gilbert, 2017a). The authors do caution that the single self-criticism factor which emerged may be a product of psychometric artefact arising from the fact the items which comprise the inadequate self and hated self are negatively worded, whilst the items in the reassured self factor are positively worded. This dichotomy may lead respondents to differentiate between two types of selfcriticism because they are overly influenced by the perceived larger differences between positive and negative items than between two different forms of self-criticism (Halamova, Kanovsky, Gilbert, Troop et al, 2018). A further caution identified is that in factor analysis negative items often cluster into a separate factor and these factors can be falsely interpreted as meaningful when in fact their content co-varies with the negative item format. As a result, the sub-scales are methodologically rather than theoretically derived. Given these cautionary notes and the fact the original three factor model proved an acceptable fit in this study the authors call for further research to discriminate between self-correcting and self-hating forms of self-criticism in clinical populations (Halamova, Kanovsky, Gilbert, Troop et al, 2018). This final point is worthy of note given in this PhD study an emergent theme in the qualitative data was the function of self-criticism, with four participants (8, 9, 20, 28) identifying that selfcriticism served the purpose of assisting in maintain high standards, which would be akin to the selfcorrecting form of self-criticism described above. Meanwhile, participant 20, expressed sentiments more in keeping with the self-hating forms of self-criticism in which he identified the purpose of his self-hate as being guarding against self-indulgence and protecting his true nature (‘not a good person’) being revealed to others (e.g. see chapter 5, page 217).
Examination of the SCS by sub-scale in relation to persistent treatment resistant depression
The quantitative data for the SCS collected in this PhD study revealed issues of multicollinearity and multidimensionality (see appendices XXV to XXX for distribution for each sub-scale of the SCS). Similarly, in the qualitative data, themes and sub-themes emerged that are not consonant with the dimensional relationship between the sub-scales in the SCS (self kindness vs. self-judgement, common humanity vs. isolation and overidentification vs. mindfulness) as proposed by Neff (2003a; 2203b) and which were investigated here. Thus, combining the quantitative and qualitative data it is concluded that the SCS did not perform as a valid and reliable measure in a cohort of patients diagnosed with persistent, treatment resistant depression.
Given the above conclusion what will follow is a critique of the SCS, considering the collated quantitative and qualitative data derived from this PhD study. This critique takes into consideration the observation by Steinmetz, (2015), that it is possible to obtain a good model fit in CFA, but the factors have no association with the phenomenon as observed in the cohort studied. This is of relevance in this current study where, not only does the quantitative data reveals poor discriminant validity, as evidenced by the strong correlations between the negative sub-scales and the positive sub-scales in the CFA, also the qualitative interviews (albeit a small sample (n=10) do not reveal any data to support the positive anchors (selfkindness, common humanity and mindfulness) of the SCS sub-scales. The qualitative interviews yield consistent data to support the negative anchors (self-judgment, isolation and overidentification) of the subscales. Based on these observations from the quantitative and qualitative data it can be argued that the negative sub-scales of the SCS tap into the psychopathology of depression and therefore its theoretical foundations can be questioned. This is discussed in greater depth below as several studies conducted since the commencement of this PhD have noted similar concerns (see Geiger, Pfattheicher Hartung, Weiss Schindler and Wilhelm 2018; Muris and Petrocchi, 2017; Pfattheicher, Geiger, Hartung, Weiss and Schindler, 2017; Muris, Otgaar and Petrocchi, 2016; Costa, Maroco, Pinto-Gouveia, Ferreria and Castilho, 2016; Williams, Dalgleish, Karl and Kuyken, 2014).
The content of the items in the SCS (see appendix XXXVI) do not hold face validity when administered to a cohort of participants diagnosed with persistent treatment resistant depression. For example, data from the qualitative interviews indicates that participants struggled to see themselves as suffering even in context of their own subjective experience of depression. In this regard participants may have struggled to engage with the language used by Neff in the items in the self-kindness -self-judgement sub-scale i.e. item 12, ‘When I’m going through a very hard time, I give myself the caring tenderness I need’. Indeed, as reported in the quantitative chapter of this thesis 9 participants failed to complete at least one item on the self-kindness sub-scale and 8 participants failed to complete at least one item of the self-judgement sub-scale. This may reflect the degree of difficulty the participants experienced in answering the items, not just in terms of deciphering meaning, but in terms of distress activated by the idea of self-kindness and self-judgement per se. The research associates who collected the quantitative data in the RCT in which this PhD was based, reported that participants frequently voiced difficulty in completing the SCS both in terms of content and its length. This missing data is reflected in each sub-scale of the SCS, which may be an indication of avoidant coping which was an emergent theme in the qualitative dataset. This observation may also account for the outliers which emerged in each sub-scale.
Taking into consideration issue of multicollinearity which arose in the quantitative analysis, it is possible to observe the overlap in item content between the two most strongly correlated sub-scales in the quantitative data set Self-judgment and overidentification. For example, item 6 in the sub-scale overidentification: ‘when I fail at something important to me, I become consumed by feelings of inadequacy’ and item 1 in sub-scale self-judgement: ‘I’m disapproving and judgemental about my own flaws and inadequacies’. The general wording of both items implies a negative stance towards self and the use of the words such as fail, flaws and inadequacy are in themselves labels that confer a very harsh judgement of self. Another example of overlapping constructs between the sub-scales can be illustrated as follows. In the self-kindness-self-judgement sub-scales Neff (2003a; 2003b) uses the word suffering as part of her definition of self-compassion, that is, using self-compassion to alleviate suffering i.e. item 19 in the self-kindness subscale ‘I’m kind to myself when I’m experiencing suffering’. Meanwhile, Item 21 of the self-judgement scale also contains the word suffering, ‘I can be a bit cold-hearted towards myself when I experience suffering’. Similarly, the words inadequate, inadequacy and inadequacies and failure and failings appear in both the common humanity and isolation and the overidentification and mindfulness subscales. This use of negative wording (in both positive and negative sub-scales) will hold greater valence for a cohort of participants diagnosed with persistent, treatment resistant depression which may impact on how items are comprehended and endorsed. This may also account for outliers, which are present in each subscale.
To elaborate further on these assertions, three key emergent themes in the qualitative data were identified. Firstly, sense of self, in which all the sub-themes reflected a negative sense of self. That is:
-
not good enough/inferior/failure associated with self-criticism.
-
Unimportant/not counting/not worthy associated with self-blame
-
Bad/inadequate/insignificant/worthless associated with self-hate and self-loathing
Secondly, a theme the function of self-criticism and finally a theme of absence of selfcompassion (with sub-themes of intellectual appreciation of, incomprehension, not deserved, risky). These themes not only readily tap into self-judgment, isolation and overidentification, they exclude the possibility of self-kindness, common humanity and mindfulness.
For example, in examining the qualitative data with regards to the self-judgement sub-scale, self-criticism serving a function was identified as an emergent theme. All ten participants gave examples of varying degrees of self-criticism, self-blame and self-hate. This was frequently, observed by the interviewer as participants spontaneously engaged in selfcriticism/self-hating in the moment during the interview. This was reflected in the language, paralanguage, facial expression and voice tone used by participants at specific points during the interviews. These findings provide evidence that the SCS lacks internal validity as the data does not support Neff’s formulation of self-compassion (Neff, 2003a; 2003b) by which, for example, as self-kindness increases then self-judgement decreases and vice versa and so on with the other sub-scales. As a result, the SCS lacks conceptual and empirical veracity (see discussion below from Costa, Maroco, Pinto-Gouveia, Ferreria and Castilho, 2016).
The language and phrasing used by Neff (2003a) reflects the fact The SCS item content was derived and the SCS subsequently tested using a cohort of US undergraduate university students who did not meet diagnostic criteria for clinical depression. Some of the phrasing of items are indicative of US idioms which do not translate into the same meaning in British culture. For example, item 16 in self-judgement sub-scale, ‘When I see aspects of myself I don’t like I get down on myself’. In American English usage the phrase ‘get down on’ means to ‘keep criticising someone or something’ (Macmillan online Dictionary, 2020). This phrase would not be used in British English to describe criticism of self. Similarly, in common humanity sub-scale item 7 reads, ‘When I am down and out, I remind myself there are lots of other people in the world feeling like I am’. The phrase ‘down and out’ refers to a person who has no job, money or accommodation i.e. homeless (Ayto, 2010, p101). This is at best inelegant phrasing in a psychometric measure and potentially problematic in terms of maximising the likelihood of respondents engaging with authenticity in completing the measure. In this regard, it can be argued the wording of the items in the SCS do not readily translate from a US to British context.
Further, in examining the face validity of the items in the self-judgement, isolation and overidentification sub-scales the inclusion of words such as inadequate and failure reflect the language used by participants to describe sense of self which are cited by participants in the qualitative interviews (e.g. see participant 20, p. 208 and participant 15, pp. 209–210). These sub-scales also reflect the memory biases cited in the cognitive science of depression literature. For example, all ten participants reported examples of overidentification when mood was depressed, the content of which was self-criticism, self-blame and/or self-loathing (e.g. see participant citations in chapter 5, pp. 220–222). This parallels the quantitative data where the two most strongly correlated sub-scales in the SCS were Self-judgment and overidentification, which is akin to the process of rumination, a central feature of persistent, treatment resistant depression (Watkins and Teasdale, 2004; Nolen-Hoeksema, 2000). Further, all ten participants recognised that as their mood became more depressed their selfcriticism and self-hating became more pervasive, intense and harsh. In addition, participants readily identified how difficult it was for them to have compassion towards themselves most of the time, regardless of level of depressed mood. Further, no participant reported that as mood improved, they became more kind towards themselves, they only recognised they were not as self-critical and self-hating once depressed mood began to remit. This finding, taken alongside the emergent theme, ‘absence of self-compassion’ provides evidence against Neff’s assertion (Neff, 2003a, 2003b) of a linear relationship between the two constructs in each sub-scale i.e. as self-judgement lessened self-compassion increased. This observation is in keeping with other SCS validation studies and is discussed further in the next section of this chapter.
Previous studies of the psychometric properties of the SCS
Since the commencement of this PhD study there have been numerous studies testing the psychometric validity of the SCS. Two meta analyses summarising this literature (Muris and Petrocchi, 2017 and MacBeth and Gumley, 2014) cite a range of publications which have tested the factor structure of the SCS on a variety of clinical and non-clinical (community samples and student cohorts) populations including adults, older adults and adolescents and across a range of nations (Belgium, China, Germany, Greece, Iran, Italy, Korea, Portugal, Spain,
Thailand and Tawian, the Netherlands and Turkey (see Muris and Petrocchi, 2017 p 374).
Overall the literature reflects inconsistent findings regarding the psychometric validity of
Neff’s (Neff, 2003a; 2003b) six factor structure of self-compassion (Geiger, Pfattheicher Hartung, Weiss Schindler and Wilhelm 2018; Kumlander, Lahetinen, Turunen and Salmivalli,
2018; Brenner, Heath, Vogel and Crede, 2017; Muris, Otgaar and Petrocchi, 2016; Lopez, Sandeerman, Smink, Zhang, van Sonderen, Ranchor and Schroevers, 2015; Williams, Dalgleish, Karl and Kuyken, 2014). This critique is summarised below.
Muris, Otgaar and Petrocchi (2016) observe that in her original validation of the SCS Neff (Neff, 2003b) had already established that the three dimensions she originally proposed, selfkindness vs. self-judgement; common humanity vs. isolation and mindfulness vs. over identification did not emerge in her study of the psychometric properties of the SCS. On this basis Neff (2003a) proposed a six-factor model in which the total score of all six sub-scales rendered an overall score of self-compassion (as defined by Neff). Muris, Otgaar and Petrocchi (2016) argue that, as a result, (as successive research groups have used the SCS in a broad range of studies) this has led to an assumption that the SCS comprises six sub-scales, with 3 subscales representing positive indicators of the self-compassion construct (selfkindness, common humanity, mindfulness) and 3 subscales representing negative indicators of the self-compassion construct (self-judgement, isolation and over identification). Importantly, according to Muris and colleagues, researchers using the SCS have neglected this issue of positive and negative indicators and only compute a total score by summing the ratings across all items (reversing the negative indicator items). In this PhD study, this is how the scores were collated. As a result, the authors argue Neff’s theoretical formulation of selfcompassion which underpins the SCS (Neff, 2003a; 2003b) and how the items which comprise the SCS operationalises her formulation of self-compassion is open to criticism and thus the internal validity of the SCS can be questioned (Muris, Otgaar and Petrocchi 2016; Steinmetz, 2015).
In their 2014 paper, Williams, Dalgleish, Karl and Kuyken, (2014) tested the six-factor structure of the SCS on three different clinical and non-clinical population samples. The researchers criticise Neff’s original (Neff, 2003a) SCS validation study on the grounds she only reports two fit indices and deploys too liberal cut off criteria, arguing these criteria are insufficient to adequately assess goodness of fit in SEM. In their testing of the SCS they report six goodness of fit indices (Williams, Dalgleish et al (2014) and more conservative cut off indices (Schermelleh-Engel, Moosbrugger and Muller (2003)). In this PhD study the fit indices which emerged in the quantitative data analysis for the SCS fall between the conservative and liberal cut offs proposed by Williams and colleagues, who conclude that the SCS is not of clinical utility in measuring self-compassion and call for more psychometrically robust measures to be developed.
Costa, Maroco, Pinto-Gouveia, Ferreria and Castilho (2016) carried out a validation study of the SCS in Portugal, on a convenient sample of three clinical cohorts and a cohort drawn from the general population. They tested the six- factor model proposed by Neff (2003a); a twofactor model of self-compassionate attitude (loading onto the positive sub-scales of the SCS: self-kindness, common humanity, mindfulness) and self-critical attitude (loading on to the negative sub-scales of the SCS: self-judgement, isolation, overidentification) and measurement invariance across the four cohorts studied. The best fit was found for a bifactor model which revealed a moderate negative correlation between the two constructs selfcompassionate attitude and self-critical attitude. Both factors showed convergent and discriminant validity which indicates each factor is best accounted for by the items from which it is comprised rather than from the items in the opposing factor. The researchers conclude that their findings are not in keeping with Neff’s (2003a, 2003b) formulation of selfcompassion as consisting of three continuous dimensions ranging from positive to negative (i.e. self-kindness to self-judgment, common humanity to isolation, mindfulness to overidentification) and identify a lack of empirical and conceptual foundation to her model of self-compassion. Specifically, in relation to Neff’s original validation studies (Neff, 2003a, 2003b) they observe that during the design of the SCS an assumption was made that the scale items were correlated with the sub-scale to which they were assigned, but this assumption was never tested by Neff. Further the various rounds of CFA carried out by Neff were all conducted on the same sample, which the researchers argue can artificially inflate goodness of fit models. Costa, Maroco, Pinto-Gouveia, Ferreria and Castilho (2016) also question the decision to reverse score the negative sub-scale items and argue Neff’s assumption of the SCS possessing a unitary structure whereby the presence of one pole implies the absence of the other is founded in methodological and conceptual incoherence. Taking this unitary construct perspective does not allow investigation of whether changes in the overall score on the SCS are a result of increases in the positive score of self-kindness or a decrease in the negative score of self-judgement. As discussed earlier in this chapter, data from this PhD thesis supports this final observation made by Costa, Maroco, Pinto-Gouveia, Ferreria and Castilho (2016) and Lopez, Sanderman, Smink, Zhang, Sonderen, Ranchor and Schroevers, (2015) that with regards to the SCS a bi-factor model of self-compassion (positive sub-scales) and selfcriticism (negative subscales) may be more helpfully formulated as separate constructs related to psychological resilience and vulnerability respectively.
Pfattheicher, Geiger, Hartung, Weiss and Schindler, (2017) and Geiger, Pfattheicher, Hartung, Weiss, Schindler and Wilhelm (2018) have also tested the factor structure of the SCS. Their results concur with those of Costa, Maroco, Pinto-Gouveia, Ferreria and Castilho (2016) and Lopez, Sanderman, Smink, Zhang, et al, (2015). Once more, they recommend that researchers do not use the SCS total score across all items to derive an overall level of self-compassion. They also propose a bi-factor model of the SCS, one comprising the positive sub-scales, selfcompassion and one comprising the negative sub-scales, emotionality and harsh selfjudgement. Having tested the SCS against the Five Factor Model of Personality focusing on neuroticism (Goldberg, 1990), Pfattheicher, Geiger, Hartung, et al, (2017) found correlations between anxiety, depression and self-consciousness (aspects of neuroticism) and the negative items in the SCS were extremely high. The authors conclude the negative items from the SCS be removed as these reflect neuroticism and therefore tap into psychopathology, which therefore represent vulnerability factors for depression and anxiety.
The work of Muris, Otgaar and Petrocchi, ( 2016) and Pfattheicher, Geiger, Hartung, et al, (2017) has led to a series of ripostes from Neff (Neff, 2016a; 2016b) and further validation of the SCS by Neff and colleagues (Neff, Toth-Kiraly and Colosimo, 2018; Neff, Whittaker and Karl, 2017). A vigorous debate between the three research groups has emerged in the research literature. In response to these criticisms Neff has conducted further psychometric testing of the SCS (Neff, Toth-Kiraly and Colosimo 2018; Neff 2016). Importantly here Neff and colleagues did find an overlap between self-compassion (as defined by Neff’s (2003a) and neuroticism and depression with the two constructs sharing two-thirds of their variance. Neff, Toth-Kiraly and Colosimo (2018) argue this large overlap does not necessarily indicate they are measuring the same construct. Whilst Neff (2016b) concedes that the definitions she uses for the negative sub-scales overlap with research in the field of psychopathology, she argues that her goal is to enable the development of a self-compassion state of mind in which self-judgment, isolation and overidentification are reduced. In this regard Neff does not define the negative sub-scale factors as forms of psychopathology.
Neff defends her definition of self-compassion (Neff, 2016b) as three positive (self-kindness, common humanity and mindfulness) and three negative components (self-judgement, isolation and overidentification) which have a linear relationship. Neff (Neff, 2016b) cites the work of Gilbert (Gilbert, 2010) and Neff and Germer, (2013) and Germer, (2009) as examples of interventions that aim to achieve the goal cited above. However, the personal experience of the author of this PhD thesis, having attended a five-day self-compassion experiential retreat led by Neff and Germer (2012) is as follows. Neff has no clinical background and does not speak about how to use her self-compassion programme named Mindfulness SelfCompassion (MSC) (Neff and Germer, 2013) with a clinical population. Further, in the clinical component of workshop Germer conceded that the clinical examples British participants brought from their NHS practice were complex and beyond his experience of using MSC. This raises the question of the degree to which Neff’s work belongs more to the positive psychology movement which is prominent in both academic and public spheres in the USA (a point Neff contests in her defence of her definition of self-compassion, (Neff, 2016b)). Further, Neff’s formulation does not consider self-compassion in the context of psychopathology and the cognitive science of emotional disorders, but rather, as she herself states, ‘for the general public, as well as academics’ (Neff, 2016b, p 794).
Summary of quantitative and qualitative data in this PhD thesis in the context of Gilbert’s
evolutionary biopsychosocial model
The quantitative data from the OAS and FSCSR and the qualitative data collected within this PhD study support Gilbert’s formulation of internal and external shame in a cohort of patients diagnosed with persistent, treatment resistant depression. Traditionally psychiatry formulates shame as a biological symptom of depression which improves as severity of depression improves. The data derived from univariate and multivariate analysis conducted in this PhD thesis showed that the OAS was minimally affected by scores on the BDI-I and PHQ-9 but not the HDRS-17 (the HDRS-17 is a measure of biological symptoms of depression as defined by the diagnostic criteria used in psychiatry in the UK in the 1960’s when the HDRS was devised (Hamilton, 1960)). This raises the question of whether there is clinical utility in formulating shame and self-criticism as a psychological facets of depression and if so, what are the parameters of a psychological formulation of shame in depression?
In his evolutionary psychobiosocial model Gilbert (2007a) defines internal shame as how a person thinks and feels about themselves, seeing self as inferior, inadequate or bad and making a negative social comparison of self with others. This internal shame is associated with feelings of anger, anxiety and disgust towards self. Meanwhile external shame is defined as a perception others look down on self and that others view them as inferior or socially undesirable, anticipating others will feel contempt, disgust or ridicule towards them. Gilbert terms this as ‘sense of self in the mind of the other’ (Gilbert, 2017a; Gilbert, 2007a).
Gilbert, (Gilbert, 2017; 2007a) gives primacy to external shame and self-criticism is formulated as an aspect of internal shame. Thus, the OAS is a measure of external shame and the FSCSR is a measure of internal shame and it is on this basis that in seeking to interpret the data gathered in this PhD study the OAS and FSCSR are considered in tandem alongside the qualitative data, when formulating shame and self-criticism and absence of self-compassion as psychological facets of depression, in a cohort of patients diagnosed with persistent,
treatment resistant depression.
The healthy control group in this PhD study (N=30) scored moderately highly on the FSCSR. This finding supports previous research where the FSCSR has been tested on non-clinical and community samples and the CFA conducted demonstrated a good model fit (i.e. Castilho,
Pinto-Gouveia and Duarte, 2015; Kupeli, Chilcot, Schmidt, Campbell and Troop, 2012; Gilbert, Clark, Hempel, Miles and Irons, 2004). As Baiao, Gilbert, McEwan and Carvalho, (2015) observe, this suggests the theory underpinning the FSCSR has validity in populations without psychopathology and raises the possibility that self-criticism in varying degrees can be observed in the general population. This position reflects Beck’s theoretical proposition that emotional disorders exist on a continuum with normal emotional reactions (Beck, 1967; 1963), a clinical observation that has subsequently been supported by experimental research in cognitive science. Specifically, that it is the frequency, intensity and persistence of negative appraisals that differentiate between clinical and non-clinical groups where depressed mood has been shown to be a mediating factor (for a comprehensive review see Harvey, Watkins, Mansell and Shafran, 2004). This observation is made by Thew, Gregory, Roberts and Rimes, (2017) who explored the phenomenology of critical thinking and its relationship to other cognitive constructs in clinical and non-clinical cohorts (depression n= 26; eating disorders, n=26 and non-clinical (undergraduate students and university staff) n = 26) and found selfcritical thinking to be highly correlated with higher levels of depression, perfectionism, rumination and lower self-compassion. Further, the authors observe that participants displayed a global negative attitude towards self, alongside self-critical thinking being both habitual and automatic. Studies which investigated the psychometric properties of the FSCSR scale which included a non-clinical sample make similar observations (Halamova, Kanovsky, Gilbert, Troop et al, 2018; Castilho, Pinto-Gouveia and Duarte, 2015; Kupeli, Chilcot, Schmidt, Campbell and Troop, 2012).
In this PhD study the univariate and multivariate regression data revealed scores on the FSCSR at baseline showed a weak association with severity of depression, whilst in the qualitative data analysis all 10 participants reported increase in the frequency, intensity and duration of shame and self-criticism with severity of depression. This may be accounted for by the possibility that the key factor in severity of depressed mood is rumination and that what the participants in the qualitative arm of the study are reporting is self-critical, self-blaming, selfhating rumination which is amplified as mood becomes more depressed. Rumination was not measured in this PhD study but in the cognitive science literature the relationship between rumination and depressed mood is well documented (Watkins and Teasdale, 2001; Watkins and Teasdale, 2001; Nolen-Hoeksema, 2000).
Spasojevic and Alloy, (2001) in a prospective study found that individuals who reported affectionless, overcontrolling parents of either gender were more likely to engage in rumination in response to depressed mood. The authors posit an explanation in terms of childhood environment whereby, overcontrolling parents fail to teach their children active coping strategies which results in a lack of capacity to exert mastery and control over their environment. Consequently, the child turns inwards, using rumination as a means of managing sadness, which becomes more habitual and entrenched as they grow older. This predisposes the child to depression. Robinson and Alloy, (2003) expand on this finding in a subsequent paper from the same study where they tested their proposed attributional model of stress-reactive rumination. They concluded that individuals who make negative inferences for negative life events and then repeatedly activate these negative interpretations through rumination are vulnerable to repeated episodes of depression and hopelessness. However, the authors do not conclude a ruminative response style confers vulnerability to depression but rather negative cognitive styles mediated the relationship between lack of warmth/rejecting parenting style and depression (Alloy, Abramson, Hogan, Whitehouse, Rose, Robinson, Kim, and Lapkin (2000)).
A strong emergent theme in the qualitative data was memory biases in depression (see chapter 5, p 220–222) for which there is a strong evidence base in the cognitive science of depression literature (Williams, Barnhofer, Crane, Herman, Raes, Watkins and Dalgleish, 2007; Williams, Watts, MaCleod, and Mathews, 1997; Williams and Broadbent, 1986). Gilbert does not formulate according to diagnostic categories and as such does not consider the cognitive science of depression literature within his formulation of shame and self-criticism. He does refer to emotional memories and to rumination but does not consider these phenomena in relation to the well-established findings that exist in the cognitive science of depression literature. Of relevance here is, the role of thought suppression in depression (Wenzlaff and Luxton, 2003); the reciprocal relationship between over-general memory and rumination (Watkins, Teasdale and Williams, 2000), which is formulated as a tacit emotional regulation strategy developed in childhood in the face of hostile and critical parenting styles and intrusive memories in depression (Brewin, Wheatley, Patel, Fearon, Hackmann, Wells, and Myers, 2009). In the qualitative interviews in this PhD study all ten participants each without prompting from the interviewer, reported recognising, not only a greater degree of negativity to their thought processes when mood was more depressed, but also an increase in the frequency, intensity and tone of their self-criticism/self-blame/self-hate and a more harsh stance towards self generally. Equally, those who reported shame reported a subjective sense of a reciprocal relationship between severity of depression and intensity of feelings of shame. This may indicate that shame, self-criticism and self-compassion do not simply function as a corollary of depressed mood but as psychological aspects of depression that in a persistent, treatment resistant clinical presentation are significant obstacles to symptom remission and require active targeting with psychological interventions. In considering the contrary finding from the quantitative data regarding severity of mood and intensity of selfcriticism and shame, more recent research has formulated rumination, thought suppression and dissociation as experiential avoidance strategies (Matos, PintoGouveia and Duarte 2012). These strategies may play a role in dampening high levels of unregulated affect in the moment. However, in the medium and long term may amplify (via a rebound effect) the psychological aspects of shame and self-criticism/self-blame/self-hate particularly if, as the cognitive science of depression literature supports, intrusive, depressive autobiographical emotional memories become more accessible as depressed mood worsens.
Recent work in autobiographical memory has formulated shame as a traumatic memory (Matos, Pinto-Gouveia and Duarte 2012; Matos and Pinto-Gouveia, 2010). The authors posit that shame memories can act as threat based emotional hot spots (cf. Gilbert, 2003) which can possess similar characteristics to trauma memories, namely an intrusive quality, flashbacks, emotional avoidance, hyper arousal, fragmented mind set and dissociation (Matos, Pinto-Gouveia and Duarte 2012). The researchers frame their theory in Gilbert’s evolutionary psychobiosocial model of shame (Gilbert, 2007a) and argue that early nterpersonally focused shame experiences in childhood, where the child experiences the negative emotions of others directed at self gives rise to negative emotional memories. These shape self-experience and self-evaluation, honing global attributions of self and identity as narratives about self and life (Matos, Pinto-Gouveia and Duarte 2012). Thus, shame experiences (i.e. experiences of criticism, humiliation, rejection and ostracism from parents/teachers/peers, bullying, failing at something important, physical and sexual abuse) lay down autobiographical memories as conditioned shame focused emotional memories (Matos, Pinto-Gouveia and Duarte 2012). These emotional memories direct aspects of attentional, emotional and cognitive processing in such a way that self is experienced as, for example, inferior, worthless, bad and others as critical, hostile, controlling and potentially ridiculing, rejecting or harmful to self (Pinto-Gouveia, Castilho, Matos and Xavier, 2013). This concept is supported by the quantitative and qualitative data collected in this PhD study. The quantitative data maps how participants view themselves within Gilbert’s theory of internal and external shame (Gilbert, 2007a) and the qualitative data maps participants observations of how early experiences in the context of others shaped their sense of self and self in relation to others in the here and now (see citation from study participants in chapter 5 pp. 191–193).
A criticism of Gilbert’s model is that it fails to consider the well validated body of research in the field of attributional models of depression (Bernstein, Evan, Van Bork, Moriarty, et al,
2019; Seligman, Abramson, Semmel and von Baeyer 1979; Abramson, Seligman and Teasdale, 1978; Abramson and Sackheim, 1977) which may be important to consider clinically when working with patients diagnosed with persistent, treatment resistant depression. Gilbert is clear that his model is not one of attribution but one of affiliative and emotional processes (Gilbert, 2010; 2007a) in which external shame, i.e. sense of self in the mind of the other is the primary driver of emotional disorders. Gilbert makes no direct reference to attribution in his theoretical model but there are references to the work of attributional theorists in his later work (Gilbert, 2017a). His Compassion Focused Therapy (CFT) also contains interventions which target attributions in the form of seeking to modify self-critical thoughts by generating a sense of warmth and more compassionate internal dialogue towards self (Gilbert and Choden, 2013) which involves both attributional, affiliative and emotional processes.
It can be argued the items and constructs which comprise the OAS and FSCSR not only tap into attributions about self and self in relation to others, in terms of how they are worded and presented but, that attributions are the focus of investigation in these measures. Thus, the CFA in this PhD study revealed a strong association between the mistakes and inferior subscales of the OAS. Similarly, for the FSCSR there emerged a strong positive association between inadequate self and hated self and a moderate negative association between hated self and reassured self and inadequate self and reassured self. Thus, it can be argued these constructs can be viewed through the lens of models of negative attribution and cognitive styles (Bernstein, Evan, Van Bork, Moriarty, et al, 2019; Seligman, Abramson, Semmel and von Baeyer 1979) and attributional models of shame (Tracy and Robins, 2007a).
In considering the attributional models of shame (which are derived from the depression and attribution literature) (Tracy and Robins 2007a; Lewis, 2007; 2000) outlined in chapter 2 of this thesis, the constructs which form the sub-scales of the OAS and FSCSR can be presented as varying degrees of attribution from external-unstable-specific to internal-stable-global (Tracy and Robins 2007a). For example, mistake making often has more flexibility in terms of attributional style i.e. a mistake can more readily be attributed as external, specific and unstable (i.e. ‘My cake did not rise because I used the wrong flour’). Meanwhile inferiority, (which speaks to social comparison and rank ordering of self) may have a degree of flexibility i.e. internal, specific, unstable, (i.e. ‘Susan is a better baker than I am, my cake did not rise as well as hers, but it did rise more than Johns’). Meanwhile, worthlessness, by definition, is an internal, stable, global/uncontrollable attribution (‘My cakes never rise because I am useless and there is nothing I can do about that’).
Thus, considering attributional models of shame, where the individual makes a failure evaluation in relation to their own standards, rules and goals (SRG’s) (Lewis, 2007), or, using Tracy and Robins (2007a) attributional formulation, if sense of self as useless is attributed as an internal, stable, uncontrollable attribution this will elicit shame. For example, receiving a diagnosis of depression may elicit feelings of shame if the SRG’s in their childhood environment imbued a sense that having a mental health problem is a sign of ‘madness’ and ‘madness’ is seen as something intrinsic to a person. If this is a shared belief in the wider community (stigmatising) and the person may observe others with a mental health diagnosis being criticised, ridiculed or rejected (they may even learn to treat others in this way). Thus, before ever experiencing depression themselves, the person has already internalised an idea that ‘depression’ is intrinsically wrong in some way and this has potential to be shameful. Once receiving the diagnosis of depression the person may anticipate, or actually experience, negative judgement from others (depending on the degree of stigma related to mental illness in their environment) and therefore fear/experience criticism or ridicule regarding this diagnosis and therefore, based on previous learning, judge themselves negatively. Thus, in keeping with the SRG’s of childhood makes an internal, stable, global/uncontrollable attribution (Lewis, 2007; 2000; Tracy and Robins, 2007a) of sense of self as worthless, eliciting feelings of shame.
A further related point regarding attribution can be extrapolated from the qualitative interviews conducted in this study. During the interviews it was sometimes difficult to distinguish whether the participants themselves were more concerned with fear of external shame or indeed the degree to which the participants observations of what might be formulated as external shame could be formulated as predictive cognitions as to how others may view them, extrapolated from their own negative judgments about self, i.e. ‘I am worthless; therefore, other people will see me as worthless’ or ‘I am worthless therefore others should see me as worthless’. From the perspective of clinical observation some patients with a diagnosis of depression do make this distinction and in CBT, conducting behavioural experiments can at times be powerful in disconfirming predictions that others will criticise, judge and reject them, leading to a change in both perception and behaviour. It is thus important to consider what the formulation of shame as an autobiographical emotional memory, alongside attributional models of depression and shame may add to understanding the clinical manifestation of shame as a psychological facet in persistent treatment resistant depression, alongside Gilbert’s formulation.
In Gilbert’s model (Gilbert and Choden, 2013), using his evolutionary formulation as a spring board, the main target for change is the generation of warmth towards self to ameliorate self-criticism/self-blame and self-hate and to create a state of resting contentment using a range of compassion focused clinical interventions (Gilbert, and Choden 2013; Gilbert, 2010a; 2010b; Gilbert and Irons, 2005). Within this PhD study, an important finding in both in the quantitative and qualitative data is the challenge of self-compassion for this cohort of participants diagnosed with persistent, treatment resistant depression. The SCS did not perform as expected given Neff’s (2003a; 2003b) formulation of self-compassion and in this cohort tapped into the psychopathology of depression (i.e. self-judgment, isolation and overidentification). Similarly, in the qualitative data there was an absence of self-compassion and no participant reported any experiential capacity for self-compassion. The ‘reassured self’ subscale of the FSCSR implicitly refers to the idea of kindness towards self which in the cohort studied in this PhD demonstrated a negative association with the ‘inadequate self’ and ‘hated self’ subs-scales, indicating participants did not endorse highly the positive items the ‘reassured self’ sub-scale. Three participants in the qualitative arm of the study who had been exposed to self-compassion principles either through a course of CBT (participants 16 and 28) or had used self-compassion focused self-help materials (participant 88) reported an intellectual appreciation of the potential benefits of self-compassion. However, each struggled to practice self-compassion and observed that when mood was more depressed any capacity for self-compassion was eradicated. Equally their self-report during the interview at times illustrated the habitual and tacit nature of self-criticism. For some participants, the idea of self-compassion was not only incomprehensible but potentially risky. At the outset of this PhD thesis, Gilbert himself observed that compassion focused treatment interventions are difficult to implement with patients presenting with depression (Gilbert, 2010a). This has been the authors experience in clinical practice over the last eight years when using groupbased compassion focused therapy interventions to work with patients diagnosed with persistent treatment resistant depression. From a Scientist-Practitioner perspective when a specified clinical intervention does not yield efficacious results then the aspects of the clinical presentation which are not amenable to the intervention are identified and questions are posed as to how the clinical intervention may be honed to target these ‘stuck points’.
Based on the findings of this PhD thesis and the clinical experience of its author, a model for understanding shame, self-criticism and absence of self-compassion in patients diagnosed with persistent, treatment resistant depression is proposed. This model, which integrates Gilberts’ biopsychosocial evolutionary approach, research evidence from attributional models of depression and shame and the cognitive science of depression literature is described below. From this the author makes suggestions regarding aspects of the clinical presentation in persistent, treatment resistant depression may be targeted and fruitful areas of further research.
A continuum of shame and self-criticism and absence of self-compassion in persistent, treatment resistant depression
Both the quantitative and qualitative data in this study provide some evidence for the clinical observations made by the author of this thesis and which prompted interest in this area of study, namely, the clinical manifestations of shame and self-criticism and absence of selfcompassion in depression occur in different forms, with varying degrees of scope and intensity of experience. Previous research supports this formulation in the context of selfcriticism. For example, Castilho, Pinto-Gouveia and Duarte, (2015) identified two distinct forms of self-criticism. A style based on inadequacy and feelings of inferiority the function of which is self-improvement and a style driven by self-hate and disgust with the function of punishing, harming or persecuting self. The qualitative data and quantitative data collected in this PhD support this distinction. The data in this PhD study also revealed an absence of self-compassion across a spectrum from an intellectual appreciation of its possibility, through incomprehension of the possibility or purpose of it, to a perception that self-compassion is risky or dangerous. The findings in this PhD study resonate with the work of Kelly and Dupasquier (2016) who found that early experiences of warmth and nurture may influence the degree to which an individual experiences a sense of connectedness, reassurance and safeness in adult social relationships. This was reflected in the accounts of participants childhood environments and sense of self in relation to other which emerged in the qualitative data set in this PhD study. Further, these same feelings influence an individual’s capacity to show self-compassion and receive compassion. These findings are consonant with Gilbert and colleagues research investigating fear of self-compassion (Gilbert, McEwan, Gibbons, Chotai, Duarte and Matos, 2011; Gilbert, McEwan, Matos and Rivis, 2011), that a sense of social safeness is an important mechanism whereby, recollections of parental warmth is related to an individual’s capacity for self-compassion and receipt of compassion.
In this regard shame and self-criticism and absence of self-compassion in persistent, treatment resistant depression can be usefully viewed as existing on a continuum. The formulation of a continuum aims to convey a continuous sequence of clinical features in which the adjacent elements are not necessarily perceptually different from each other, but the anchors are distinct. Further, these differing forms of shame and self-criticism and absence of self-compassion seem to reflect early childhood environments which may shape attachment style, capacity for feeling safe and connectedness in relation to others, alongside an individual’s sense of self and self in the mind of the other. A conceptual model of shame, self-criticism and absence of self-compassion in patients diagnosed with persistent, treatment resistant depression is proposed and represents the integration of the following:
-
The findings from this PhD thesis.
-
Affiliative and emotional processes (Gilbert’s 2017a; 2017b; 2010b) and attributional processes (Bernstein, Evan, Van Bork, Moriarty, et al, 2019; Tracy and Robins, 2007a) framed within an evolutionary biopsychosoical formulation of shame and depression (Gilbert, 2017a; 2017b; 2016; 2007a; 2005a; 2005b; 2001; 1998; Price, Sloman, Gardner, Gilbert and Rohde 1994).
-
established research evidence from the cognitive science of depression: Overgeneral memory and rumination (Williams, Barnhofer, Crane, Herman et al 2007; Spasojevic and Alloy, 2001; Watkins and Teasdale, 2001); autobiographical emotional memories (Matos, Pinto-Gouveia and Costa 2011; Kuyken and Brewin 1995; 1994) thought suppression in depression (Rosebrock, Arditte Hall, Rando, Pineles and Liverant, 2019;
Watkins and Moulds, 2009; Wenzlaff, Rude and West, 2002; Wegner, Schneider, Carter and White, 1987).
-
The authors own clinical observations from using cognitive therapy with patients diagnosed with persistent, treatment resistant depression (Garland, 2016; Garland and Scott, 2008; Moore and Garland, 2003)
In the light of the study findings the potential clinical utility of the proposed conceptual model is explored. This proposed formulation of a continuum of shame, self-criticism and absence of self-compassion is described below and illustrated in diagrammatic form in figure 8.
FIGURE 9: FORMULATION OF A CONTINUUM OF SHAME, SELF-CRITICISM AND ABSENCE OF SELF-COMPASSION IN PERSISTENT TREATMENT RESISTANT DEPRESSION
(*=hypothetical position of each qualitative interview participant on continuum)
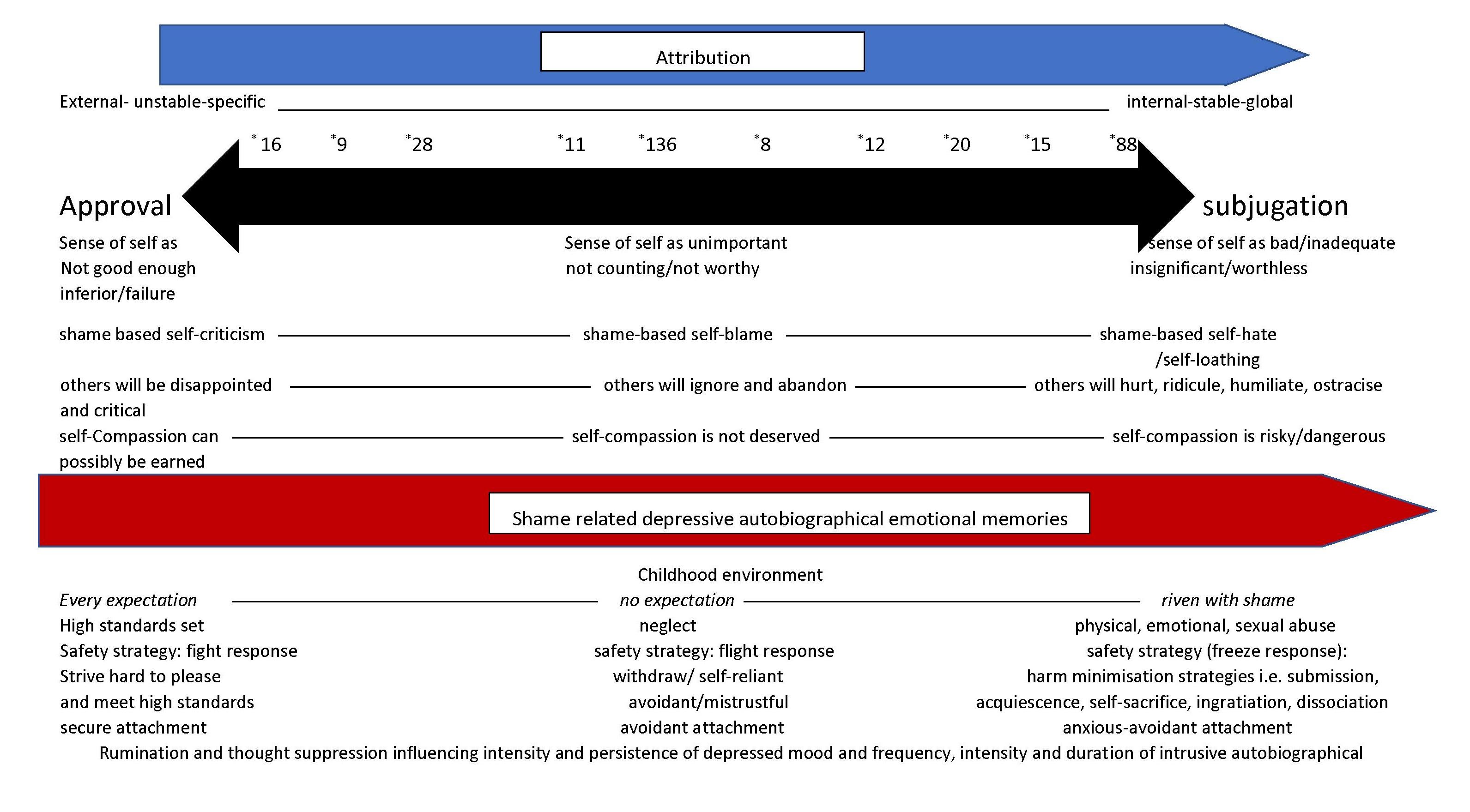
The overall formulation of the model of shame, self-criticism and absence of self-compassion proposed in this thesis is that of a continuum with approval and subjugation as the central anchors. As the continuum progresses the intensity and perseveration of the psychological symptoms external shame (sense of self in the mind of the other) and internal shame (selfcriticism, self-blame, self-hate) and emotional symptoms (shame as a blended emotion: fear, anxiety, anger, sadness and disgust) become more perseverative, internally located, more stable across time and more global in terms of intrapersonal and interpersonal spheres of influence. These constructs of approval and subjugation are well documented in the cognitive therapy clinical literature (Garland, 2016; Kinsella and Garland, 2008; Moore and Garland, 2003; Young, Klosko and Weishaar, 2003; Young, 1990; Beck, rush, Shaw and Emery, 1979). These are also articulated in Gilberts’ formulation of shame (Gilbert, 2017a), in what he terms social motivational systems, namely, the social safeness motivational system, social rank motivational system and compassion motivational system. Embedded within this central continuum of approval-subjugation is a series of further continuua as follows:
-
Sense of self as an attribution (Bernstein, Evan, Van Bork, Moriarty et al, 2019; Tracy and Robins,2007a)
-
Sense of self-in relation to others and attachment style (Matos, Pinto-Gouveia and Costa, 2013)
-
Shame as a blended emotion: fear, anxiety, sadness, anger, guilt, disgust (Gilbert and Choden, 2011; Gilbert, 2007a; 1998; Kaufman, 1989)
-
Shame focused depressive autobiographical emotional memories (Matos and PintoGouveia 2010)
-
shame-based self-criticism or self-blame or self-hate/self-loathing (Castilho, PintoGouveia and Duarte, 2015)
-
Absence of self-compassion
-
The proposed model also considers the severity of depressed mood and rumination, over general memory and thought suppression and dissociation as emotional regulation strategies in the context of childhood trauma ((Matos, Pinto-Gouveia and Costa, 2012).
The continuum (see figure 9 for a diagrammatic representation) is articulated as follows.
Approval is defined in the context of Gilbert’s evolutionary perspective which posits that humans possess social motives which arise from strategies aimed at maximising the chances of survival and reproduction. These motives shape phenotypes which are consonant with the environments from which they emerge (Gilbert, 2017a). This evolutionary perspective has at its heart Attachment Theory (Bowlby 1973/1969) which posits that, from an evolutionary perspective, humans are born defenceless and as a result prepossess a range of attachment behaviours that enable them to maintain connection with attachment figures in order to access care, protection, support and assistance with emotional regulation (Gilbert, 2017a).
Attachment theory as described by Mikulincer, Shaver, Gillath and Nitzberg, (2005) posits three attachment styles as follows. Attachment avoidance, which reflects the degree to which an individual distrusts other and therefore maintains behavioural independence and emotional distance and is more wary of both the giving and receipt of care. The second is attachment anxiety where the individual worries about the degree to which others will be available if needs be, where there is a preoccupation with the receipt of care. The third is secure attachment which reflects a capacity to trust others and to share reciprocity in terms of the giving and receipt of care. From this starting point (as outlined in chapter 2 of this thesis) Gilbert argues that as humans we have evolved as social beings for whom attachment to others is an intrinsic aspect of survival (Gilbert, 2017a; 2017b; 2009; 2007a; 2005a; 2005b; 2000; 1998; 1992). Thus, for us as human beings, a primary concern is ‘sense of self in relation to other’ (Gilbert, 2007a), an aspect of which is an intrinsic need for approval from others. This need for approval is governed by three social motivational systems. These are the social safeness motivational system which creates a sense of social safeness for the growing child in which significant others provide care, nurture and validation. This instils a sense of self as having worth and lovability and where this is present then the child experiences emotional warmth and positive affect towards self and others. This system in turn facilities cooperative and affiliative relationships with others (secure attachment). However, if a child is raised in an environment where this nurture and care is not available and rather than conveying warmth, significant others exhibit threat, hostility and shaming towards the child then this sense of safeness is lost or absent. As a result, not only is emotional warmth and positive affect towards self and others dampened, but the threat system becomes amplified which may trigger anger/fight, anxiety/flight, submission and appeasement and/or anxious clinging (Gilbert, 2005b). In such an environment the social rank motivational system dominates.
The social rank motivational system is defined as our concern for our position in a social rank
i.e. are we viewed and treated by others as equal, inferior, or superior (Gilbert, 2007a; Gilbert, 1998; Gilbert and McGuire, 1998). It is from this system, working in conjunction our ability to be self-aware, that our capacity to experience a sense of external and internal shame has evolved (Gilbert, 2017a). Thus, as human beings we are sensitive to unfavourable social comparison and the potential negative judgment of others, alongside the fear of rejection, ostracism and attack. Thus, for Gilbert shame is not an emotion in its own right but a blended emotion comprising anxiety, anger, disgust and sadness, alongside the emergence of defeat related behaviours and depressed mood (Gilbert, 2007a; 1998). Thus, in the social rank motivational system, the child is acutely aware of the power of others and to their potential for harm or neglect or abandonment. It is in this context, according to Gilbert (with reference to Bowlby 1973/1969), that internal shame emerges as a defensive strategy deployed by the child to reduce the danger of attack from and maintain attachment with the stronger, more powerful significant other. Thus, in such a threat focused environment, the child assumes responsibility (self-blame) for the care givers anger and hostility and for keeping interactions safe. A sense of safety may be achieved by becoming excessively appeasing and submissive in the face of threat or when in need of help and support, all the while living in a state of fear that they may do something wrong resulting in anger, punishment and rejection from the significant other. In extremis this emerges as a subjugated position which compromises the individual’s autonomy in which there is no sense of their own rights, needs and wants, leading to perceptions of powerlessness and lack of control.
Thirdly the compassion motivational system is formulated as an evolved motive and intention to pay heed to suffering in self and others. This the motivation is to acknowledge the suffering in the world at large and to act with the intention to alleviate both our own and the suffering of others (Gilbert, 2017a). This requires both empathy and intersubjectivity (see chapter 2 for a more detailed description).
Defining the parameters of approval and subjugation
In defining the parameters of the continuum, three broad themes emerged from the data collected in this PhD study. These will be described below with reference to the embedded continuua described above. Taking and evolutionary perspective, the interplay between organism and environment is the crucial factor in the emergence of phenotypes and for Gilbert environment is primary in the onset of depression. In keeping with this formulation, the descriptors for the themes identified in this formulation refer to the environments described by the participants interviewed in this study. All ten participants interviewed as part of this PhD study spontaneously referred to their childhood environments and their relationships with care givers and significant others in the community i.e. teachers, as important in terms of how they viewed self and self in relation to others and their experience of depression and anxiety disorders.
Shame of not meeting expectation: Every expectation
At the approval anchor of this formulation of shame, self-criticism and absence of selfcompassion, sense of self is expressed as a not good enough/inferior/failure and sense of self being held as a disappointment in the mind of the other for having not met expectation (external shame) and therefore have potential to be critical (see participants 9, 16 and 28 citations in chapter 5 of this thesis). Thus, approval from others is contingent upon meeting expectation. There is an absence of global condemnation of self and more a focus on behaviours which signify ‘not meeting the mark’ (see citations from study participants, chapter 5, pp. 198–200). It might be anticipated that pride can be experienced if expectations are met and praise and reward is forthcoming from significant others when expectations are met. Formulating shame as a blended emotion, key emotions in this domain are anxiety and sadness which are transient in the context of specific experiences or situations. There is an absence of anger towards self and others and more impatience and exasperation towards self that is situation or behaviour specific. There is capacity for anger at others to be expressed when appropriate and importantly individuals have a sense of what their own rights, needs and wants are in a situation and can to a greater or lesser extent have these met in the context of mutually affirming and supportive relationships.
The authors clinical experience of working with depression would suggest that in this domain of the continuum intrusive depressive autobiographical emotional memories are limited to one or two specific examples which are discrete, located in a specific time and place and only emerge when mood is depressed. In addition, the individual has a significant cache of pleasant, affirmative, nurturing autobiographical memories associated with feelings of warmth and safeness, contentedness and joy available to them which are present when mood is less or not depressed.
Internal shame is manifest as situation specific self-criticism associated with a perception of not meeting expectations. This was reflected in participants use of the terms ‘should’ and ‘could’, whereby the respondent identified a discrepancy between how they perceived they had performed in a certain context and how they perceived they should have performed i.e. the standards they perceive they ‘should’ or ‘could’ have met (see citations from study participants chapter 5, pp. 198–200). The use of the term ‘should’ evoke a sense of obligation, duty or correctness. The term ‘could’ conveys the idea of degrees of possibility of what might be done or achieved (see participant citations, chapter 5, pp. 193–194 and 224) and for participants 9, 16 and 28 there was a sense the fuel for self-criticism was a perception of having failed through some act of omission i.e. ‘not trying hard enough’. In this context voice tone takes a chastising stance with a sense of exasperation and disappointment at self, but with the aim of admonishing self. Self-criticism serves a purpose of improving performance (see citations from study participants chapter 5, p. 200). Behaviours manifest in this domain are associated with a fight response. This may manifest as striving to achieve a certain standard which may evoke feelings of pride if approximated. Within this domain of the spectrum there is a conditionality to self-compassion, this may be earned if sufficient effort is made.
In childhood environments (i.e. home, school, community) in this domain of the continuum, there may be an imperative to perform to a certain standard or to meet a certain set of expectations. Behaviourally there is a sense in which the individually continually strives to achieve a particular standard. For example, participants 9, 16 and 28 described varying degrees of a sense of self as ‘not having met the mark’ and thus in some way felt they ran the risk of disappointing significant others or being viewed as less than in some way. Their sense of self was shaped by this, evoking a sense of shame if expectations were not met. At the approval end of the continuum attachments are likely to be secure. In the interviews in this PhD study participants 9, 16 and 28 reported and displayed behaviours consonant with secure attachment. That is, a working alliance was quickly formed in the interview, questions were engaged with and pondered over and there were reciprocal exchanges of warmth and humour, conveying a sense of safety. Childhood was spoken of in a way that conveyed parental care, nurture and support was present. Each participant described a current friendship group, had engaged in long term romantic relationships and had worked in a profession (engineering, nursing, dietetics).
Shame, ridicule and humiliation: No expectation
At the midway anchor on the proposed approval-subjugation continuum sense of self is formulated as unimportant/not counting/not worthy and a sense of self as not being held at all in the mind of the other i.e. ‘out of sight is out of mind’ (external shame) (participants 8, 12, and 136). This idiom ‘out of sight is out of mind’ conveys a sense that people who are no longer visible or present are soon forgotten (Ayto, 2010, p 316) (see citations from study participants in chapter 5, pp. 200–205). With this emerges a sense of never being in receipt of care, praise, love or encouragement and occupying a subjugated position in this regard. Subjugation in this domain of the continuum can be defined as the act of treating a person or their rights and needs and wishes as less important than other people or their rights, needs and wishes or the person and their rights, needs and wishes not counting at all. Formulating shame as a blended emotion, key emotions in this domain are fear (as opposed to anxiety), anger at self and others and sadness with experiential avoidance being a central coping strategy. A greater number of depressive autobiographical emotional memories associated with fear, anger and sadness are accessible which operate across time, place and person and are therefore more pervasive in their impact. These are potentially present most of the time and become amplified when mood is depressed. There are possibly fewer pleasant, affirmative, nurturing autobiographical memories associated with feelings of warmth and safeness, contentedness and joy available to them.
In this domain of the continuum internal shame is dominated by a dialogue of self-blame ‘it’s my fault’ which is subjectively more insidious in its manifestation than the self-criticism at the approval end of the continuum. In this domain the finger of blame has been turned upon self, expressed as a sense that the individual themselves, by acts of omission or commission, is responsible for causing others to behave towards them in a particular i.e. their own childhood adversity and maltreatment. For example participant 8 (see citation chapter 5, p.192) in discussing how his parents treated him as a child drew responsibility away from his parents and attributing the problem to his own personality and participant 12 ‘it was all my fault’ (see citations chapter 5 , p227-228). There is a sense of the importance of ‘knowing your place’ and a fear non-compliance will result in punishment. The idiom ‘knowing your place’ is defined as:
‘to accept your position within society, an organisation, your family etc. and to not want to
improve it’
Cambridge Dictionary (Cambridge University Press, 2020).
Within the interviews conducted in this PhD study a degree of subjugation and ‘knowing your place’ was described. For example, always prioritising the needs of others (participant 12), never expressing an opinion (participant 136) and ridiculing self-deprecation (participant 8).
In this context voice tone towards self is impatient, with a self-deprecating, mocking stance towards self. This was apparent throughout the interviews with participant 8, who spoke continuously and participant 136 who gave short, clipped answers (see participant citations in chapter 5, pp. 204–205). There is also degree of hostility and contempt directed not only at self but at others too. For example, participant 136, when discussing experiencing panic attacks in public, displayed hostility in his voice tone towards others for what he deemed their judgement of him and ignoring him i.e. not helping. Self-blame serves the purpose of maintaining the safety of ‘knowing your place’ and not lifting their head over the parapet for fear of being physically or psychologically attacked.
Behaviours manifest this domain are associated with a flight response. This includes withdrawal from and avoidance of others and self-reliance as a safety strategy. There is also a sense of helplessness in which striving to achieve or change circumstances is experienced as futile and therefore not attempted and is associated with a sense of resigned defeat. Selfcompassion as a concept is beyond comprehension in terms of possibility and utility.
Childhood environments (both at home, school and the wider community) in this domain of the continuum are likely to be characterised by a combination an absence of emotional care and nurture and the deliberate instilling of fear using a combination of physical punishment and ridicule and humiliation with a philosophy of ‘spare the rod, spoil the child’. This idiom conveys the idea that a child requires punishment (physical or psychological) when they do wrong to ensure appropriate moral and social development and strength of character.
Punishment in this form is an act of physical and psychological subjugation of the child by the adult and was reflected in the accounts of the participants in the qualitative part of this PhD study. Participants 8, 12 and 136 described an absence of connectedness to care givers and no expectations from care givers and school regarding care and nurture, achievement, or life goals and as children, they recalled being left to their own devices without adult supervision. For example, the account from participant 136 about how he was parented (chapter 5 , p. 192) and the emotional memory recalled by participant 8 of being verbally put down and dismissed with a ridiculing tone when he told his father he could count to ten in French ( chapter 5 p. 191). At the time of the interview participant 8 had never worked in paid employment and had been an unpaid carer most of her life. Participant 12 worked as a parttime taxi driver and participant 136 worked as a storeman. This description illustrates the social rank motivational system and its mode of function at both macro and micro levels (i.e. society, organisation, family, friendship group etc). In this context these three participants were raised within a working-class environment. Demarcations of class can be formulated as an aspect of social rank and in this regard this sub-group of participants would be deemed to exist at the lower end of such a rank.
Participants in this sub- group reported and displayed behaviours consonant with an avoidant attachment style. It was hard to establish a sufficiently consistent emotional connection in the interview to form a working alliance and avoidant and submissive safety strategies interfered with the flow of conversation. For example, participant 136 was very guarded in answering questions, often gave monosyllabic answers and was deferential in his manner, not engaging at an emotional level throughout the interview. Participant 8 was garrulous in his conversational style and emotionally avoidant. Even on occasions when he became tearful in the interview he quickly deflected to a different focus whilst dismissing his own distress. Participant 12 was deferential throughout the interview apologising profusely when she began to cry whilst describing the emotional and physical abuse perpetrated against her by her father.
Riven with shame: trapped and defeated
At the subjugation anchor of the continuum sense of self is expressed as bad/inadequate/insignificant/worthless and sense of self one of being held in contempt, derision and disgust in the mind of the other (external shame). Thus, there is anticipation of harm, ridicule, humiliation, punishment and ostracism from others (see participant citations in chapter 5, pp. 205–211). Internal shame is manifest as self-hate and self-loathing and is a combination of self-blame and a pernicious self-punishing form of self-criticism which has a visceral quality in terms of its subjective experience and overt manifestation. There is anger towards self and a notable absence of anger towards others. This represents an internal, stable, global condemnation of self that operates across time, place and person and has been present since childhood. The individual views self as in some way objectionable, not just in terms of behaviour but in terms of their very self (this is articulated vividly by participant 88 in her description of her own self-loathing, chapter 5, p 206) and not only anticipates but believes, others should hold them with the same degree of antipathy and loathing. In this context voice tone is angry at and contemptuous of self, with an air of repugnance at self.
This manifest in the form of the ‘inner bully’, a concept referred to in Gilbert’s clinical writing (Gilbert and Choden, 2013; Gilbert, 2010a). ‘Bullying’ can be defined as a process by which a person deliberately intimidates or is cruel to a weaker person. This bullying internal dialogue often turns the person against themselves in the form of self-subjugation, as they may perceive particular aspects of self as indicative of ‘badness’ or ‘weakness’.
From the authors own clinical experience this point is exemplified by (but not exclusive to) patients’ descriptions of the visceral level of repugnance they feel toward their own body which they must inhabit and therefore, by default, their own self in the context of childhood sexual abuse. Participant 88 described and then experienced this in vivo in her interview in this study (see citation chapter 5, p 206). This self-hate/self-loathing is often closely aligned to self-condemnation on moral grounds and is manifest across situations and has the capacity to take on a persistent, pervasive, ruminative tone.
Formulating shame as a blended emotion, key emotions in this domain are fear (as opposed to anxiety), anger (at self), guilt, disgust and sadness with experiential avoidance and dissociation being central coping strategies. A greater number of depressive autobiographical emotional memories associated with fear, anger, guilt, disgust and sadness are readily accessible on a daily basis. These operate across time, place and person and are therefore more pervasive in their impact becoming amplified in extremis when mood is depressed. There are very few or no, pleasant, affirmative, nurturing autobiographical memories associated with feelings of warmth and safeness, connectedness and joy available to them. Combining this predominance of depressive autobiographical emotional memories with the internal, global, stable attributions about self and self in relation to others, this manifests as a felt sense (Teasdale, 1999), an ever present visceral experience of being ashamed of who or what you perceive yourself to be. Behaviours manifest in this domain of the continuum are associated with a freeze response. These include submission, self-sacrifice, acquiescence, clinging, ingratiation and dissociation. These engender an intense sense of fear of others, powerlessness and inert defeat ( i.e. see citation from participant 88, describing how her father gained her submission and compliance chapter 5 ,p 195–196) and in the extreme, a subjugated sense of self that does not exist in its own right. In this domain self-compassion is risky or dangerous as it involves letting your guard down, which has potential to leave you vulnerable to harm or attack and thus triggers fear. Further, in extremis, such is the level of self-hate that kindness, (towards self and from others), rather than alleviate can amplify selfdisgust.
From the qualitative data collected in this PhD study participants (11, 15, 20 and 88) who fell under this domain of the continuum exhibited a range of behaviours that Gilbert would cite as markers for high levels of shame being activated (Gilbert, 2010a). These include, high levels of cognitive, emotional and behavioural avoidance (participants 11 and 15), changing the focus of discussion when difficult topics arise (participants 15, 20), disorganisation of thought processes and language (participants 11, 15, 20 and 88), freezing during conversation (participant 11) and averting of gaze when disclosing perceived shameful (participants 11, 15, 20 and 88). Examples from the qualitative data collected in this PhD study can be found in chapter 5, pp. 196 and 211–212).
The childhood environments (i.e. home, school, community) in this domain of the continuum are marked by sustained and significant trauma in the form of childhood sexual abuse (participant 88), bullying by peers and teachers regarding a stammer (participant 20), (likely although not overtly articulated) racial discrimination and harassment (participant 11) and physical abuse (participant 15). Such environments engender experiences founded in powerlessness and a sense of helplessness, hopelessness and absence of control, engendering a defeated position. This in turn may increase the likelihood of shame based attributions about self and self in relation to others becoming more dominant (c.f. Tracy and Robins, 2007a).
In the interviews in this PhD study participants 11, 15, 20 and 88 reported and displayed behaviours consonant with an anxious-avoidant attachment style. Each displayed selfconsciousness in the room and at times, their antipathy towards themselves as they interacted in the interview had to be navigated as part of the conversation. Participant 88 was very ingratiating, compliant and acquiescent with the interviewer, as reflected in the degree of unsolicited self-disclosure she gave in the interview (see citation chapter 5, p 195–196). Meanwhile, participant 11 was reserved and cautious as if screening her answers before replying to the interviewer’s enquiries, as exemplified in the citation in chapter 5, pp. 196197) where she refers to going back in her own mind in the interview to childhood but does not disclose the content of the recollection to the interviewer. Participant 15 was guarded in the interview and managed this by going on the offensive, speaking constantly, diverting the conversation at certain points, possibly with the aim of keeping the interviewer at arm’s length (see citation in chapter 5, p. 197). Participant 20 spoke with candour about his feelings of anger at self, fear of others and self-disgust resulting from the sustained bullying to which he was subjected and his sense of powerlessness and defeat (see citation in chapter 5, p 207).
.
Clinical implications of these findings and avenues for future research
As is evidenced in the demographic data of the cohort studied in this PhD thesis, this clinical population is complex and difficult to treat. The model described above proposes several aspects of the clinical presentation of persistent, treatment resistant depression which may be more proactively targeted as part of a psychological intervention which integrates the principles and practices of CBT and CFT as follows.
In considering the approval anchor of the continuum it is proposed that standard cognitivebehavioural treatment interventions (i.e. activity scheduling and graded task assignment, identifying and modifying negative automatic thoughts with behavioural experiments, modifying conditional beliefs) are highly effective (Kinsella and Garland, 2008) at ameliorating depressive symptoms. Further, it is in the first third of the continuum that the self-compassion interventions proposed by Gilbert and colleagues (Gilbert and Choden 2013; Germer, 2009; Gilbert and Procter, 2006; Gilbert and Irons, 2005) are most readily implemented, where a negative view of self, self-criticism and attendant shame based emotional memories are circumscribed and there are warm and affirming emotional memories from childhood which can be drawn on in using compassion focused interventions. There is an intellectual appreciation of the possibility self-compassion. In this regard an integration of CBT and compassion focused therapy interventions delivered in a group format may be of clinical utility.
Once the territory of the second two thirds of the continuum is entered and sense of self as unimportant/not counting/not worthy and bad/ inadequate/ insignificant/worthless is present both cognitive-behavioural and compassion focused interventions become more difficult to implement. In the group-based treatment implemented by the author of this PhD thesis a consistent theme among patients falling into these domains is an inability to act as if they matter in the way they relate to both self and others. This is subjugation in action and indeed their self-blaming and self-hating stance is used against themselves to subjugate self even further and impacts on therapy itself.
What was striking about the cohort recruited to this study, (in which this PhD author acted as a psychotherapist delivering CBT treatment) was the scope and severity of childhood trauma disclosed by the participants in the course of therapy and how these experiences resonated in the here and now in their daily lives. This was most apparent in their sense of self in the mind of the other, including the therapist. This is reflected in the accounts of their childhood environments shared by the participants in the qualitative arm of this PhD study.
A significant clinical reflection from working with this cohort of patients diagnosed with persistent, treatment resistant depression was that a key aspect of therapy was facilitating a process of speaking about childhood experiences. This frequently involved part of the therapist’s role as both bearing witness to and validating testimony to a life story filled with immense sorrow, tragedy and unfathomable cruelty. This was often immensely challenging for the patient (and therapist) and it is in this domain that experiential avoidance strategies were most apparent, both in the telling of their childhood, in their attachment and interaction in treatment sessions and their approach to using both CBT and CFT interventions.
Here it is proposed that shame based autobiographical emotional memories are present, where, if shame is formulated as a composite emotion, then, in persistent, treatment resistant depression the key emotions embodied in the shame memory are unregulated fear and sadness. These are subjectively experienced as highly aversive and are therefore managed using experiential avoidance strategies established in childhood which unintentionally amplify depressed mood. These are over-general memory, rumination and thought suppression. This may be a reflection that effective skills in affect regulation have never been developed in childhood, as is posited in Gilberts model (Gilbert and Procter, 2006) and by Williams in his formulation of the relationship between over general memory and rumination (Williams, Barnhofer, Crane, Herman, Raes, Watkins, and Dalgleish, 2007).
Taking these factors into consideration the following are proposed as targets for intervention:
1. Validation through life story work and the marking and mourning of losses.
2. Working with unresolved grief from childhood.
3. ‘Acting like I matter’- tackling subjugation of self by self (‘self-attack’) and self by others.
4. Emotion focused interventions targeting fear and sadness and generation of more adaptive emotional state i.e. pride (Greenberg and Pascual-Leone, (2006)).
5. Working with shame based autobiographical emotional memories (Brewin, Wheatley, Patel, Fearon, Hackmann, Wells and Myers, (2009)) and targeting emotional ‘hot spots’ to change attribution and meaning (Grey, Holmes and Brewin (2001)).
6. Development of specific interventions to target self-criticism, self-blame and selfhate/self-loathing (Castilho, Pinto-Gouveia and Duarte, (2015)).
With regards to future research with patients diagnosed with persistent, treatment resistant depression further investigation and differentiation of the form and function of self-criticism, self-blame and self-hate in this population would be a useful preliminary step to developing more targeted clinical interventions for these phenomena. There are already in existence protocols for working with intrusive depressive memories (Brewin, Wheatley, Patel, Fearon, Hackmann, Wells and Myers, (2009) which interestingly have not garnered much uptake among CBT practitioners. This may be explained by the fact, borne out by the experience of the author of this thesis, that engaging the patient in this intervention is challenging. This may reflect the fact that emotional memories arising from the types of childhood trauma exemplified by the participants in the qualitative arm of this study are not single incident events located at a particular developmental stage and therefore amenable to rescripting as the protocol describes. Rather, these are composite emotional memories of learning to survive in a particular environment with its myriad of toxicities across developmental stages which fundamentally shape sense of self and self in relation to other (Conway, 2005). What lies beneath these emotional memories is unregulated fear and sadness which is managed using the tacit experiential avoidance strategies, which emerge in the face of childhood trauma, namely over general memory, rumination and thought suppression. In this regard testing interventions, which aim to facilitate emotional regulation of fear and sadness in persistent, treatment resistant depression may be of benefit. This may require a more stepwise approach to combine narrative, emotion focused interventions to process and regulate fear and sadness, alongside already established evidence-based interventions (i.e. CBT and MBCT). This also raises the issue of models of service delivery and the value of specialised services for patients with persistent, treatment resistant depression in meeting complex needs (Morriss, Garland, Nixon, Boliang Guo, 2016).
Strengths of this study
A major strength of this study was the cohort of participants recruited. In terms of sample size (n=187), gender distribution and severity and recurrence of depression, the sample is representative of patient cohorts recruited in other studies of depression. However, the current study cohort not only had significantly higher rates of depressive symptomatology (e.g. melancholia) but also higher levels of comorbidity for both psychiatric and physical health problems (see tables 6 and 7 in chapter 4 p 135–136) and Star*D study, Rush, Madhukar, Trivedi, Wisniewski, Nierenberg, Stewart, Warden, Thase, Lavori, Lebowitz, McGrath, Rosenbaum, Sackheim, Kupfer, Luther and Fava 2006). With regards to co-morbid anxiety disorders and gender distribution, this sample is similar to that reported by the 2007 household Survey of Adult Psychiatric Morbidity in England. The baseline demographic characteristics are similar to those reported in other studies. For example the CoBalT depression trial (Wiles, Thomas, Abel, Ridgway, Turner, Campbell, Garland, Hollinghurst,
Jerrom, Kessler, Kuyken, Morrison, Turner, Williams, Peters and Lewis 2013) report similar baseline demographic characteristics for age, gender and relationship status in a cohort of participants diagnosed with treatment resistant depression treated in primary care. However, in the current study the cohort were less likely to be in full-time employment (22.5%: 46.1%) but reported a higher level of attainment of educational qualifications (before age 16 5%:
22.9%).
Further, this PhD study is the first to test the OAS, FSCSR and SCS on a clinical cohort with such severity and persistence of depressive symptomatology, with significant co-morbidity for both anxiety disorders and physical health conditions. As Kim, Thibodeau and Jorgensen, (2011) concede in their concluding comments to their metanalytic review of shame, guilt and depressive symptoms, their findings are most relevant to self-reported depressive symptoms in a sub-clinical range. This cannot be said of this sample.
A further strength of this study is the convergent parallel mixed methods design (Cresswell and Plano-Clark (2011)) and its framing within the Pragmatism paradigm (Biesta, 2010) embedded within the Scientist-Practitioner model (Salkovskis, 2002). Clinical practice is an art, a science and a craft (Callaghan and Butler, 2017; James, Morse and Howarth, 2010) and the mixed methods approach embodies both of these forms of knowledge and endeavour. This PhD has at its heart improving patient care for those who suffer with persistent, treatment resistant depression and the strength of this thesis is its origins in the primacy of praxis. It is the authors view that research that collates and gives equal weight to both forms of data, numbers and words (Biesta, (2010)), enables a more ethical, collaborative endeavour between clinicians and researchers and the patients whose best interests they are employed to serve. Enshrined within CBT is the principle of collaboration, working together as a team. This collaborative stance is predicated on the idea that the patient brings their expertise regarding their own struggles and suffering to the therapy endeavour and the clinician, their knowledge and skill in using CBT treatment strategies, with the aim of working together to try and alleviate that suffering. The mixed methods research design has capacity to promote inclusion and empowerment for patients and for them to actively participate in the design, development and testing of psychological therapies (see Simpson, Jones, Barlow, Cox and Service User and Carer Group Advising on Research (SUGAR) (2014).
Limitations of this study
There are several limitations to this study. Notably the omission in one study site to administer the OAS (n=29), alongside 10 participants either failing or refusing to complete the OAS at baseline, which resulted in a smaller sample size for testing the psychometric properties of the OAS (n=148). Similarly, 10 and 8 participants respectively either failed or refused to complete the FSCSR and the SCS. This has implications for the statistical results and their interpretation. In addition, it can be argued the sample size (n=187) is lower than the recommend sample size of a minimum of 200 participants (see Frost, Reeve, Liepa, Stauffer, Hays and the Mayo/FDA Patient-Reported Outcomes Consensus Meeting Group (2007)) for testing reliability and validity of self-reported measures. This may have implications in terms of some of the analysis of validity and the weak associations between items and sub-scales found in some of the quantitative data analysis. Given the observation above regarding the reduced sample size of the OAS, this limitation is particularly relevant with regards to the sample size on which the OAS was tested.
A further limitation that arose was observed by the research associates who collected the quantitative data for this PhD study who reported that for some participants, the OAS, FSCSR and SCS were distressing to complete. This is reflected in the missing data and may have impacted upon how participants engaged with completing the measures. Equally, when interpreting data, the potential impact of respondent fatigue in completing psychometric tests which are long, (i.e. SCS is 26 items) and require concentration to decipher meaning, is important to take into consideration. In this cohort the depressive symptoms the participants experience (i.e. reduced concentration, reduced abstracting ability, tiredness, irritability) are likely to impact further not only on their ability to complete questionnaires, but their capacity to show diligence in so doing and this needs to be considered in interpreting the results. It is also important to note that the mood dependent processing biases cited in this PhD (for a summary see Harvey, Watkins, Mansell and Shafran 2004) may influence how psychometric measures are completed by respondents.
The size of healthy control sample is not equal to that of the clinical cohort studied here, which was used to test how the OAS, FSCSR and SCS performed when administered to a group of healthy controls. As summarised by Jones, Carley and Harrison (2003), power and sample size estimations are used in research to determine how many participants are needed to answer a research question. This small sample size (n=33) of healthy controls, in comparison to the clinical cohort (n=187), reduces the statistical power of the comparison as a small sample size increases the chances of a false positive or false negative result occurring (Jones, Carley and Harrison 2003).
The use of the SCS as a measure of self-compassion was a limitation in two ways. Firstly, it does not formulate self-compassion within the same theoretical frame as Gilbert (Gilbert and Choden, 2013). At the commencement of this PhD thesis and in consultation with Paul Gilbert the SCS was identified as the only available measure of self-compassion. Subsequently Gilbert and colleagues (Gilbert, McEwan, Matos, and Rivis, 2011) have developed the Fear of
Compassion Scale which is consonant with Gilbert’s underlying theory of self-compassion. This scale aims to assess fear of expressing compassion for others, fear of responding to compassion from others and fear of expressing kindness and compassion towards yourself. This measure, had it been available, would have been more appropriate than the SCS to test in this PhD study. Also, it may have yielded quantitative data to support the qualitative findings regarding an overall absence of self-compassion and the perceived potential risks and dangers of self-compassion in a cohort of patients diagnosed with persistent, treatment resistant depression.
Conclusion
The quantitative analysis in this thesis suggests the OAS (a measure of external shame) and the FSCSR (a measure of internal shame) are reliable and valid measures when tested on a cohort of participants diagnosed with persistent, treatment resistant depression. Further, both the quantitative and qualitative results provide evidence to support the formulation of shame tested in this thesis, and the presence of an interrelated, but differentiated relationship between external and internal shame in this population. One sub-scale of the OAS, emptiness did not perform as well in the cohort studied, as evidenced in both forms of data collected. On this basis it is proposed that emptiness as a construct is not central in the formulation of external shame in persistent, treatment resistant depression and it is suggested a revision is made to the OAS, incorporate a construct measuring worthlessness.
In addition, within this PhD study the validity of these measures overtime and in treatment was not explored and this would be an important to pursue in future research.
Meanwhile, whilst the SCS demonstrated reliability, it did not prove to be a valid measure in the population under investigation. Rather, the SCS showed poor discriminant validity as indicated by the very strong correlations between the both the negative sub-scales (selfjudgement, isolation and overidentification) and the positive sub-scales, (self-kindness, common humanity and mindfulness). Thus, in a cohort of patients diagnosed with persistent, treatment resistant depression, the findings in this thesis do not support the theoretical formulation of self-compassion which underpins the SCS. Further, examining the quantitative and qualitative data in unison it is proposed that, in this population, the SCS actually taps into the psychopathology which characterises depression ( i.e. self-criticism, social withdrawal, rumination) and in this regard lacks theoretical and conceptual veracity as a measure of selfcompassion.
An interesting and unexpected finding in this PhD thesis was that in the quantitative data analysis levels of shame and self-criticism did not appear to be a function of severity of depression but appeared to be more stable psychological constructs. However, the qualitative data did reveal evidence to support a relationship between severity of mood and frequency and intensity of self-criticism and feelings of shame. In addition, both forms of data collected in this thesis highlight the importance of attribution in depression and shame and in this regard, it is proposed consideration is given to an integration of attributional models of depression and shame, within an evolutionary psychobiosocial framework.
On this basis a model is proposed in which It is hypothesised that, in formulating shame and self-criticism as psychological constructs linked to childhood environment, these exist on a continuum, central to which are attributions related to approval and subjugation. Continuua of external shame (childhood environment) and internal shame (self-criticism-self-blameselfhate/self-loathing) are embedded within this approval-subjugation continuum. The model takes into consideration the cognitive science of depression, specifically, the presence of intrusive, autobiographical, shame based emotional memories in depression and the role of rumination, thought suppression and dissociation, as affect regulation strategies. It is proposed these memories, linked to childhood trauma, are important in the maintenance of persistent, treatment resistant depression. These affect regulation strategies are aimed at managing the intrusive nature of such memories (which are amplified the more depressed mood becomes) and associated emotions (fear, sadness, anger, disgust of which shame as an emotion is a composite) but which are, in fact counterproductive, as they exacerbate rather than alleviate these emotions and ultimately depressed mood. The data derived from this study extends clinical knowledge of the phenomenology of shame, self-criticism and selfcompassion in a cohort of patients diagnosed with persistent treatment resistant depression. In addition, these inductive findings provide an opportunity for the testing of the proposed model and the development and testing of clinical interventions when working with shame and self-criticism in persistent, treatment resistant depression.
References
Abramson, L.Y. and Sackheim, H.A. (1977) A paradox in depression: uncontrollability and selfblame. Psychological Bulletin, 84 (5): pp. 838–851.
Abramson, L. Y., Seligman, M. E. P. and Teasdale, J. D. (1978) Learned helplessness in humans: Critique and reformulation. Journal of Abnormal Psychology (87): 49–74.
Aguinis, H., Gottfredson, R.K. and Joo, H. (2013) Best-practice recommendations for defining, identifying and handling outliers. Organizational Research Methods 16 (2) pp. 270–301.
Allan, S., Gilbert, P. and Goss, K. (1994) An exploration of shame measures-II: Psychopathology. Personality and Individual Differences (17): 719–722.
Alloy, L. B., Abramson, L. Y., Hogan, M. E., Whitehouse, W. G., Rose, D. T., Robinson, M. S., Kim, R. S. and Lapkin, J. B. (2000) The Temple-Wisconsin Cognitive Vulnerability to Depression Project: Lifetime history of Axis I psychopathology in individuals at high and low cognitive risk for depression. Journal of Abnormal Psychology 109 (3): pp. 403–418. Available at: https://doi.org/10.1037/0021-843X.109.3.403 (Accessed 16th September 2019).
Alloy, L.B., Abramson, L.Y., Smith, J.M., Gibb, B.E. and Neeren E.M. (2006) The Role of Parenting and Maltreatment Histories in Unipolar and Bipolar Mood Disorders: Mediation by Cognitive Vulnerability to Depression. Clinical Child and Family Psychology Review 9 (1): Available at: DOI: 10.1007/s10567-006-0002 (Accessed 9th January 2020).
American Psychiatric Association (2013) Diagnostic and Statistical Manual (5th ed.). (DSM-5): Arlington, VA: American Psychiatric Association.
American Psychiatric Association (1994) Diagnostic and Statistical Manual (4th ed.). (DSMIV): Arlington, VA: American Psychiatric Association.
Amital, D., Fostick, L., Silberman, A., Beckman, M. and Spivak, B. (2008) Serious life events among resistant and non-resistant MDD patients. Journal of Affective Disorders 110 (3): pp. 260–264.
Andrews, B. (1998) Shame and childhood abuse. In: P. Gilbert, P. and Andrews, B. (Eds.) Shame: Interpersonal Behaviour, Psychopathology and Culture. Oxford: Oxford University Press, PP. 176–190.
Andrews, B., Qian, M., and Valentine, J.D. (2002) Predicting depressive symptoms with a new measure of shame: The Experience of Shame Scale. British Journal of Clinical Psychology 41:
pp. 29–42.
Aronfreed, J. (1964) The Origins of Self-criticism. Psychological Review 71 (3): pp. 193–218.
Ayto, J. (2009) Oxford Dictionary of English Idioms. (3rd ed). Oxford: Oxford University Press.
Bagby, R.M., Ryder, A.G., Schuller, D.R. and Marshall, M.B. (2004) The Hamilton Depression Rating Scale: Has the Gold Standard Become a Lead Weight? American Journal of Psychiatry 161: pp. 2163–2177.
Baiao, R., Gilbert, P., McEwan, K. and Carvalho, S. (2015) Forms of Self-Criticising/attacking and Self-reassuring Scale: psychometric properties and normative study. Psychology and psychotherapy: Theory, Research and Practice 88: pp. 438–452.
Balsamo, M., Macchia, A., Carlucci, L., Picconi, L., Tommasi, M., Gilbert, P. and Saggino, R. (2015) Measurement of external shame: An inside view. Journal of Personality
Assessment 97 (1): pp. 81–89. Available at: DOI: 10.1080/00223891.2014.947650 (Accessed 12th May 2020).
Bandura, A. (1977) Social Learning Theory. Englewood-Cliff, New Jersey: Prentice Hall.
Barnard, L.K. and Curry, J.F. (2011) Self-compassion: conceptualisations, correlates and interventions. Review of General Psychology 15(4): pp. 289–303.
Bastin, C., Harrison, B.J., Davey, C.G., Moll, J. and Whittle, S. (2016) Feelings of shame, embarrassment and guilt and their neural correlates: a systematic review. Neuroscience and Biobehavioural Reviews 71: pp. 455–471.
Baumeister, R.F. and Leary, M.R. (1995) The need to belong: desire for interpersonal attachments as a fundamental human motivation. Psychological Bulletin 117: pp. 497–529.
Baxter, A.J., Scott, K.M., Ferrari, A.J., Norman, R.E., Vos, T. and Harvey, H.A. (2014) Challenging the myth of an ‘epidemic’ of common mental disorders: trends in the global prevalence of anxiety and depression between 1990 and 2010. Depression and Anxiety 31(6): pp. 506–516. Available at: https://doi.org/10.1002/da.22230 (Accessed on 4th January 2020).
Beck, A.T. (1983) Cognitive Therapy of depression: New Perspectives. In Clayton, P.J. and Barrett, J.E. (Eds.) Treatment of depression: old controversies and new approaches New York: Raven Press, pp. 265–290.
Beck, A.T. (1967) Depression: clinical, experimental and theoretical aspects. New York: Harper Row.
Beck, A.T. (1963) Thinking and Depression I: Idiosyncratic Content and cognitive distortions. Archives of General Psychiatry 9: pp. 324–333.
Beck, A. T., Brown, G., Steer, R.A., Eidelson, J. I. and Riskind, J. H. (1987) Differentiating anxiety and depression: A test of the cognitive content-specificity hypothesis. Journal of Abnormal Psychology 96(3): pp. 179–183.
Beck, A.T., Emery, G. and Greenberg, R.L. (1985) Anxiety disorders and phobias: a cognitive approach. New York: Basic Books.
Beck, A.T., Rush, A.J., Shaw, A.J., and Emery, G. (1979) Cognitive Therapy for Depression. New York: Guilford Press.
Beck, A. T., Steer, R. A. and Garbin, M. G. (1988) Psychometric properties of the Beck depression inventory: Twenty–five years of evaluation. Clinical Psychology Review 8: pp. 77– 100.
Beck, A.T., Ward, C.H., Mendelson, M., Mock, J.E. and Erbaugh, J.K. (1961) An Inventory for Measuring Depression. Archives of General Psychiatry 4: pp. 561–571.
Beck, A.T., Weissman, A., Lester, D. and Trexler, L. (1974) The measurement of pessimism: the hopelessness scale. Journal of Consulting and Clinical Psychology 42: pp. 861–865.
Beevers, C.G. and Carver, C.S. (2003) Attentional Bias and Mood Persistence as Prospective Predictors of Dysphoria. Cognitive Therapy and Research 27: pp. 619–637. Available at: https://doi.org/10.1023/A:1026347610928 (Accessed on 5th March, 2020).
Belsher, G. and Costello, C. G. (1988) Relapse after recovery from unipolar depression: A critical review. Psychological Bulletin 104(1): pp. 84–96. Available at: https://doi.org/10.1037/0033-2909.104.1.84 (Accessed on 4th January 2020).
Benevides, J., da Motta, C., Sousa, M., Claderia, S.N. and Carvalho, C. (2016) The Psychometric properties of the brief Other as Shamer Scale for children (OAS-C): a preliminary validation studies in a sample of Portuguese children. 3.º Congresso Internacional de Saúde do IPLeiria, Instituto Politécnico de Leiria, 6–7 de maio. (Poster) available at: https://repositorio.uac.pt (Accessed on 2nd July 2020).
Bennett-Levy, J.B., Butler, G., Fennell, M., Hackman, A., Mueller, M. and Westbrook, D. (2004)
The Oxford Guide to Behavioural Experiments in Cognitive Therapy. Oxford: Oxford University Press.
Bernet, C.Z. and Stein, M.B. (1999) Relationship of childhood maltreatment to the onset and course of major depression in adulthood. Depression and Anxiety 9: pp. 169–174.
Bernstein, E.E., Evan, E.M., Van Bork, R., Moriarty, D.P., Giollabhui, N.M., Abramson, L.Y. and Alloy, L. (2019) Unique and predictive relationships between components of cognitive vulnerability and symptoms of depression. Depression and Anxiety 36 (10): pp. 950–959. Available at: DOI: 10.1002/da.22935 (Accessed on 6th June 2020).
Berwick, D. (2013) A promise to learn-a commitment to act: improving the safety of patients in England. Cmnd 2901213. London. Department of Health.
Bieling, P.J., Beck, A.T. and Brown, G.K. (2000) The sociotropy-autonomy scale: structure and implications. Cognitive Therapy and Research 24: pp. 763–780.
Bierhoff, H. W. (2005) The psychology of compassion and prosocial behaviour. In: Gilbert, P.
(Ed.) Compassion: Conceptualisation, Research and use in Psychotherapy. Hove, East Sussex: Routledge, pp. 148–167.
Biesta, G. (2010) Pragmatism and the Philosophical Foundations of Mixed Methods Research. In: Tashakkori, A. and Teddlie, C. (Eds.) Sage Handbook of Mixed Methods in Social and Behavioural Research. Thousand Oaks, CA: Sage Publications Inc, pp. 95–117.
Biesta, G. (2007). Bridging the gap between educational research and educational practice:
The need for critical distance. Educational Research and Evaluation 13 (3): pp. 295–301.
Biggerstaff, D. and Thompson, A.R. (2008) Interpretative Phenomenological Analysis (IPA): A qualitative methodology of choice in healthcare research. Qualitative Research in Psychology 5 (3): pp. 214–224.
Bland, J.M. and Altman, D.G. (1997) Statistics notes: Cronbach’s Alpha. British Medial Journal
314: 572. Available at: https://www.bmj.com/content/bmj/314/7080/572.full.pdf (Accessed 25th August 2019).
Blatt, S.J. (1974) Levels of object representation in anaclitic and introjective depression. Psychoanalytic Studies of the Child 29: pp. 107–157.
Blatt, S.J., D’Afflitti, J.P. and Quinlan, D.M. (1976) Depressive Experiences Questionnaire unpublished manuscript. New Haven: Yale University, Department of Psychiatry. In Klein, D.N., Harding, K., Taylor, E.B. and Dickstein, S. (1988) Dependency and self-criticism in depression: Evaluation in a clinical population Journal of Abnormal Psychology 97 (4) pp. 399404.
Blatt, S.J., Quinlan, D.M., Chevron, E.S., McDonald, C. and Zuroff, D. (1982) Dependency and self-criticism: psychological dimensions of depression. Journal of Consulting and Clinical Psychology 50 (1): pp. 113–124.
Blatt, S.J and Zuroff, D. (1992) Interpersonal relatedness and self-definition: Two prototypes for depression. Clinical Psychology Review 12: pp. 527–254.
Blesher, G. and Costello, C.G. (1988) Relapse after recovery from unipolar depression: a critical review. Psychological Bulletin 104: pp. 84–96.
Blum, A. (2008) Shame and guilt, misconceptions and controversies: a critical review of the literature. Traumatology 14 (3): pp. 91–102.
Bower, G. H. (1981). Mood and memory. American Psychologist 36: pp. 129–148.
Bowlby, J. (1973) Attachment and Loss: volume 2: Separation, anxiety and anger. New York: Basic Books.
Bowlby, J. (1969) Attachment and Loss: volume 1: Attachment. New York: Basic Books.
Bradley, B.P., Mogg, K. and Lee, S.C. (1997) Attentional biases for negative information in induced and naturally occurring dysphoria. Behaviour, Research and Therapy 35 (10): pp. 911–927.
Brawley, L.R. (1993) The Practicality of using social psychological therapies for exercise and health research and intervention. Journal of Applied Sport Psychology 5: pp. 99–115.
Brenner, R.E., Heath, P.J., Vogel, D.L. and Crede, M. (2017) Two is more valid than one: examining the factor structure of the self-compassion scale (SCS). Journal of Consulting and Clinical Psychology 64 (6): pp. 696–707. Available at: http://doi.org/10.1037/cou0000211 (Accessed on 5th March 2020).
Brewin, C.R. and Firth-Cozens, J. (1997) Dependency and self-criticism as predictors of depression in young doctors. Journal of Occupational Health Psychology 2: pp. 242–246.
Brewin, C.R. and Furnham, A. (1987) Dependency, self-criticism and depressive attributional style. British journal of Clinical Psychology 26: pp. 225–226.
Brewin, C. R., Wheatley, J., Patel, T., Fearon, P., Hackmann, A., Wells, A. and Myers, S. (2009) Imagery rescripting as a brief stand-alone treatment for depressed patients with intrusive memories. Behaviour Research and Therapy 47(7): pp. 569–76. Available at: https://doi.org/10.1016/j.brat.2009.03.008 (Accessed on 9th January 2020).
British Association of Behavioural and Cognitive Psychotherapies (BABCP) (2017) Standards of Conduct, Performance and Ethics (online). Available at: www.babcp.com (Accessed 15th July 2020).
Brocki, J.M. and Wearden, A.J. (2006) A critical evaluation of the use of Interpretative Phenomenological Analysis (IPA) in health psychology. Psychology and Health 21 (1): pp. 87108.
Brookfield, S. (1998) Critically Reflective Practice. The Journal of Continuing Education in Health Professions 18: pp. 197–205.
Brown, J.D. and Silberschatz, G. (1989) Dependency, Self-criticism and Depressive Attributional Style. Journal of Abnormal Psychology 98 (2): pp. 187–188.
Brown, J.D. and Weiner, B. (1984) Affective consequences of ability versus effort ascriptions: controversies, resolutions and quandaries. Journal of Educational Psychology 76: pp. 146158.
Burman, E. (1994) Interviewing. In: Banister, P., Burman, E., Parker, I. and Tindall, C. (Eds.) Qualitative methods in Psychology: A research guide. Berkshire: Open University Press McGraw Gill Education, pp. 49–71.
Butler, A.C., Chapman, J.E., Forman, E.M. and Beck, A.T. (2006) The empirical status of cognitive-behavioural therapy: a review of meta-analyses. Clinical Psychology Review 26: pp. 17–31.
Callaghan P, Butler D. (2017) Mental health nursing in the 21st century: reclaiming the art, science and craft of caring. In: Chambers, M. (ed.) Psychiatric and Mental Health Nursing: The Craft of Caring. (3rd edn). London: Routledge, pp. :817–829.
Cambridge online Dictionary (2019) Cambridge: Cambridge University Press. Available at: https://dictionary.cambridge.org (Accessed 6th October 2019).
Cangur, S. and Ercan, I. (2015) Comparison of model fit indices used in structural equation modelling under multivariate normality. Journal of Modern Applied Statistical Methods 14 (1): pp. 152–167. Available at: DOI: 10.22237/JMASM/1430453580 (Accessed 25th August 2019).
Carver, C.S. and Ganellen, R.J. (1983) Depression and components of self-punitiveness: high standards, self-criticism and overgeneralization. Journal of Abnormal Psychology 92: pp. 330337. Available at: https://doi.org/10.1037/0021-843X.92.3.330 (Accessed 5th November 2014).
Carver, C. S., La Voie, L., Kuhl, J. and Ganellen, R. J. (1988) Cognitive concomitants of depression: A further examination of the roles of generalization, high standards, and selfcriticism. Journal of Social and Clinical Psychology 7 (4): pp.350–365. Available at: https://doi.org/10.1521/jscp.1988.7.4.350 (Accessed 5th November 2014).
Castilho, P., Pinto-Gouveia, J. and Duarte, J. (2015) Exploring self-criticism: confirmatory factor analysis of the FSCSRS in clinical and non-clinical samples. Clinical Psychology and psychotherapy 22: pp. 153–164.
Catarino, F., Gilbert, P., McEwan, K. and Baiao, R. (2014) Compassion motivations: distinguishing submissive compassion from genuine compassion and its association with shame, submissive behaviour, depression, anxiety and stress. Journal of Social and Clinical Psychology 33 (5): pp. 399–412. Available at: DOI:10.1521/jscp.2014.33.5.399 (Accessed 12th May 2020).
Chamberlain, K. (2011) Troubling Methodology. Health Psychology Review 5: pp. 48–54.
Chapman, D.P., Perry, G. and Strine, T.W. (2005) The Vital Link Between Chronic Disease and Depressive Disorders: Preventing Chronic Disease. Public Health Research, Practice and Policy 2 (2): pp. 1–10.
Cheung, M.S-P., Gilbert, P. and Irons, C. (2004) An exploration of shame, social rank and rumination in relation to depression. Personality and Individual Differences 26 (5): pp. 11431153.
Claesson, K. and Sohlberg, S. (2002) Internalized shame and early interactions characterised by indifference, abandonment and rejection: replicated finding. Clinical Psychology and psychotherapy 9 (2): pp. 227–284.
Cleare, A. Pariante, C.M; Young, A.H; Anderson, I.M; Christmas, D; Cowen, P.J; Dickens, C;
Ferrier, I.N; Geddes, J; Gilbody, S; Haddad, P.M; Katona, C; Lewis, G; Malizia, A; McAllisterWilliams, R.H; Ramchandani, P; Scott, J; Taylor, D; Uher, R (2015) Evidence based guidelines for treating depressive disorders with antidepressants: a revision of the 2008 British Association for Psychopharmacology guidelines. Journal of Psychopharmacology 29 (5): pp: 459–525.
Comrey, A. L. and Lee, H. B. (1992). A first course in factor analysis. (2nd ed). Hillsdale, NJ: Erlbaum.
Conway, M.A. (2005) Memory and the self. Journal of Memory and Language 53 (4): pp. 594628.
Conway, C.R., George, M.S. and Sackheim, H.A. (2017) Towards evidence -based, operational definition of treatment resistant depression: when enough is enough. Journal of American Medical Association: Psychiatry 74 (1): pp. 9–10.
Conway, C.C. and Slavich, G.M. (2017) Behaviour genetics of prosocial behaviour. In Gilbert, P. (Ed.) Compassion: Concepts, Research and Applications. London: Routledge, pp. 151–170.
Costa, J., Marôco, j., Pinto-Gouveia, J., Ferreira, C. and Castilho, P. (2016) Validation of the psychometric properties of the self-compassion scale: testing the factorial validity and factorial invariance of the measure among borderline personality disorder, anxiety disorder, eating disorder and general populations. Clinical Psychology and Psychotherapy 23 (5): pp. 460–468. Available at: DOI: 10.1002/cpp.1974 (Accessed 18th May 2020).
Coyne, J.C. and Whiffen, V.E. (1995) Issues in personality disorder as diathesis for depression: The case of sociotropy-dependency and autonomy- self-criticism. Psychological Bulletin 18 (3): pp. 358–378.
Craddock, N. and Mynors-Wallis, L. (2014) Psychiatric Diagnosis: impersonal, imperfect and important. The British Journal of Psychiatry 204 (2): pp. 93–95. Available at: doi:
10.1192/bjp.bp.113.133090 (Accessed 9th January 2020).
Cresswell, J.W. (2010) Mapping the developing landscape of mixed methods research. In Tashakkori, A. and Teddlie, C. (Eds.) Sage Handbook of Mixed Methods in Social and Behavioural Research. Thousand Oaks, California: Sage Publications Inc., pp. 45–68.
Cresswell, J.W. and Plano-Clark, V.L. (2011) Designing and Conducting Mixed Methods Research. (2nd ed.) Thousand Oaks, California: Sage Publications Inc.
Cronbach, L. J. and Meehl, P. E. (1955) Construct validity in psychological tests. Psychological Bulletin 52(4): pp. 281–302.
Cuijpers, P., Berking, M., Andersson, G., Quigley, L., Kleiboer, A. and Dobson, K.S. (2013) A meta-analysis of cognitive-behavioural therapy for adult depression, alone and in comparison with other treatments. Canadian Journal of Psychiatry 58 (7): pp. 376–385.
Cuijpers, P., van Straten, A., Bohlmeijer, E., Hollon, S.D. and Andersson, G. (2010) The effects of psychotherapy for adult depression are overestimated: a meta-analysis of study quality and effect size. Psychological Medicine 40 (2): pp. 211–223.
Cunha, M., de Jesus Xavier, A., Cherpe, S. and Pinto Gouiveia, J. (2017) Assessment of shame in adolescents: The other as shamer scale. Psychology: Theory and Research 33: Brasilia, Epub: pp. 1–11. Available at: https://doi.org/10.1590/0102.3772e3336 (Accessed 10th May 2020).
Curley, S., Smout, M.F. and Denson, L.A. (2019) Does behavioural activation lack credibility among those who need it most? A comparison of responses to rationales for behavioural activation and schema therapy Behavioural and Cognitive Psychotherapy 47 (4): pp. 493–498.
Cusin C., Yang H., Yeung A and Fava, M. (2010) Rating scales for depression. In: Baer, L. and Blais, M.A. (Eds.) Handbook of clinical rating scales and assessment in psychiatry and mental health. New York: Humana Press, Springer, pp. 7–35.
Dancey, C.P., Reidy, J.G. and Rowe, R. (2012) Descriptive statistics. In: Statistics for the health Sciences: A non-mathematical introduction. Sage: London, pp. 75–121.
Darzi, A. (2008) Briefing: High Quality Care for All: the NHS next stage review final report (online). available at: https://www.kingsfund.org.uk/ (Accessed 1ST July 2020).
Davis, M.H. (1983) Measuring individual differences in empathy: evidence for a multidimensional approach. Journal of Personality and Social Psychology 44 (1): pp. 113–126.
Department of Health (DoH) (2005) Research Governance Framework for Health and Social Care (2nd ed.). Available at: https://www.gov.uk/ (Accessed 1st July 2020).
Derogatis, L. R., Lipman, R. S. and Covi, L (1973) SCL-90: An outpatient psychiatric rating scale preliminary report. Psychopharmacology Bulletin 9 (1): pp. 13—28.
De Souza, A.C., Costa-Alexandre, N.M. and De Brito Guirardello, E. (2017) Psychometric properties in instrument evaluation of reliability and validity. Epidemiologia e Serviços de Saúde Brasilia, (Epidemiology and Health Services Brazil) 26 (3): pp. 1–11. Available at: doi.org/10.5123/s1679-49742017000300022 (Accessed 3rd July 2019).
Dewey, J. (1938) Logic: The theory of inquiry. Holt: Rhinehart and Winston.
Dickerson, S.S., Grunewald, T.L. and Kemeny, M.E. (2004) When the social self is threatened: shame, physiology and health Journal of Personality 72 (6): pp. 1191–1216.
Dimidjian, S., Hollon, S.D., Dobson, K.S., Schmaling, K.B., Kohlenberg, RJ., Addis, M.E., Gallop, R., McGlinchey, J.B., Markley, D.K., Gollan, J.K., Atkins, D.C., Dunner, D.L, and Jacobson, N.S. (2006) Randomized trial of behavioural activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. Journal of Consulting and Clinical Psychology 74(4): pp. 658–670.
Disner, S.G., Shumake, J.D. and Beever, C.G. (2017) Self-referential schemas and attentional bias predict severity and naturalistic course of depression. Cognition and Emotion 31 (4): pp. 632–644.
Dobson K.S. (1989) A meta-analysis of the efficacy of cognitive therapy of depression. Journal of Consulting and Clinical Psychology 57 (3): pp. 414–419.
Doyle, L., Brady, A.M. and Byrne, G. (2009) An overview of mixed methods research. Journal of Research in Nursing 14 (2): pp: 175–185.
Ehret, A.M., Joorman, J. and Berking, M. (2015) Examining risk and resilience factors for depression: The role of self-criticism and self-compassion. Cognition and Emotion 29 (8): pp. 1496–1504.
Ekman, P. (1992) An argument for basic emotions. Cognition and Emotion 6 (3–4): pp. 169200.
Elkin, I., Shea, T.M., Watkins, J.T., Imber, S.D., Sotsky, S.M., Collins, J.F., Glass, D.R., Pilkonis,
P.A., Leber, W.R., Docherty, J.P., Fiester, S.J. and Parloff, M.B. (1989) National Institute of Mental Health treatment of depression collaborative research program: General effectiveness of treatments. Archives of General Psychiatry 46 (11): pp. 971–983.
Fava, M. (2003) Diagnosis and definition of treatment resistant depression. Biological Psychiatry 53 (8): pp. 649–659.
Fennell, M.J.V. (1998) Cognitive Therapy in the treatment of low self-esteem. Advances in Psychiatric Treatment 4: pp. 296–304.
Fennell, M.J.V. (1989) Depression. In Hawton, K., Salkovskis, P. M., Kirk, J. and Clark, D. M.
(Eds.) Cognitive behaviour therapy for psychiatric problems: A practical guide. Oxford: Oxford University Press, pp.169–234.
Field, A. (2013) Discovering statistics using IBM SPSS Statistics. (4thed.) Sage publications: London.
First, M.B., Spitzer, R.L., Gibbon, M. and Endicott, J. (1997) Structured Clinical Interview for DSM-IV Axis 1 Disorders. Washington, DC: American Psychiatric Press.
Frank, E., Kupfer, D.J., Perel, J.M., Cornes, C., Jarret, D.B., Mallinger, A.G., Thase, M.E., McEachran, A.B. and Grocchocinski, V.J. (1990) Three-year outcomes for maintenance therapies in recurrent depression. Archives of General Psychiatry 47 (12): pp. 1093–1099.
Frijda, N.H. (1987) Emotion, cognitive structure an action tendency. Cognition and Emotion 1 (2): pp. 115–143.
Frost, J. (2019). Regression Analysis: An Intuitive Guide for Using and Interpreting Linear
Models (1st ed.) Available at: https://statisticsbyjim.com/regression/regression-analysishttps://statisticsbyjim.com/regression/regression-analysis-intuitive-guide/][intuitivehttps://statisticsbyjim.com/regression/regression-analysis-intuitive-guide/guide/ (Accessed 23rd May 2020).
Frost, M.H., Reeve, B.B., Liepa, A.M., Stauffer, J.W., Hays, R.D. and the Mayo/FDA Patient-Reported Outcomes Consensus Meeting Group (2007) What Is Sufficient Evidence for the Reliability and Validity of Patient-Reported Outcome Measures? Value in Health 10 (2): pp: S94-S105. Available at: https://onlinelibrary.wiley.com/doi/pdf/10.1111/j.1524-4733.2007.00272 (Accessed 1st July 2020).
Furukawa, T.A., Schramm, E., Weitz, E.S., Salanti, G., Efthimiou, O., Michalak, J., Watanabe,
N., Cipriani, A., B Keller, M.B., H Kocsis, J.H. Klein, D.N. and Cuijpers, P. (2016) CognitiveBehavioural Analysis System of Psychotherapy (CBASP), a drug, or their combination: differential therapeutics for persistent depressive disorder: a study protocol of an individual participant data network meta-analysis. British Medical Journal Open Access 4th May. Available at: 6:e011769. doi:10.1136/bmjopen-2016-011769 (Accessed 8th February 2020).
Garland, A. (2016) Cognitive behavioural case formulation for complex and recurrent depression. In: Tarrier, N. and Johnson, J. (Eds.) Case Formulation in Cognitive Behaviour Therapy: The treatment of challenging and complex cases (2nd ed.). London: Routledge, pp. 119–142.
Garland, A. and Scott, J. (2008) Chronic depression. In: Wishman, M. (Ed.) Cognitive Therapy for complex and co-morbid depression: conceptualization, assessment and treatment. New York: Guilford Press, pp. 88–109.
Gaynes, B.N., Warden, M.H., Trivedi, S.R., Wisniewski, M., Fava, M. and Rush, A.J. (2009) What did STAR*D teach us? Results from a large scale, practical, clinical trial for patients with depression. Psychiatric Services 60 (11): pp. 1439–1445.
Geiger, M., Pfattheicher, S., Hartung, J., Weiss, S., Schindler, S. and Wilhelm, O. (2018) Selfcompassion as a facet of neuroticism? a reply to the comments of Neff, Toth-Kiraly and Colosimo. European Journal of Personality 32: pp. 393–404. Available at: DOI:
10.1002/per.2168 (Accessed April 6th 2020).
Germer, C.K. (2009) The mindful path to self-compassion: freeing yourself from destructive thoughts and emotions. New York: Guilford Press.
Gilbert, P. (2017a) Compassion as a social mentality: an evolutionary approach. In Gilbert, P. (Ed.) Compassion: concepts, research and applications. Oxon: Routledge, pp: 31–68.
Gilbert, P. (2017b) Compassion: definitions and controversies. In Gilbert, P. (Ed.) Compassion:
concepts, research and applications. Oxon: Routledge, pp: 3–15.
Gilbert, P. (2016) A biopsychosocial and evolutionary approach to formulation. In: Tarrier, N. and Johnson, J. (Eds) Case Formulation in Cognitive Behaviour Therapy: The treatment of challenging and complex cases. (2nd ed.) London: Routledge, pp. 52–89.
Gilbert, P. (2014) The origins and nature of compassion focused therapy. British Journal of Clinical Psychology 53: pp. 6–41. Available at: doi: 10.1111/bjc.12043 (Accessed 9th May 2020).
Gilbert, P. (2010a) Personal Communication. Individual Clinical Supervision within the CLAHRC-NDL Mood Disorders Study. (2010–2015).
Gilbert, P. (2010b) Compassion Focused Therapy. Dryden, W. (Series Ed.) CBT Distinctive Features Series. Hove: East Sussex, Routledge.
Gilbert, P. (2009) The Compassionate Mind. London: Constable and Robinson.
Gilbert, P. (2007a) The evolution of shame as a marker for relationship security: A biopsychosoical approach. In: Tracy, J.L., Robins, R.W. and Tangney, J.P. (Eds.) The selfconscious emotions: Theory and Research. New York: Guilford Press, pp. 283–309.
Gilbert, P. (2007b) An Introduction to Compassion Focused Therapy. 2-day clinical skills workshop, 8–9th June 2007, Kingsway Hospital, Derby, UK. East Midlands Branch of the British Association of Behavioural and Cognitive Psychotherapies (BABCP).
Gilbert, P. (2005a) Introduction and Outline. In: Gilbert. P. (Ed.) Compassion: conceptualisation, research and use in psychotherapy. Hove: Routledge, pp 1–6.
Gilbert, P. (2005b) Compassion and cruelty: a biopsychosocial approach. In: Gilbert. P. (Ed.) Compassion: conceptualisation, research and use in psychotherapy. Hove: Routledge, pp 974.
Gilbert, (2003) Evolution, social roles and the differences in shame and guilt. Social Research 70 (4): pp. 1205–1230.
Gilbert, P. (2001) Depression and Stress: a biopsychosocial exploration of evolved functions and mechanisms. Stress 4(2): pp: 121–235.
Gilbert, P. (2000) The relationship of shame, social anxiety and depression: the role of the evaluation of social rank. Clinical Psychology and Psychotherapy 7 (3): pp. 174–189.
Gilbert, P. (1998) What is Shame? In: Gilbert, P. and Andrews, B. (Eds.) Shame: interpersonal behaviour, psychopathology and culture Oxford: Oxford University Press, pp. 3–38.
Gilbert, P. (1997) Overcoming depression: a self-help guide using cognitive-behavioural techniques. Robinson New York: Robinson.
Gilbert, P. (1995) Biopsychosocial approaches and evolutionary theory as aids to integration in Clinical Psychology and Psychotherapy. Clinical Psychology and Psychotherapy 2: pp. 135156.
Gilbert, P. (1992) Depression: the evolution of powerlessness. New York: Guilford press.
Gilbert, P. (1989) Human Nature and Suffering. Hove: Lawrence Erlbaum.
Gilbert, P. and Allan, S. (1994) Assertiveness, submissive behaviour and social comparison. British Journal of Clinical Psychology 33 (3): pp. 295–306. Available at: doi.10.1111/j.20448260.1994.tb.01125.x (Accessed 5th July 2017).
Gilbert, P., Allan, S. and Goss, K. (1996) Parental Representations, shame, interpersonal problems and vulnerability to psychopathology. Clinical Psychology and Psychotherapy 3 (1): pp. 23–34. Available at: https://doi.org/10.1002/(SICI)1099-0879 (Accessed 5th July 2017).
Gilbert, P., Baldwin, M.W., Irons, C., Baccus, J.R. and Palmer, M. (2016) Self-criticism and selfwarmth: an imagery study exploring their relation to depression. Journal of Cognitive Psychotherapy 20 (2): pp 183–200. Available at: DOI: 10.1891/jcop.20.2.183 (Accessed 9th November 2019).
Gilbert, P., Birchwood, M., Trower, J., Hay, B., Murray, A., Meaden, K., Olsen, K. and Miles, J.N.V. (2001) An exploration of evolved mental mechanisms for dominant and subordinate behaviour in relation to auditory hallucinations in schizophrenia and critical thoughts in depression. Psychological Medicine 31: pp. 1117–1127 Available at: doi:10:1017/S003329170105409z (Accessed 9th May 2020).
Gilbert, P., Cheung, M.A., Grandfield, T., Campey, F. and Irons, C. (2003) Recall of threat and submissiveness in childhood: Development of a new scale and its relationship with depression, social comparison and shame. Clinical Psychology and Psychotherapy 10 (2): pp. 108–115.
Gilbert, P., Cheung, M.A., Irons, C. and McEwan, K. (2005) An exploration into depressionfocused and anger-focused rumination in relation to depression in a student population. Behavioural and Cognitive Psychotherapy 33 (3): pp. 273–283.
Gilbert, P. and Choden (2013) Mindful Compassion: using the power of mindfulness and compassion to transform our lives. London: Constable and Robinson.
Gilbert, P. and Choden (2011) Introduction to Compassion Focused Therapy. 3-day experiential workshop, 6th-8th July 2011, London, UK. Compassionate Mind Foundation and Samye Ling Buddhist Retreat, Holy Isle, Scotland.
Gilbert, P., Clarke, M., Hempel, S., Miles, J.N.V. and Irons, C. (2004) Criticising and reassuring oneself: an exploration of forms, styles and reasons in female students. British Journal of Clinical Psychology 43 (1): pp. 31–50.
Gilbert, P., Durrant, R. and McEwan, K. (2006) Investigating relationships between perfectionism, forms and functions of self-criticism and sensitivity to put downs. Personality and Individual Differences 41 (7): pp. 1299–1308.
Gilbert, P. and Irons, C. (2005) Focused therapies and compassionate mind training for shame and self-attacking. In: Gilbert, P. (Ed.) Compassion: conceptualisation, research and use in psychotherapy. Hove: Routledge, pp. 263–325.
Gilbert, P., McEwan, K., Gibbons, L., Chotai, S., Duarte, J. and Matos, M. (2011) Fears of compassion and happiness in relation to alexithymia, mindfulness and self-criticism. Psychology and Psychotherapy 85 (4): pp. 239–255.
Gilbert, P., McEwan, K., Irons, C., Bhundia, R., Christie, R., Broomhead, C., and Rockcliff, H.(2010), Self-harm in a mixed clinical population: the roles of self-criticism, shame and social rank. British journal of Clinical Psychology 49 (4): pp. 563–576.
Gilbert, P., McEwan, K., Matos, M. and Rivis, A. (2011) Fears of compassion: development of three self-report measures. Psychology and Psychotherapy 84 (3): pp. 239–255.
Gilbert, K. McEwan, R. Mitra, L. Franks, A. Richter and H. Rockliff (2008) Feeling safe and content: A specific affect regulation system? Relationship to depression, anxiety, stress, and selfcriticism. The Journal of Positive Psychology 3 (3): pp 182–191. Available at: doi:
10.1080/17439760801999461 (Accessed 9TH January 2020).
Gilbert, P. and McGuire, M.T. (1998) Shame, status and social roles: psychobiology and evolution. In Gilbert, P. and Andrews, B. (Eds.) Shame: interpersonal behaviour, psychopathology and culture Oxford: Oxford University, pp 99–125.
Gilbert, P. and Procter, S. (2006) Compassionate Mind Training for people with high shame and self-criticism: overview and pilot study of a group therapy approach. Clinical Psychology and Psychotherapy 13 (6): pp. 353–379.
Glaser, B. G. and Strauss, A. L. (1967) The discovery of grounded theory: Strategies for qualitative research. Chicago: Aldine Publishers.
Gloaguen V, Cottraux J, Cucherat M and Blackburn, I.M. (1998) A meta-analysis of the effects of cognitive therapy in depressed patients. Journal of Affective Disorders 49 (1): pp. 59–72.
Global Burden of Disease (2017) Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990– 2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet (2018) 392: pp. 1789–1858 Available at: https://www.thelancet.com/ (Accessed July 2020).
Goetz, J.L. and Keltner, D. (2007) Shifting meanings of self-conscious emotions across cultures. In: Tracy, J.L., Robins, R.W. and Price Tangney, J.P. (Eds.) The self-conscious emotions: Theory and Research New York: Guilford Press, pp. 153–173.
Goetz, J., Keltner, D. and Simon-Thomas, E. (2010) Compassion: an evolutionary analysis and empirical review. Psychological Bulletin 136 (3): pp. 351–374. Available at: DOI:
10.1037/a0018807 (Accessed 11TH January 2019).
Goldberg, L.R. (1990) An ‘alternative description of personality’: The big five factor structure. Journal of Personality and Social Psychology 59 (6): pp. 1216–1229.
Goldstein, H. (2003) Multilevel Statistical Models. (3rd ed.) London: Edward Arnold.
Goss, K., Gilbert, P. and Allan, S. and (1994) An exploration of shame measures I: The Other as Shamer Scale. Personality and Individual Differences 17 (5): pp. 713–717.
Gotlib, I. H., Krasnoperova, E., Yue, D. N., & Joormann, J. (2004). Attentional biases for negative interpersonal stimuli in clinical depression. Journal of Abnormal Psychology 113 (1): pp. 127–135. Available at: https://psycnet.apa.org/doi/10.1037/0021-843X.113.1.121 (Accessed 6th February 2020).
Gouva, M., Paschou, A., Kaltsouda, A., Dragioti, E., Paralikas, T., Mantzoukas, S. and
Kotrotsiou, E. (2016) Psychometric properties and factor structure of the Greek version of the Other As Shamer Scale (OAS). Inter-scientific Health Care 8 (4): pp. 159–164. Available at: https://eds.b.ebscohost.com/ (Accessed 7th July 2020).
Grayson, P.A. (1983) The self-criticism gambit: How to safeguard self-esteem through blaming the self. Individual Psychology 39 (1): pp. 17–27.
Greene, J.C. (2008) Is mixed methods social inquiry a distinctive methodology? Journal of Mixed Methods Research 2 (1): pp. 7–22.
Green, S., Lambon-Ralph, M.A., Moll, J., Deakin, J.F.W. and Zahn, R. (2012) Guilt-selective functional disconnection of anterior temporal and subgenual cortices in major depressive disorder guilt selective functional disconnection. Archives of General Psychiatry 69 (10): pp. 1014–1021.
Green, S., Moll, J., Deakin, J.F.W., Hulleman, J. and Roland Zahn, R. (2013) Proneness to decreased negative emotions in major depressive disorder when blaming others rather than oneself. Psychopathology 46: pp. 34–44 Available at: DOI: 10.1159/000338632 (Accessed April 2019).
Greenberg, L.S. and Pascual-Leone, (2006) Emotion in Psychotherapy: A practice friendly research review. Journal of Clinical Psychology 62 (5): pp. 611–630. Available at:
https://doi.org/10.1002/jclp.20252 (Accessed 11th February 2020).
Greenwald, D.F. and Harder, D.W. (1998) Domains of shame: evolutionary, cultural and psychotherapeutic aspects. In Gilbert, P. and Andrews, B. (Eds.) Shame: interpersonal behaviour, psychopathology and culture Oxford: Oxford University Press, pp 225–245.
Grey, N., Holmes, E. and Brewin, C. (2002) Peritraumatic emotional ‘hotspots’ in memory.
Behavioural and Cognitive Psychotherapy 29 (3): pp. 367–372.
Grice, P. (1989) Studies in the Way of Words. Cambridge Massachusetts: Harvard University Press.
Grusec, J. (1966) Some antecedents of self-criticism. Journal of Personality and Social Psychology 4 (3): pp. 244–252.
Gu J., Cavanagh K., Baer R, and Strauss C. (2017) An empirical examination of the factor structure of compassion. PLoS ONE 12(2): e0172471. Available at: https://doi.org/10.1371/journal.pone.0172471 (Accessed 12th February 2020).
Gulliford, M.C., Adams, G., Ukoumunne, O.C., Latinovic, R., Chinn, S., and Campbell, M.J. (2005) Intraclass correlation coefficient and outcome prevalence are associated in clustered binary data. Journal of Clinical Epidemiology 58 (3): pp. 246–251.
Guthrie., E, Moorey., J, Margison., F, Barker., H, Palmer., S, McGrath., G, Tomenson, B. and Creed., F. (1999) Cost-effectiveness of brief psychodynamic-interpersonal therapy in high utilizers of psychiatric services. Archives of General Psychiatry 56 (6): pp. 519–526.
Halamova, J., Kanovsky, M., Gilbert, P., Troop, N.A., Zuroff, D.C., Hermanto, N., Petrocchi, N.,
Sommers-Spijkerman, M., Kirby, J.N., Shahar, B., Kreiger, T., Matos, M., Asano, K., Yu, F., Basran, J. and Kupeli, N. (2018) The Factor structure of the forms of self-criticising/attacking and self-reassuring scale in thirteen distinct populations. Journal of Psychopathology and Behavioural Assessment 40: pp. 736–751. Available at: https://doi.org/10.1007/s10862https://doi.org/10.1007/s10862-018-9686-2][018https://doi.org/10.1007/s10862-018-9686-29686-2 (Accessed 8th June 2020).
Hamilton, M. (1960) A rating scale for depression. Journal of Neurology, Neurosurgery and Psychiatry 23 (1): pp. 56–62.
Harder, D.H. and Zalma, A. (1990) Two promising shame and guilt scales: a construct validity comparison. Journal of Personality Assessment 55:(3–4): pp. 729–745. Available at: DOI:
10.1080/00223891.1990.9674108 (Accessed 18th July 2013).
Hartlage, S., Arduino, K. and Alloy, L.B. (1998) Depressive Personality characteristics: state dependent concomitants of depressive disorder and traits independent of current depression. Journal of Abnormal Psychology 107 (2): pp. 349–354.
Harvey, A., Watkins, E., Mansell, W. and Shafran, R. (2004) Cognitive behavioural process across psychological disorders: A transdiagnostic approach to research and treatment. Oxford: Oxford University Press.
Haslam, N. and Beck, A. T. (1994). Subtyping major depression: A taxometric analysis. Journal of Abnormal Psychology 103(4): pp. 686–692. Available at: https://doi.org/10.1037/0021https://psycnet.apa.org/doi/10.1037/0021https://psycnet.apa.org/doi/10.1037/0021-843X.103.4.686][843X.103.4.686843X.103.4.686 (Accessed 9th January 2020).
Hayes, S. C., Luoma, J. B., Bond, F. W., Masuda, A. and Lillis, J. (2006) Acceptance and commitment therapy: model, processes and outcomes. Behaviour Research and Therapy 44(1): pp. 1–25.
Haynes, S. N., Richard, D. C. S. and Kubany, E. S. (1995) Content validity in psychological assessment: A functional approach to concepts and methods. Psychological Assessment 7(3): pp. 238–247.
Health Research Authority (HRA) (2015) East Midlands-Nottingham Research Ethics
Committee Guidance. Available at: https://www.hra.nhs.uk/about-us/committeeshttps://www.hra.nhs.uk/about-us/committees-and-services/res-and-recs/search-research-ethics-committees/east-midlands-nottingham-1/][andhttps://www.hra.nhs.uk/about-us/committees-and-services/res-and-recs/searchhttps://www.hra.nhs.uk/about-us/committees-and-services/res-and-recs/search-research-ethics-committees/east-midlands-nottingham-1/][research-ethics-committees/east-midlands-nottingham-1/services/res-and-recs/searchhttps://www.hra.nhs.uk/about-us/committees-and-services/res-and-recs/search-research-ethics-committees/east-midlands-nottingham-1/][research-ethics-committees/east-midlands-nottingham-1/ (Accessed 8th June 2020).
Henderson, D., Hargreaves, I., Gregory, S. and Williams, J. M. G. (2002) Autobiographical memory and emotion in a non-clinical sample of women with and without a reported history of childhood sexual abuse. British Journal of Clinical Psychology 41 (2): pp. 129 –141.
Hetherington, S. (2006) How to Know (that Knowledge — that is Knowledge — how). In: Hetherington, S. (Ed.) Epistemology Futures. Oxford: Clarendon Press, pp. 71–94.
Hill, J. (2009) Developmental perspectives on adult depression. Psychoanalytic Psychotherapy 23 (3): pp. 200–212.
Hollon, S. (2014) CBT treatment for depression. 2-day Masterclass 25th-26th May 2014. Charlie Waller Centre, University of Reading, England.
Hookway, C. (2006) Epistemology and Inquiry: Primacy of Practice. In: Hetherington, S. (Ed.) Epistemology Futures. Oxford: Oxford University Press, pp 95–110.
Hookway, C. (2002) Common Sense, Pragmatism and Rationality. In: Truth, Rationality and Pragmatism: Themes from Pierce. Oxford: Oxford University Press, pp. 198–222.
Hu, L.T. and Bentler, P.M. (1999) Cut off criteria for fit indexes covariance structure analysis: conventional criteria versus new alternatives. Structural Equation Modelling 6 (1): pp. 1–55 Available at: doi: 0.1080/107005519909540118 (Accessed 15TH July 2019).
Hu, L.T. and Bentler, P.M. (1998) Fit indices in covariance structure modelling: sensitivity to underparametized model misspecification. Psychological Methods, 3: pp. 424–453 Available at: doi:10.1037/1082-989X.3.4.424 (Accessed July 2019).
Hu, T., Zhang, D. and Yang, Z. (2015) Negative outcomes and depression: The relationship between attributional style for negative outcomes and depression: a meta-analysis. Journal of Social and Clinical Psychology 34 (4): pp. 304–321.
Huang, C. (2015) Relation between attributional style and subsequent depressive symptoms: A systematic review and meta-analysis of longitudinal studies. Cognitive Therapy and Research 39: pp. 721–735. Available at: DOI 10.1007/s10608-015-9700-x (Accessed 9TH May 2020).
Institute for Public Policy Research (IPPR) (2018) Better Health and Care for All: The Lord
Darzi Review of Health and Care Final Report. Available at: https://www.ippr.org/files/2018https://www.ippr.org/files/2018-06/better-health-and-carehttps://www.ippr.org/files/2018-06/better-health-and-care-for-all-june2018.pdf][for-all-june2018.pdf06/better-health-and-care-for-all-june2018.pdf (Accessed 15th June 2020).
International Classification of Diseases (ICD-10) (1994) Classification of Mental and Behavioural Disorders. World Health Organisation (WHO): Geneva.
Irons, C., Gilbert, P., Baldwin, M.W., Baccus, J.R. and Palmer, M. (2006) Parental recall, attachment relating and self-attacking/self-reassurance: their relationship with depression.
British journal of Clinical Psychology 45 (3): pp. 297–308.
Ishiyama, F. I. and Munson, P. A. (1993) Development and validation of a self-critical cognition scale. Psychological Reports 72(1): pp. 147–154. Available at: https://doi.org/10.2466/pr0.1993.72.1.147 (Accessed 2nd July 2020).
Izard, C.E. (1977) Human Emotions. New York: Plenum Press.
Jackson, D. L., Gillaspy, J. A., Jr. and Purc-Stephenson, R. (2009). Reporting practices in confirmatory factor analysis: An overview and some recommendations. Psychological Methods 14(1): pp. 6–23. Available at: https://doi.org/10.1037/a0014694 (Accessed 12th January 2019).
Jagacinski, C.M. and Nicholls, J.G. (1984) Conceptions of ability and related affects in task involvement and ego involvement. Journal of Educational Psychology 76 (5): pp. 909–919.
James, I.A., Morse, R. and Howarth, A. (2010) The science and art of asking questions in cognitive therapy. Behavioural and Cognitive Psychotherapy 38 (1): pp. 83–93.
Janoff-Bulman, R. (1979) Characterological versus Behavioural Self-blame: Inquiries into depression and rape. Journal of Personality and Social Psychology 37 (10): pp. 1798–1809.
Johnson, B. and Gray, R. (2010) A history of philosophical and theoretical issues for mixed methods research. In Tashakkori, A. and Teddlie, C. (Eds:) Sage Handbook of Mixed Methods in Social and Behavioural Research. Thousand Oaks, California: Sage Publications Inc., pp. 6994.
Jones, S.R., Carley, S. and Harrison, M. (2003) An introduction to power and sample size estimation. Emergency Medicine Journal 20 (5): pp. 453–458.
Kabat-Zinn, J. (2003) Mindfulness based interventions in context: past, present, future. Clinical Psychology Science and Practice 10 (2): pp. 144–156.
Kappas, A. (2001) A metaphor is a metaphor is a metaphor: exorcising the homunculus from appraisal theory. In: Scherer, K.R., Schorr, A. and T. Johnstone, T. (Eds.) Appraisal processes in Emotion: Theory, Methods, Research. New York: Oxford University Press, pp. 157–172.
Kaufman, G. (1974) The meaning of shame: toward a self-affirming identity. Journal of Counselling Psychology 21 (6): pp. 568–574.
Keller, M.B., Lavori, P.W., Lewis, C.E. and Klerman, G.L. (1983) Predictors of Relapse in Major Depressive Disorder. Journal of American Psychiatric Association 250 (24) pp. 3299–3304.
Kelly, A.C. and Dupasquier, J. (2015) Social safeness mediates the relationship between recalled parental warmth and the capacity for self-compassion and receiving compassion.
Personality and Individual Differences 89: pp. 157–16.
Kememny, M.E, Gruenewald, T.L. and Dickerson, S. (2004) Shame as the emotional response to threat to social self: implications for behaviour, physiology and health. Psychological Inquiry 15: PP. 153–160.
Kim, S., Thibodeau, R. and Jorgensen, R.S. (2011) Shame, guilt and depressive symptoms: A meta-analytic review. Psychological Bulletin 137 (1): pp. 68–96.
Kimberlin, C.L., Winterstein, A.G. (2008) Validity and reliability of measurement instruments used in research. American Journal of Health Systems Pharmacy 65 (23): pp. 2276–2284.
Kinsella, P. and Garland, A. (2008) Cognitive behavioural therapy for mental health workers: A beginner’s guide. London: Routledge.
Kirkby, J. (2017) Compassion interventions: The programmes, the evidence and implications for research and practice. Psychology and Psychotherapy: Theory, Research and Practice 90 (3): pp. 432–455.
Kirby, J. and Gilbert, P. (2017) The Emergence of Compassion Focused Therapies. In: Gilbert, P. (Ed.) Compassion: Concepts, Research and Applications. Routledge: London, pp: 258–285.
Klein, D.N., Harding, K., Taylor, E.B. and Dickstein, S. (1988) Dependency and self-criticism in depression: evaluation in a clinical population. Journal of Abnormal Psychology 97 (4): pp. 399–404.
Kline, P. (2000) The Handbook of Psychological Testing (2nd Ed.). London, Routledge.
Knox, J. (2013) ‘Feeling for’ and ‘feeling with’: developmental and neuroscientific perspectives on intersubjectivity and empathy. Journal of Analytical Psychology 58 (4): pp. 491–509.
Koestner, R., Zuroff, D.C. and Powers, T.A. (1991) Family origins of adolescent self-criticism and its continuity into adulthood. Journal of Abnormal Psychology 100 (2): pp. 191–197.
Kramer, M. (1983) The increasing prevalence of mental disorder: a pandemic threat. Psychiatric Quarterly 55 (2–3): pp 115–143.
Kroenke, K., Spitzer, R. and Williams, J.B.W (2001) The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine 16(9): pp. 606–613. Available at: doi:
10.1046/j.1525-1497.2001.016009606.x (Accessed 10th April 2012).
Kumlander, S., Lahtinen, O., Turunen, T. and Salmivalli, C. (2018) Two is more valid than one, but is six even better? The factor structure of the self-compassion scale (SCS). PLoS ONE 13
(12): e020770. Available at: https://doi.org/10.1371/journal.pone.0207706 (Accessed March 5th 2020).
Kupeli, N., Chilcot, J., Schmidt, U.H., Campbell, C. and Troop, N.A. (2012) A confirmatory factor analysis and validation of the forms of self-criticism/self-reassurance scale. British Journal of Clinical Psychology 52 (1): pp. 12–25.
Kupfer, D.J., Frank, E., Perel, J.M., Cornes, C., Mallinger, A.G., Thase, M.E., McEachran, A.B. and Grochocinski, V.J. (1992) Five-year outcome of maintenance therapies in recurrent depression. Archives of General Psychiatry 49 (10): pp. 769–773.
Kuyken, W. and Brewin, C.R. (1995) Autobiographical memory functioning in depression: The role of early adverse experiences. Journal of Abnormal Psychology 104 (4): pp. 585–591.
Kuyken, W. and Brewin, C. (1994) Intrusive memories of childhood abuse during depressive episodes. Behaviour, Research and Therapy 32 (5): pp. 525–528.
Kuyken, W., Byford, S., Taylor, R. S., Watkins, E., Holden, E., White, K., Barrett, B., Byng, R., Evans, A., Mullan, E., & Teasdale, J. D. (2008) Mindfulness-based cognitive therapy to prevent relapse in recurrent depression. Journal of Consulting and Clinical Psychology 76(6): pp. 966– 978. Available at: https://doi.org/10.1037/a0013786 (Accessed 9th February 2020).
Kuyken, W., Watkins, E., Holden, E., White, K., Taylor, R.S., Byford, S., Evans, A., Radford, S.,
Teasdale, J.D. and Dalgleish, T (2010) How does Mindfulness-based Cognitive Therapy Work? Behaviour, Research and Therapy 48(11) pp. 1105–1112. Available at: https://doi.org/10.1016/j.brat.2010.08.003 (Accessed 9th February 2020).
Langdridge, D. (2008) Phenomenology and critical social psychology: Directions and debates in theory and research. Social and Personality Psychology Compass 2(3): pp. 1126–1142. Available at: https://doi.org/10.1111/j.1751-9004.2008.00114.x (Accessed 12th February 2020).
Laxter, R.M. (1964a) Relation of real self-rating to mood and blame and their interaction in depression. Journal of Consulting and Clinical Psychology 28 (6): pp. 538–546.
Laxter, R.M. (1964b) Self-concept changes of depressive patients in general hospital treatment. Journal of Consulting and Clinical Psychology 28 (3): pp. 214–219.
Layden, M.A. Newman, C. F., Freeman, A., Eyers-Mors S. (1998) Cognitive therapy for borderline personality disorder. Journal of Cognitive Psychotherapy 12 (3): pp. 282–284.
Leary, M.R. (2007) How the self became involved in affective experience: three sources of self-reflective emotions. In: Tracy, J.L., Robins and June Price Tangney, J.P. (Eds.) The selfconscious emotions: Theory and Research. New York: Guilford Press, pp. 38–52.
Leary, M. R., Tate, E. B., Adams, C. E., Batts Allen, A., & Hancock, J. (2007) Self-compassion and reactions to unpleasant self-relevant events: The implications of treating oneself kindly.
Journal of Personality and Social Psychology 92 (5): pp. 887–904. Available at:
https://doi.org/10.1037/0022-3514.92.5.887 (Accessed 16th June 2014).
Leaviss, J. and Uttley, L. (2015) Psychotherapeutic benefits of compassion -focused therapy: an early systematic review. Psychological Medicine 45 (5): pp. 927–945. Available at: doi:10.1017/S0033291714002141 (Accessed 12th February 2020).
Lee, A.S. and Murray, R.M. (1998) The Long-Term outcome of Maudsley Depressives. British Journal of Psychiatry 153 (6): pp. 741–751.
Lepine J.P. and Briley, M. (2011) The Increasing Burden of Depression. Neuropsychiatric Disorders and Treatment 7 (1): pp. 3–7. Available at: doi: 10.2147/NDT.S19617 (Accessed 10th January 2020).
Lewis, H.B. (1971) Shame and Guilt in Neurosis. New York: International Universities Press.
Lewis, M. (2007) Self-conscious emotional development. In: Tracy, J.L., Robins, R.W. and Tangney, J.P. (Eds.) The self-conscious emotions: Theory and Research. New York: Guilford Press, pp. 134–152.
Lewis, M. (2000) Self-conscious emotions: embarrassment, shame, pride and guilt. In: Lewis, M. and Haviland-Jones, J.M. (Eds.) Handbook of Emotions. (2nd ed.) New York: Guilford Press, pp. 623–636.
Lewis, M. (1992) Shame: the exposed self. New York: The Free Press.
Lewis, M., Sullivan, M.W., Stanger, C. and Weiss, M. (1989) Self-development and selfconscious emotions. Child Development 60 (1): pp. 146–156.
Li, C. H. (2016) Confirmatory Factor Analysis with ordinal data: comparing robust maximum likelihood and diagonally weighted least squares. Behaviour Research Methods 48: pp. 936949. Available at: DOI: 10.3758/S13428-015-0619-7 (Accessed 15th July 2019).
Lickel, B., Schmader, T. and Spanovic, M. (2007) Group conscious emotions: the implications of others’ wrongdoings for identity and relationships. In: Tracy, J.L., Robins, R.W. and Tangney, J.P. (Eds.) The self-conscious emotions: Theory and Research. New York: Guilford Press, pp. 351–370.
Lieberman, M. D., Gaunt, R., Gilbert, D. T. and Trope, Y. (2002) Reflexion and reflection: A social cognitive neuroscience approach to attributional inference. In Zanna, M.P. (Ed.) Advances in experimental social psychology. Volume 34. Cambridge: Massachusetts:
Academic Press, pp. 199–249. Available at: https://doi.org/10.1016/S0065-2601(02)80006-5 (Accessed 20th January 2020).
Lindisfarne, N. (1998) Gender, shame and culture: an anthropological perspective. in Gilbert, P. and Andrews, B. (Eds.) Shame: interpersonal behaviour, psychopathology and culture. Oxford: Oxford University Press, pp 246–260.
Linehan M. (1993) Cognitive-behavioural treatment of borderline personality disorder. New York: Guilford Press.
Liu, R.T., Alloy, L.B., Abramson, L.Y., Iacoviello, B.M., and Whitehouse, W.G. (2009) Emotional maltreatment and depression: prospective prediction of depressive episodes. Depression and Anxiety 26 (2): pp. 174–181.
López, A., Sanderman, R., Smink, A., Zhang, Y., van Sonderen, E., Ranchor, A. and Schroevers, M.J. (2015) A Reconsideration of the Self-Compassion Scale’s Total Score: Self-Compassion versus Self-Criticism. PLoS ONE 10(7): e0132940. doi:10.1371/journal. pone.0132940. (Accessed 16TH February 2020).
Lowe, B., Spitzer, R.L., Grafe, K., Kroenke, K., Quenter, A., Zipfel, S., Buchholz, C., Witte, S.,
Herzog, W., (2004) Comparative validity of three screening questionnaires for DSM-IV depressive disorders and physicians’ diagnoses. Journal of Affective Disorders 78 (2): pp. 131140.
Luyten, P., Sabbe, B., Blatt, S.J., Meganck, S., Jansen, B., De Grave, C., Maes, F. and Corveleyn, J. (2007) Dependency and self-criticism: relationship with major depressive disorder, severity of depression, and clinical presentation. Depression and Anxiety 24 (8): pp. 586–596.
Ma, H. and Teasdale, J.D. (2004) Mindfulness based cognitive therapy for depression: replication and exploration of differential relapse prevention effects. Journal of Consulting and Clinical Psychology 72 (1): pp. 31–40. Available at: DOI:10.1037/0022-006X.72.1.31 (Accessed 20th January 2020).
MacBeth, A. and Gumley, A. (2012) Exploring compassion: A meta‐analysis of the association between self‐compassion and psychopathology. Clinical Psychology Review 32 (6): pp. 545 – 552. Available at: DOI: 10.1016/j.cpr.2012.06.003 (Accessed April 2016).
Maccoby, E.E. (1959) Role-taking in childhood and its consequences for social learning. Childhood Development 30 (2): pp. 239–252.
Macmillan Education Limited (2009–2020) Online dictionary. Available at: https://www.macmillandictionary.com/ (Accessed 18th November 2019).
McAllister-Williams, R.H., Christmas, D.M.B., Cleare, J.A., Currie. A., Gledhill, J., Insole, L., Malizia, A.L., McGeever, M., Morriss, R., Robinson, L.J., Scott, M., Stokes, P.R.A., Talbot, P.S. and Young, A.H. (2018) Multiple-therapy-resistant major depressive disorder: a clinically important concept. British Journal of Psychiatry 212 (5): pp. 274–278. Available at: doi:
10.1192/bjp.2017.33 (Accessed 11th January 2020).
McCullough, J.P. (2000) Treatment for Chronic Depression: Cognitive Behavioural Analysis System of Psychotherapy. Guilford Press: New York.
McDonald, R. P. and Ho, M.-H. R. (2002) Principles and practice in reporting structural equation analyses. Psychological Methods 7(1): pp. 64–82. Available at: https://doi.org/10.1037/1082-989X.7.1.64 (Accessed on 15th July 32019).
Maltby, J., Williams, G., McGarry, J. and Day, L. (2010) Research Methods for Nursing and Healthcare. Harlow: Prentice Hall.
Malterud, K. (2001) Qualitative research: standards, challenges, and guidelines. Lancet 358 (9280): pp. 483–488.
Marsh, H.W., Morin, A.J.S., Parker, P.D. and Kaur, G. (2014) Exploratory structural equation modelling: An integration of the best features of exploratory and confirmatory factor analysis. Annual Review of Clinical Psychology 10 (1): pp. 85–110.
Marks, I.M. (1981) Cure and Care of Neurosis. New York: Wiley.
Markus, H. and Nurius, P. (1986) Possible Selves. American Psychologist 41 (9): pp. 954–969.
Matos, M. and Pinto-Gouveia, J. (2010) Shame as a traumatic memory. Clinical Psychology and Psychotherapy 17 (4): pp. 299–312.
Matos, M., Pinto-Gouveia, J. and Costa, V. (2013) Understanding the importance of attachment in shame traumatic memory relation to depression: The impact of emotion regulation processes. Clinical Psychology and Psychotherapy 20 (2): pp. 149–165.
Matos, M., Pinto-Gouveia, J. and Duarte, AC. (2012) Above and beyond emotional valence: the unique contribution of central and traumatic shame memories to psychopathological vulnerability. Memory 20 (5): pp. 461–477.
Matos, M., Pinto‐Gouveia, J., Gilbert, P., Duarte, C. and Figueiredo, C. (2015) The Other As Shamer Scale-2: Development and validation of a short version of a measure of external shame. Personality and Individual Differences 74: pp. 6–11.
Mayberg, H.S. (2014) Neuroimaging and Psychiatry: The Long Road from Bench to Bedside. Hastings Center Report. In: Johnston, J. and Perens, E. (Eds.) Special issue: Interpreting neuroimaging: an introduction to the technology and its limits. 22 (s2): pp. s31-36. Available at: https://doi.org/10.1002/hast.296 (Accessed 16th January 2020).
Merriam-Webster Dictionary (2020) Online dictionary. Available at:
https://www.merriamhttps://www.merriam-webster.com/webster.com/ (Accessed 17th March
2020).
Mikulincer, M., Shaver, P. R., Gillath, O. and Nitzberg, R. A. (2005). Attachment, caregiving, and altruism: Boosting attachment security increases compassion and helping. Journal of Personality and Social Psychology 89(5): pp. 817–839. Available at: https://doi.org/10.1037/0022-3514.89.5.817 (Accessed 23rd February 2020).
Mihailova, L. and Jobson, L. (2018) Association between intrusive negative autobiographical memories and depression: a meta-analytic investigation. Clinical Psychology and Psychotherapy 25 (5): pp. 509–524.
Moore, R.G. and Garland, A. (2003) Cognitive therapy for chronic and persistent depression. Chichester: Wiley.
Morriss, R. (2012) National Institute Health Research (NIHR): CLAHRC-NDL Mood Disorder RCT treatment protocol version 9. (trial registration: NCT01047124) (REC reference#: 09/H0405/42), pp: 1–47. University of Nottingham.
Morriss, R., Garland, A., Nixon, N., Boliang Guo., James, M., Kaylor-Hughes., C., Moore, R., Ramana, A., Sampson, C., Sweeney, T. and Dalgleish, T. (2016) Efficacy and cost effectiveness of a specialist depression service versus specialist mental healthcare to manage persistent depression: a randomised controlled trial. The Lancet Psychiatry 3 (9): pp. 821–831.
Morriss, R., Martunnen, S., Garland, A., Nixon, N., McDonald, R., Sweeney, T., Flambert, H., Fox, R., Kaylor-Hughes, C., James, M. and Yang, M., (2010) Randomised controlled trial of the clinical and cost effectiveness of a specialist team for managing refractory unipolar depressive disorder. BMC Psychiatry 10:100. Available at: doi 10.1186/1471-244x-10-100 (Accessed 16th June 2012).
Morse, J.M. (1991) Approaches to Qualitative-Quantitative Methodological Triangulation. Nursing Research 40 (2): pp. 120-123.
Moussavi, S., Chatterji, S., Verdes, E., Tandon, A., Patel, V. and Ustun, B. (2007) Depression, chronic diseases, and decrements in health: results from the World Health Surveys. The Lancet 370 (9590): pp. 851–858.
Mowrer, O.H. (1950) Learning Theory and Personality Dynamics. New York: Roland Press.
Muris, P. and Meesters, C. (2014) Small or big in the eyes of the other: on the developmental psychopathology of self-conscious emotions as shame, guilt and pride. Clinical Child and Family Psychology Review 17: pp. 19–40. Available at: DOI 10.1007/s10567-013-0137-z (Accessed 23rd May 2016).
Muris, P., Otgaar, H. and Petrocchi, N. (2016) Protection as the mirror image of psychopathology: Further critical notes on the self-compassion scale. Mindfulness 7: pp. 787790. Available at: DOI 10.1007/s12671-016-0509-9 (Accessed 18th February 2020).
Muris, P. and Petrocchi, N. (2017) Protection or vulnerability? A metanalysis of the relations between the positive and negative components of self-compassion and psychopathology. Clinical Psychology and Psychotherapy 24 (2): pp. 373–383. Available at: doi:10.1002/CPP.2005 (Accessed 18th February 2020).
Murphy, J.A., Sarris, J. and Byrne, G.J. (2017) A Review of the Conceptualisation and Risk
Factors Associated with Treatment Resistant Depression. Depression Research and
Treatment (Article ID 4176825 10 pages). Available at: https://doi.org/10.1155/2017/4176825 (Accessed January 9th 2020).
Muthén, L.K. and Muthén, B.O. (1998–2012). Mplus User’s Guide. Seventh Edition. Los Angeles, California: Muthén & Muthén.
National Institute for Health and Clinical Excellence (NICE) (2009) Depression in adults: recognition and management Clinical Guideline 90. (last updated April 2018). Available at:
https://www.nice.org.uk/guidance/CG90 (Accessed 18th June 2018).
National Institute for Health and Clinical Excellence (NICE) (2004) Depression in adults: recognition and management Clinical Guideline 23. Available at: https://www.nice.org.uk/guidance/cg23 (Accessed 18th June 2018).
National Institute for Health Research (NIHR) (2019) Research Participant Experience Survey Report 2018–19. Available at: https://www.nihr.ac.uk/documents/researchhttps://www.nihr.ac.uk/documents/research-participant-experience-survey-report-2018-19/12109][participanthttps://www.nihr.ac.uk/documents/research-participant-experience-surveyhttps://www.nihr.ac.uk/documents/research-participant-experience-survey-report-2018-19/12109][report-2018-19/12109experience-survey-report-2018-19/12109 (Accessed 16th January
2020).
National Institute for Health Research (NIHR) (2011) 1-day training event: Introduction to Good Clinical Practice (GCP): A practical guide to ethical and scientific quality standards in clinical research. Wednesday 14th December, University of Nottingham. CLAHRC-NDL.
Neff, K.D. (2016a) The self-compassion scale is a valid and theoretically coherent measure of self-compassion. Mindfulness 7: pp. 264–274. Available at: doi.org/10.1007/s12671-015https://doi.org/10.1007/s12671-015-0479-3][0479https://doi.org/10.1007/s12671-015-0479-33 (Accessed February 2020).
Neff, K.D. (2016b) Does Self-Compassion Entail Reduced Self-judgement, Isolation and Overidentification? A response to Muris, Otgaar and Petrocchi. Mindfulness 7: pp. 791–797.
Available at: https://link.springer.com/article/10.1007/s12671-016-0531-y (Accessed February 2020).
Neff, K. (2004) Self-compassion and psychological wellbeing. Constructivism in the human sciences 9 (2): pp. 27–37.
Neff, K.D. (2003a) Self-compassion: an alternative conceptualisation of a healthy attitude toward oneself. Self and Identity 2 (2): pp. 85–101.
Neff, K.D. (2003b) The development and validation of a scale to measure self-compassion. Self and Identity 2 (3): pp. 223–250.
Neff, K.D. and Germer, C.K. (2013) A pilot study and randomized controlled trial of the mindful self-compassion program. Journal of Clinical Psychology 69 (1) pp. 28–44 Available at: https://doi.org/10.1002/jclp.21923 (Accessed 25th February 2020).
Neff, K.D. and Germer, C.K. (2012) An introduction to mindful self-compassion: A five-day retreat at Samye Ling Buddhist Monastery, Holy Isle, Scotland, June 4–8th June 2012. Compassionate Mind Foundation.
Neff, K.D., Kirkpatrick, K.L. and Rude, S.S. (2007) Self-compassion and adaptive psychological functioning. Journal of Research and Personality 41: pp. 139–154.
Neff, K.D. and Pommier, E. (2013) The relationship between self-compassion and other focused concern among college undergraduates, community adults and practising mediators. Self and Identity 12 (2): pp 160–176.
Neff, K.D., Toth-Kiraly, I. and Colosimo, K. (2018) Self-compassion is best measured as a global construct and is overlapping but distinct from neuroticism: a response to Pfattheicher, Geiger, Hartung, Weiss and Schindler (2017). European Journal of Personality 32 (4): pp. 371–392. Available at: doi.org/10.1002/per.2148 (Accessed 18th February 2020).
Neff K.D. and Vonk R. (2009) Self-compassion versus global self-esteem: two different ways of relating to oneself. Journal of Personality 77 (1): pp. 23–50. Available at:
https://doi.org/10.1111/j.1467-6494.2008.00537.x (Accessed 23rd November 2019).
Neff, K.D., Whitaker, T.A. and Karl, A. (2017) Examining the factor structure of the selfcompassion scale in four distinct populations: Is the use of the total scale score justified?
Journal of Personality Assessment 99(6): pp. 596–607. Available at: https://doi.org/10.1080/00223891.2016.1269334 (Accessed 18th February 2020).
Nesse, R.M. (1990) Evolutionary explanations of emotions. Human Nature 1: pp. 261–289.
Nemeroff, C.B. (2007) Prevalence and management of treatment resistant depression. Journal of Clinical Psychiatry 68 (8): pp.17–25.
Niedenthal, P.M., Tagney, J.P. and Gavanski, I. (1994) ‘If only I weren’t’ versus ‘If only I hadn’t’: distinguishing shame from guilt in counterfactual thinking. Journal of Personality and Social Psychology 67(4): pp. 585–595.
Nietzel, M. and Harris, M. (1990) Relationship of dependency and achievement/autonomy to depression. Clinical Psychology Review 10 (3): pp. 279–297.
Nolen-Hoeksema, S. (2000) The role of rumination in depressive disorders and mixed anxiety/depressive symptoms. Journal of Abnormal Psychology 109 (3): pp. 504–511.
Nursing and Midwifery Council (NMC) (2018) The Code: Professional Standards of Practice and Behaviours for Nurses, Midwives and Nursing Associates. Available at: [[https://www.nmc.org.uk/][https://www.nmc.org.uk]][[https://www.nmc.org.uk/][/]][[https://www.nmc.org.uk/][ ]]
Nystrom, S. (1979) Depressions: factors related to 10-year prognosis. Acta Psychiatrica Scandinavica 60 (2): pp. 225–238.
Office of National Statistics (ONS) (2009) Adult Psychiatric Morbidity in England-2007: results of a household survey Available at: https://digital.nhs.uk/ (Accessed 15th January 2020).
Onwuegbuzie, A.J. and Johnson, R.B. (2006) The validity issue in mixed research. Research in the Schools 13 (1): pp. 48–63. Available at: http://www.msera.org/ (Accessed 11th June 2020).
Papageorgiou, C. and Wells, A. (2003) An empirical test of clinical metacognitive model of rumination and depression. Cognitive Therapy and Research 27 (3): pp 261–273.
Parker, G., Manicavasagar, V., Crawford, J. O., Tully, L., & Gladstone, G. (2006). Assessing personality traits associated with depression: The utility of a tiered model. Psychological Medicine 36 (8): pp. 1131–1139. Available at: https://doi.org/10.1017/S0033291706007562 (Accessed 23rd November 2019).
Patton, G.G., Coffey, C., Posterino, M., Carlin, J.B., and Wolfe, R. (2001) Parental ‘affectionless control’ in adolescent depressive disorder. Social Psychiatry and Psychiatric Epidemiology 36: pp. 475–480.
Paul, L. (1970). The cruel inner critic. Psychotherapy: Theory, Research and Practice 7(3): pp. 178–180.
Pauley, G. and McPherson, S. (2010) The experience and meaning of compassion for individuals with depression and anxiety. Psychology and Psychotherapy: Theory, Research and Practice 83 (2): pp. 129–143.
Paykel, E.S. (1971) Classification of depressed patients: cluster analysis derived groupings. British Journal of Psychiatry 118 (544): pp. 275–288.
Paykel, E.S., Scott, J., Teasdale, J.D., Johnson, A.L., Garland, A., Moore, R., Jenaway, A., Cornwall, P.L., Hayhurst, H., Abott, R. and Pope, M. (1999) Prevention of relapse in residual depression by cognitive therapy: A controlled trial. Archives of General Psychiatry 56 (9): pp. 829–835.
Peselow, E. D., Robins, C., Block, P., Barouche, F. and Fieve, R. R. (1990). Dysfunctional attitudes in depressed patients before and after clinical treatment and in normal control subjects. The American Journal of Psychiatry 147(4): pp. 439–444.
Peter, J.P. (1981) Construct validity: a review of basic issues and marketing practices. Journal of marketing Research, 18 (1): pp. 133–145. Available at: https://doi.org/10.1177%2F002224378101800201 (Accessed July, 2019).
Peterson, C., Schwartz, S.M. and Seligman, M.E.P. (1981) Self-blame and depressive symptoms. Journal of Personality and Social Psychology 42 (2): pp. 253–259.
Pfattheicher, S., Geiger, M., Hartung, J., Weiss, S. and Schindler, S. (2017) Old wine in new bottles? The case of self-compassion and neuroticism. European Journal of Personality 31 (2): pp. 160–169.
Phillips, A.G. and Silvia, P.J. (2005) Self-awareness and the emotional consequences of selfdiscrepancies. Personality and Social Psychology Bulletin 31 (5): pp. 703–713.
Pinto-Gouveia, J., Castilho, P., Matos, M. and Xavier, A. (2013) Centrality of shame memories and psychopathology: the mediator effect of self-criticism. Clinical Psychology: Science and Practice 20 (3): pp. 323–334.
Price, J., Sloman, L., Gardner, R., Gilbert, P. and Rohde, P. (1994) The Social Competition Hypothesis of Depression. British Journal of Psychiatry 164: pp. 309–315.
Raby, K.L., Lawler, J.M., Shlafer, R.J. Hesemeyer, P.S., Collins, A.W. and Sroufe, A.L. (2015) The interpersonal antecedents of supportive parenting: A prospective, longitudinal study from infancy to adulthood. Developmental Psychology 51 (1): pp. 115–123.
Raes, F., Hermans, D., Williams, J. M. G., Beyers, W., Eelen, P., & Brunfaut, E. (2006). Reduced autobiographical memory specificity and rumination in predicting the course of depression. Journal of Abnormal Psychology 115(4): pp. 699–704. Available at: doi:10.1037/0021843X.115 (Accessed 25th May 2020).
Reise, S.P., Bonifay, W.E. and Haviland, M.G. (2013) Scoring and modelling psychological measures in the presence of multidimensionality. Journal of Personality Assessment 95 (2): pp. 129–140. Available at: https://doi.org/10.1080/00223891.2012.725437 (Accessed 6th June 2020).
Rhebergen, D., Beekman, A.T.F., de Graaf, R., Nolen, W.A., Spijker, J., Hoogendijk, W.J. and Penninx, B.W.J.H. (2010) Trajectories of recovery of social and physical functioning in major depression, dysthymic disorder and double depression: a three year follow up. Journal of Affective Disorders 124 (1–2): pp. 148–156.
Robins, R.W., Norem, J.K. and Cheek, J.M. (1999) Naturalising the self. In: Pervin., L.A. and John, O.P. (Eds.) Handbook of Personality: Theory and Research. (2nd ed.). New York: Guilford Press, pp. 443–477.
Robinson, M.S. and Alloy, L.B. (2003) Negative cognitive styles and stress reactive rumination interact to predict depression: a prospective study. Cognitive Research and Therapy 27 (3): pp. 275–292.
Roe, C. and Garland, A. (2011) The use of poetry in the construction of meaning in cognitive behavioural psychotherapy and mental health studies. Mental Health Review Journal 16 (3) pp. 93–101. Available at: https://doi.org/10.1108/13619321111178032 (Accessed 15th March 2020).
Rogers, C.R. (1979) The Foundations of the Person-Centred Approach. Education 100 (2): pp. 98–107.
Rosebrock, L.E., Arditte Hall K.A., Rando, A., Pineles, S.L. and Liverant, G.I. (2019) Rumination and its relationship with thought suppression in unipolar depression and co-morbid PTSD.
Cognitive Therapy and Research 43: pp. 226–235. Available at:
https://doi.org/10.1007/s10608https://doi.org/10.1007/s10608-018-9935-4018-9935-4 (Accessed 18th February 2020).
Roseman, I.J. (1991) Appraisal determinants of discrete emotions. Cognition and Emotion 5 (3): pp. 161–200.
Rush, A., Madhukar, M.D., Trivedi, M.H., Wisniewski, S.R., Nierenberg, A.A., J.W., Warden, D.,
Niederehe, G., Thase, M.E. Lavori, P.W., Lebowitz, B.D., McGrath, P.J., Rosenbaum, J.F., Sackeim, H.A., Kupfer, D.J., James, L. J. and Fava, M. (2006) Acute and Longer-Term Outcomes in Depressed Outpatients Requiring One or Several Treatment Steps: A STAR*D Report. American Journal of Psychiatry 163: pp. 1905–1917.
Ryle, G. (1971) ‘Knowing How and Knowing That’. Collected Papers, vol. II. London: Hutchinson, pp. 212–25.
Ryle, A. and Kerr, I. B. (2002) Introducing cognitive analytic therapy: principles and practice. Chichester: John Wiley.
Safran, J. and Segal, Z. (1996) Interpersonal process in cognitive therapy. Northvale, New Jersey: Jason Aronson Inc.
Saggino, A., Carlucci, L., Sergi, M.R., D’Ambrosio, I., Fairfield, B., Cera, N. and Balsamo, M.
(2017) A validation study of the psychometric properties of the Other as Shamer Scale-2. SAGE Open 2 (7): pp 1–10. Available at: https://doi.org/10.1177%2F2158244017704241 (Accessed 16th June 2020).
Salkovskis, P.M. (2002) Empirically Grounded Clinical Interventions: Cognitive-behavioural therapy progresses through a multidimensional approach to clinical science. Behavioural and Cognitive Psychotherapy 30 (1): pp: 3–9.
Schermelleh-Engels, K., Moosbrugger, H. and Muller, H. (2003) Evaluating the fit of structural equation models: tests of significance and descriptive goodness of fit measures. Methods of Psychological Research 8 (2): pp. 23–74.
Schramm, E., Schneider, D. and Zobel, I., Van Kalker, D., Dykierek, P., Kech, S., Harter, M. and Berger, M. (2008) Efficacy of Interpersonal Psychotherapy plus pharmacotherapy in chronically depressed patients. Journal of Affective Disorders 109 (1–2): pp. 67–73.
Schreiber, J.B., Nora, A., Stage, F.K., Barlow, E.A. and King, J. (2006) Reporting structural equation modelling and confirmatory factor analysis results: A review. The Journal of Educational Research 99 (6): pp. 323–338. Available at: DOI: 10.3200/JOER.99.6.323-338 (Accessed 1st July 2019).
Schwartz, N. and Clore, G.L. (2003) Mood as information. Psychological Inquiry 14 (3–4): pp.296–303. Available at: https://doi.org/10.1080/1047840X.2003.9682896 (Accessed 23rd May 2020).
Scott, K.M., Bruffaerts, R., Tsang, a., Ormel, J., Alonos, J., Angermeyer, M.C., Benjet, C.,
Bromet, E., de Girolamo, G. de Graaf, R., Gasquet, I., Gureje, O.,Haro, J.M., He, Y., Kessler, R.C., Levinson, D., Mneimneh, Z.N., Oakley-Browne, M.A., Posada-Villa, J., Stein, D.J., Takeshmia, T. and Von Korff, M. (2007) Depression-anxiety relationships with chronic physical conditions: Results from the World Mental Health surveys. Journal of Affective Disorders 103 (1–3): pp. 113–120.
Seligman, M.E.P. (1975) Helplessness: on depression, development and death. San Francisco: Freeman.
Seligman, M.E.P. (1973) Fall into helplessness. Psychology Today 7: pp. 43–48.
Seligman M.E., Abramson L.Y., Semmel A. and von Baeyer C. (1979) Depressive attributional style. Journal of Abnormal Psychology 88 (3): 242–247.
Simpson, A., Jones, J., Barlow, S., Cox, L. and Service User and Carer Group Advising on Research (SUGAR) (2014) Adding SUGAR: service user and carer collaboration in mental health nursing research. Journal of Psychosocial Nursing and Mental Health Services 52 (1): pp. 22–30.
Smart, L. M., Peters, J. R. and Baer, R. A. (2015). Development and validation of a measure of self-critical rumination. Assessment 23 (3): pp. 321–332. Available at: https://doi.org/10.1177/1073191115573300 (Accessed 18th June 2020).
Smith, J.A. (2004) Reflecting on the development of interpretative phenomenological analysis and its contribution to qualitative research in psychology. Qualitative Research in Psychology 1 (1): pp. 39–54.
Smith, J.A. (1996) Beyond the divide between cognition and discourse: using interpretative phenomenological analysis in health psychology. Psychology and Health 11 (2): pp. 261–271.
Smith, J.A., Flowers, P. and Larkin, M. (2009) Interpretative Phenomenological Analysis: Theory, Methods, Research. Sage Publications: London.
Smith, C.A. and Lazarus, R.S. (1993) Appraisal components, core relational themes and the emotions. Cognition and Emotion 7 (3–4): pp. 233–269.
Solomon, D.A., Keller, M.B., Leon, A.C., Mueller, T.I., Lavori, P.W., Shea, T., Coryell, W., Warshaw, M., Turvey, C., Maser, J.D. and Endicott, J. (2000) Multiple recurrences of major depressive disorder. American Journal of Psychiatry 157: pp. 229–233.
Spasojevic, J. and Alloy, L.B. (2001) Rumination as a common mechanism relating to depressive risk factors to depression. Emotion 1 (1): pp. 25–37.
Spikins, P. (2017) Prehistoric origins: the compassion of far distant strangers. in Gilbert, P.
(Ed.) Compassion: Concepts, Research and Applications. Routledge: London, pp. 16–30. Sprecher, S. and Fehr, B. (2005) Compassionate love for close others and humanity. Journal of Social and Personal Relationships 22 (5): pp. 629–651.
Sroufe, L.A. (2005) Attachment and development: a prospective longitudinal study from birth to adulthood. Attachment and Human Development 7 (4): pp. 349–367.
Stata Corps. (2013) Stata Statistical Software: Release 13. College Station, Texas: StataCorp LP.
Steinmetz, H. (2015) Factor Loading in SEM. Senior researcher, Leibniz Institute for Psychology Information (ZPID) in Trier/Germany. Verified email at leibniz-psychology.org. Available at: https://stats.stackexchange.com/questions/148618/ (Accessed March 2020).
Strauss, C., Lever-Taylor, B., Gu, J., Kuyken, W., Baer, R., Jones, F. and Cavanagh, K. (2016) What is compassion and how can we measure it? A review of definitions and measures. Clinical Psychology Review 47: pp. 15–27.
Sturman, E.D. and Mongrain, M. (2005) Self-criticism and major depression: an evolutionary perspective. British Journal of Clinical Psychology 44 (4): pp. 505–519.
Summerfield, D. (2006) Depression: epidemic or pseudo-epidemic? Journal of the Royal Society of Medicine 99: pp. 161–162.
Sweeney, P., Anderson, K. and Bailey, S. (1986) Attributional style in depression: a metaanalytic review. Journal of Personality and Social Psychology 50 (5): pp. 774–791.
Tangney, J.P. (1995) Shame and guilt in interpersonal relationships. In: Tangney, J.P. and Fischer, K.W. (Eds.) The self-conscious emotions: The psychology of shame, guilt, embarrassment and pride. New York: Guilford Press, pp. 114–139.
Tangney, J.P. (1991) Moral affect: The good, the bad, and the ugly. Journal of Personality and Social Psychology 61 (4): pp. 598–607.
Tangney, J.P. (1990) Assessing individual differences in proneness to shame and guilt: Development of the self-conscious affect and attribution inventory. Journal of Personality and Social Psychology 59 (1): pp. 102–111.
Tangney, J.P. and Dearing, R.L. (2002) Shame and Guilt. Guilford Press: New York
Tangney, J.P., Wagner, P.E., Fletcher, C. and Gramzow, R. (1992) Shamed into anger? the relation of shame and guilt to anger and self-reported aggression. Journal of Personality and Social Psychology 62 (4): pp. 669–675.
Tangney, J.P., Wagner, P. E. and Gramzow, R. (1992) Proneness to shame, proneness to guilt and psychopathology. Journal of Abnormal Psychology 101 (4): pp. 585–595.
Tangney, J.P; Wagner, P.E., Hill-Barlow, D., Marschall, D.E. and Gramzow, R. (1996) Relation of shame and guilt to constructive versus destructive responses to anger across the lifespan. Journal of Personality and Social Psychology 70 (4): pp. 797–809.
Tansella, M., Thornicroft, G., Barubi, C., Cipriani, A. and Saraceno, B. (2006) Seven criteria for improving effectiveness trials in psychiatry. Psychological Medicine 36 (5): pp. 711–720.
Teasdale, J.D. (1999) Metacognition, mindfulness and the modification of mood disorders. Clinical Psychology and Psychotherapy 6 (2): pp. 146–155.
Teasdale, J.D. and Barnard, P.J. (1993) Affect, Cognition and Change: remodelling depressive thought. Hove: Erlbaum.
Teasdale, J. D., Moore, R. G., Hayhurst, H., Pope, M., Williams, S., & Segal, Z. V. (2002) Metacognitive awareness and prevention of relapse in depression: Empirical evidence.
Journal of Consulting and Clinical Psychology 70(2): pp. 275–287. Available at: https://doi.org/10.1037/0022-006X.70.2.275 (Accessed 16th January 2020).
Teasdale, J. D., Taylor, R. and Fogarty, S. (1980) Effects of induced elation-depression on the accessibility of memories of happy and unhappy experiences. Behavior Research and Therapy 18 (4): pp. 339–346.
Thew, G.R., Gregory, J.D., Roberts, K. and Rimes, K.A. (2017) The phenomenology of selfcritical thinking in people with depression, eating disorders and in healthy individuals. Psychology and Psychotherapy: Theory, Research and Practice 90 (4): pp. 751–769. Available at:
https://doi.org/10.1111/papt.12137 (Accessed 20th May 2020).
Thompson, R. and Zuroff, D.C. (2004) The Levels of Self-criticism scale: comparative selfcriticism and internalised self-criticism. Personality and Individual Differences 36 (2): pp. 419–430.
Thompson, R. and Zuroff, D.C. (1999) Development of self-criticism in adolescent girls: roles of maternal dissatisfaction, maternal coldness and insecure attachment. Journal of Youth and Adolescence 28: pp. 197–210.
Tomkin, S.S. (1963) Affect, imagery and consciousness, vol. II: the negative affects: fear and anger. New York: Springer.
Tracy, J.L. and Robins, R.W. (2007a) The self in self-conscious emotions: a cognitive appraisal approach. In: Tracy, J.L., Robins, R.W. and Tangney, J.P. (Eds.) The self-conscious emotions: Theory and Research. New York: Guilford Press, pp. 3–20.
Tracy, J.L. and Robins, R.W. (2007b) The Nature of Pride. In: Tracy, J.L., Robins, R.W. and Tangney, J.P. (Eds.) The self-conscious emotions: Theory and Research. New York: Guilford Press, pp. 263–282.
Tracy, J.L. and Robins, R.W. (2006) Appraisal antecedents of shame and guilt: support for a theoretical model. Personality and Social Psychology Bulletin 32 (10): pp. 506–525.
Tracy, J.L. and Robins, R.W. (2004) Putting the self into self-conscious emotions: a theoretical model. Psychological Inquiry 15 (2): pp. 103–125.
Turner E.H., Matthews A.M., Linardatos E., Tell R. A. and Rosenthal R. (2008) Selective publication of antidepressant trials and its influence on apparent efficacy. New England Journal of Medicine 358: pp. 252–260.
University of Nottingham (2013a) Code of Research Conduct and Research Ethics version 4. March.
University of Nottingham (2013b) Policy and Guidance for the Safe Conduct of Fieldwork.
February. Available at:
https://www.nottingham.ac.uk/safety/documents/fieldworkhttps://www.nottingham.ac.uk/safety/documents/fieldwork-policy.pdfpolicy.pdf (Accessed 24th November 2019).
Ustan, T.B., Ayuso-Mateos, J.L., Chatterji, S., Mathers, C. and Murray, C.J.L. (2004) Global Burden of Disease Study. British Journal of Psychiatry 184 (5): pp. 386–392.
Vagos, P., Riberio da Silva, D., Brazao, N., Rijo, D. and Gilbert, P. (2016) Dimensionality and measurement invariance of the Other as Shamer Scale across diverse adolescent groups. Personality and Individual Differences 98: pp. 289–296.
Van Vilet, K.J. (2009) The role of attributions in the process of overcoming shame: a qualitative analysis. Psychology and Psychotherapy: Theory, Research and Practice 82 (2): pp. 137–152.
Vrticka, P., Favre, P. and Singer, T. (2017) Compassion and the brain. In: Gilbert, P. (Ed.) Compassion: Concepts, Research and Applications. Routledge: London, pp 120–134.
Watkins, E. R. and Moulds, M. L. (2009). Thought control strategies, thought suppression, and rumination in depression. International Journal of Cognitive Therapy 2(3): pp. 235–251.
Watkins, E., Mullan, E., Wingrove, R., Rimes, K., Steiner, H., Bathhurst, N., Eastman, R. and Scott, J. (2004) Rumination focused cognitive behaviour therapy for residual depression: phase II randomised controlled trial. British Journal of Psychiatry 199 (4) pp. 317–322.
Watkins, E. and Teasdale, J. D. (2004) Adaptative and maladaptive self-focus in depression. Journal of Affective Disorder 82 (1): pp. 1–8.
Watkins, E. and Teasdale, J. D. (2001) Rumination and overgeneral memory in depression: Effects of self–focus and analytic thinking. Journal of Abnormal Psychology 110 (2): pp. 353– 357.
Watkins, E., Teasdale, J. D. and Williams, J. M. G. (2000) Decentring and distraction reduce over general autobiographical memory in depression. Psychological Medicine 30 (4): pp. 911–920.
Wegner, D.M., Schneider, D.J., Carter, S. and White, T. (1987) Paradoxical effects of thought suppression. Journal of Personality and Social Psychology 53 (1): pp. 5–13.
Weiner, B., Graham, S. and Chandler, C. (1982) Pity, anger and guilt: an attributional analysis. Personality and Social Psychology Bulletin 8 (2): pp. 226–232.
Weishaar, M.E. (1993) Aaron T. Beck. In: Series Ed: Windy Dryden. Key Figures in Counselling and Psychotherapy Thousand Oaks, California: Sage Publications.
Wenzlaff, R.M. and Luxton, D.D. (2003) The role of thought suppression in depressive rumination. Cognitive Therapy and Research 27: pp. 293–308.
Wenzlaff, R. M., Rude, S.S. and West, L.M. (2002) Cognitive vulnerability to depression: The role of thought suppression and attitude certainty. Cognition and Emotion 16 (4): pp. 533– 548.
Westen, D. and Rosenthal, R. (2003) Quantifying construct validity: Two simple measures. Journal of Personality and Social Psychology 84(3): pp. 608–618. Available at: https://doi.org/10.1037/0022-3514.84.3.608 (Accessed 25th August 2019).
Whewell, P. (2002) Profound Desolation: the working alliance with dissociative patients in an NHS setting. In: Sinason, V. (Ed.) Attachment, Trauma and Multiplicity: Working with Dissociative Identity Disorder. Hove: Brunner-Routledge, pp. 166–176.
Whiteford, H.A., Degenhardt, L., Rehm, J., Baxter, A.J., Ferrari, A.J., Erskine, H.E., Charlson, F.J., Norman, R., Flaxman, A.D., Johns, N., Burstein, R., Murray C.J.L. and Vos, T. (2013) Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Diseases Study. 2010. Lancet 382 (9904): pp. 1540–1542. Available at:
http://dx.doi.org/10.1016/S0140-6736(13)61611.6 (Accessed 9th January 2020).
Wiles, N., Thomas, L., Abel, A., Ridgway, N., Turner, N., Campbell, J., Garland, A.,
Hollinghurst, S., Jerrom, B., Kessler, D., Kuyken, W., Morrison, J., Turner, K., Williams, C., Peters, T., and Lewis, G. (2013) Cognitive behavioural therapy as an adjunct to pharmacotherapy for primary care based patients with treatment resistant depression: results of the CoBalT randomised controlled trial. Lancet 381 (9864): pp. 375–84.
Williams, J. B. W. (1988). A structured interview guide for the Hamilton Depression Rating Scale. Archives of General Psychiatry 45 (8): pp. 742- 747.
Williams, J.B.W., Kobak, K. A., Bech, P., Engelhardt, N., Evans, K., Lipsitz, J., Olin, J., Pearson, J. and Kalali, A. (2008) The GRID-HAMD: standardization of the Hamilton Depression Rating Scale. International Clinical Pharmacology 23 (3): pp. 120–129. Available at: doi: 10.1097/YIC.0b013e3282f948f5 (Accessed 5TH September 2019).
Williams, J.M.G. (1997) Depression. In: Clark, D.M. and Fairburn, C.G. (Eds.) Science and Practice of Cognitive Behaviour Therapy. Oxford: Oxford University Press, pp: 259–284.
Williams, J.M.G. (1992) The Psychological Treatment of Depression: A guide to the theory and practice of cognitive behaviour therapy. (2nd ed.). London: Taylor Francis.
Williams, J. M. G., Barnhofer, T., Crane, C., Herman, D., Raes, F., Watkins, E. and Dalgleish, T.(2007) Autobiographical memory specificity and emotional disorder. Psychological Bulletin 133 (1): pp. 122–148.
Williams, J. M. G. and Broadbent, K. (1986). Autobiographical memory in suicide attempters. Journal of Abnormal Psychology 95 (2): pp. 144–149.
Williams, J.M.G., Dalgleish, T., Karl, A. and Kuyken, W. (2014) Examining the factor structures of the five facets of mindfulness questionnaire and the self-compassion scale. Psychological Assessment 26 (2): pp. 407–418.
Williams, J.M.G., Watts, F.N., MaCleod, C. and Mathews, A. (1997) Cognitive Psychology and Emotional Disorders. (2nd ed.) London: Wiley.
Willig, C. (2001) Qualitative research in psychology: A practical guide to theory and method. Buckingham: Open University Press.
Wilson, A.E. and Ross, M. (2001) From chump to champ: people’s appraisals of their earlier and present selves. Journal of Personality and Social Psychology 80 (4): pp. 572–584.
World Health Organization (2005) Handbook for good clinical research practice (GCP): guidance for implementation. World Health Organization. Available at: https://apps.who.int/iris/handle/10665/43392 (Accessed 25th June 2017).
World Medical Association (2004) World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. Ferney-le-Voltaire, France: World Medical Association.
Wright, N., Callaghan, P. and Bartlett, P (2011) Mental health service users’ and practitioners’ experiences of engagement in assertive outreach: a qualitative study. Journal of Psychiatric and Mental Health Nursing 18 (9) pp. 822–832. Available at:
https://doi.org/10.1111/j.1365https://doi.org/10.1111/j.1365https://doi.org/10.1111/j.1365–2850.2011.01733.x][2850.2011.01733.x2850.2011.01733.x (Accessed 23rd May 2020).
Wykes, T. and Callard, F. (2010) Diagnosis, diagnosis, diagnosis: towards DSM 5. Journal of Mental Health 19 (4): pp: 301–304.
Young, J.E. (1990) Cognitive Therapy for Personality Disorder: a schema focused approach. Sarasota, Florida: Professional Resources Exchange Inc.
Young, J. E., Klosko, J. S., & Weishaar, M. E. (2003). Schema therapy: A practitioner’s guide. New York: Guilford Press.
Zahn, R., Lythe, K.E., Gethin, J.A., Green, S., Deakin, J.F.W., Young, A.H. and Moll, J. (2015) The role of self-blame and worthlessness in psychopathology of major depressive disorder.
Journal of Affective Disorders 186: pp. 337–341.
Zajonc, R.B. (1980) Feeling and Thinking: Preferences Need No Inferences. American Psychologist 35 (2): pp. 151–175.
Zeltzer, J. (2016) Zstatistics: Regression output Explained. Available at: http://www.zstatistics.com/videos#/regression%20https://www.neura.edu.au (Accessed 19th August 2019).
Zeltzer, J. (2013) Zstatistics: Regression II: Degrees of Freedom Explained. http://www.zstatistics.com/videos#/regression%20https://www.neura.edu.au (Accessed 19th August 2019).
Zeltzer, J. (2011) Zstatistics: What is Regression?
http://www.zstatistics.com/videos#/regression%20https://www.neura.edu.au (Accessed 19th August 2019).
Zuroff, D.C., Igreja, I. and Mongrain, M. (1990) Dysfunctional Attitudes, dependency and selfcriticism as predictors of depressed mood states: a 12-month longitudinal study. Cognitive Therapy and Research 14: pp. 315–326.
Appendices
Appendix I: Continuum of Schools of Cognitive Behavioural Psychotherapies (adapted from Gilbert 2007b)
338
Appendix II: Table of summary of the biological, psychological, genetic and clinical correlates of Treatment Resistant Depression
(from Murphy, Saris and Byrne 2017 p. 4).
Biological
Activation of the inflammatory system
HPA axis disturbance
Dysfunctional neuroanatomic circuits (particularly the default mode network)
Abnormal neural activity
Neurotransmitter dysfunction
Clinical and psychosocial
Melancholic features
Frequent and recurrent episodes
Previous non-remission or partial remission
Long illness duration/chronicity
Prevalence of psychiatric co-morbidity
Bipolarity features
High number of stressful life events/trauma
Genetic
Involvement of polymorphisms in the 5-HTT promoter region (5HTTLPR) Interactions between BDNF and NTRK2 polymorphisms
Personality
Personality dysfunction
High neuroticism
Low extraversion, openness and conscientiousness High levels of social inhibition
BDNF, brain derived neurotrophic factor; NTRK2, neurotrophic tyrosine kinase receptor 2.
339
Appendix III: Proposed criteria for Multiple-Therapy-Resistant (MTR) Major Depressive Disorder
(from McAllister-Williams, Christmas, Cleare, Currie et al 2018 P 277).
The patient: diagnosed with MDD (using (DSM-5).24
Their depression: MDD of at least moderate severity.
Their treatment
(a) Psychotherapy. At least two trials of structured, evidence-supported psychological therapy.1 The trials should ideally each be of a different modality and provided by a different therapist. In both cases, the clinician should assure themselves that the patient has received a structured course of therapy delivered by an experienced therapist with whom the patient had a good therapeutic relationship. Ideally, at least one of the trials should have been of at least 16 hours duration and at least one trial should have been given in combination with pharmacotherapy.
(b) Antidepressants. Four adequate trials of antidepressants. There is little consensus with regards how antidepressants should be divided into different ‘classes’ and how important it is that drugs from different classes are trialled. However, it is recommended that the trials should not all be from the same class of drugs and that at least two trials are using antidepressants that are viewed as being potentially more efficacious in severe depression and/or compared with other antidepressants, for example as listed by BAP guidelines (clomipramine, venlafaxine (≥150[th]mg), escitalopram (20[th]mg), sertraline, amitriptyline or mirtazapine).2 We would also recommend consideration of a traditional MAOI (for example phenelzine), especially for patients with atypical symptoms.
(c) Pharmacological augmentation. At least two adequate trials of an evidence-based augmentation/combination agent given in combination with an antidepressant. Ideally these should both be agents listed as first-line options in BAP guidelines (lithium (ideally with a plasma level of 0.6–1.0[th]mmol/L), quetiapine and aripiprazole).2
(d) ECT. A trial of ECT (at least eight treatments, and ideally bilateral if tolerated). For all treatments: the requirement for a treatment may be waived if there is a recognised contraindication or the patient has, despite extensive discussions and the provision of information, declined it, or there have been well-documented adverse effects that have limited tolerability. This applies to ECT, psychotherapy and medication. Given evidence for possible greater efficacy of a structured psychological treatment in combination with medication,25,26 a period of combined treatment over a period of 9–15 months, is recommended.
340
Appendix IV: A theoretical process model of self-conscious emotions (Tracy and Robins 2007a p10)
Event
yes
341
Appendix V: Appraisal model of compassion illustrating how witnessing negative outcomes leads to felt compassion with moderation of relevance to self
(from Goetz, Keltner and Simon-Thomas 2010 p 356)
| <right> |
Is target deserving of help? |
342
Appendix VI: Theories of shame measured against Brawley’s (1993) Practicality of a theory criteria
| Theory of shame | Criteria 1 | Criteria 2 | Criteria 3 | Criteria 4 | Criteria 5 | Criteria 6 |
| Shame as an affect: |
Tangney (1995)
Tangney and Dearing
(2002) | Defining shame as a selfconscious emotion in contrast to a basic emotion | Five features of selfconscious emotions | Psychometric measures:
Test of Self-Conscious Emotions (TOSCA) versions 1,2,3. | Draws on evolutionary theory of emotions | Scenario based questionnaire measuring shame and guilt as defined in the theory. | Psychometric properties of TOSCA (all versions) tested student population
Theory not tested on clinical population
Theoretically used to inform psychoanalytic
Clinical formulations
No studies of clinical application |
| Cognitive-attributional theory of shame: |
Lewis (2000) | Shame as a self-conscious emotion which is a product
Of cognitive-attributional processes | 3 inter-connected
Cognitive-attributional processes:
SRG’s
Internal vs. external attributions Global vs. specific attributions | No psychometric measures developed
Uses observational data collection methods | Draws on research in:
V Developmental
psychology
V Causal attributions
V Cognitive
appraisal and emotions | V Attributions of
self V Socially derived Standards, Rules and
Goals
V Attributions of
causality
V Attributions of
Globality
V Behavioural
Disturbance | Theory tested on range of clinical populations of maltreated children
Using observational data collection methods
Not used to inform clinical interventions |
| Appraisal based process model of self-conscious emotions (Tracy and Robins 2007; 2006; 2204) | Shame as a self-conscious emotion as a product of a sequential appraisal process | A sequential |
appraisal process as follows:
V Survival goal
relevance
V Attentional focus on
self and activation of self-representations | | Draws on research from social-personality psychology in studies of self and emotions:
V Causal attributions and emotions | V Self-focus attention
V Representations of self
V Attributions of
causality
V Attributions of
controllability | Theory not yet tested |
| V | Cognitive |
appraisal and
emotions | | |
| 343 |
| V Identity goal- |
congruence
V Internality
attributions
V Stability, globality, controllability attributions | | V Cognitive antecedents to shame
Self-evaluative processes | V Attributions of
Globality
Depressive symptoms | Not used to inform clinical interventions |
| Evolutionary |
And biopsychosocial
Theory of shame
(Gilbert 2005; 2007a) | Shame as a phylogenetic
mechanism to regulate social rank and is an involuntary submissive response triggered by social threat which functions de-escalate conflict | 6 interconnected aspects:
V Humans have
innate motives for attachment
V Socio-cultural
context
V External shame
V Internal shame
V Humiliation
V Reflected
stigma
(to family or others) rejection by community | Psychometric measures:
Others as shamer scale
Forms of self-criticising/ self-
attack/selfreassurance scale | Draws on research from:
V evolutionary
biology
V evolutionary psychology
V evolutionary anthropology
emotion research | V External shame
V Self-
criticism/selfattack/selfreassurance
V Self-compassion | 1 study of Compassion Focused Therapy (CFT) to target shame and selfcriticism in a mixed clinical group | 344
Appendix VII: Consort diagram of participant flow through RCT
(from Morriss, Garland, Nixon, Boliang, et al, 2016)
Appendix VIII: Email invitation to participate as a healthy control in the study
Dear
Thank you for volunteering to take part as a healthy volunteer in our study of depression. I am contacting to ask if I can:
1. Make a time to speak on the phone to explain what the study involves and to collect some initial information
2. Make a time to meet to conduct the face to face interview
I was hoping to speak with you on…… for around 10 minutes. Please could you let me know if this is convenient and if there is a preferred time for me to contact you? If you have any questions about this, please don’t hesitate to contact me either by email or telephone: ………
Many thanks again for your help with this and I look forward to hearing from you.
With best wishes,
Anne Garland
Nurse Consultant in Psychological Therapies
CLAHRC Clinician & Researchers
Appendix IX: Healthy Controls: Screening Questionnaire Introduction and Background Information
“As you know I’m calling about a research project I’m conducting with the University of Nottingham. I’m exploring the role of shame, self-criticism and self-compassion in depression. To do this we are investigating peoples experience of depression within health services, and then comparing these to people without any current or past mental health problem. The purpose of your involvement is to provide this healthy comparison, so that differences between these two groups can be examined. This will involve meeting for around 90 minutes at a location of your choice. The first half of the meeting will involve asking you questions about your mental health, to ascertain that you are free of any mental health problems. The second part of the meeting will then consist of you completing a set of questionnaires, three related to symptoms of depression and three others related to shame, self-criticism and self-compassion.
The data you provide will be kept in a locked filing cabinet in a locked room and then destroyed once analysed. Our meeting will be recorded so that a colleague of mine can verify that my findings are accurate and reliable. This will also be stored to protect confidentiality as above.
Before arranging to meet it will be helpful to ask you some basic questions about your health, to check that I won’t be wasting your time by arranging to meet in person. Is this ok? Do you have any questions that you would like to ask?
I’m going to start just by getting some basic demographic details.”
Demographic Information Name:
Address:
DOB: Telephone: (landline): (mobile):
Gender: M/F: Marital Status: Race/ethnicity: Religion: Age left education:
I’m now going to ask you questions about your mental health…….”
Mental Health Status
“Have you ever had an episode of depression?”
“Have you ever been treated for a mental health problem?”
“Do you think you might have or have had a mental health problem in your life either treated or untreated?”
-
Depression, anxiety, panic, OCD, eating disorder, major phobias e.g. spiders, dogs, blood, heights, snakes, vomit?
Appendix X: Participant Information Sheet Study Title
Shame, Self-Criticism, Self-Compassion and Depression
Invitation to take part in the study
The researcher carrying out this study is Anne Garland. She is a mental health nurse by profession and works for Nottinghamshire Healthcare NHS Trust. Anne is employed as a consultant nurse in psychological therapies and her place of work is Nottingham Psychotherapy Unit, St. Ann’s House, 114 Thorneywood Mount, Nottingham, NG3 2PZ.
Before you decide to take part in the research study it is important that you understand why the research is being done and what it will involve.
Please take time to read the following information carefully and discuss it with others if you wish. Please take your time to decide whether or not you wish to take part in the research.
Thank you for taking the time to read this.
What is the purpose of the study?
Shame and self-criticism have been shown to contribute to the maintenance of depression and self-compassion has been proposed as something that can tackle the adverse effects of shame and self-criticism in depression.
The aim of this study is to recruit 10 people from both arms of the CLAHRC depression research project and invite them to take part in a one to one semi-structured interview to try and examine in greater depth their experience of depression, shame, self-criticism and selfcompassion and how these may influence the persons everyday life.
Why have I been approached about this research project?
You have been approached because you are already a participant in the CLAHRC-NDL depression research project. This small project being carried out by Anne Garland is part of the CLAHRC depression project and is part of a programme of study for her PhD.
Do I have to take part?
No, it is up to you whether or not you decide to take part. If you do decide to take part you will be given this information sheet to keep and asked to sign a consent form. If you decide to take part you will be free to withdraw at any time without giving a reason. A decision to take part, not take part or withdraw at any time will not affect the care and treatment you receive from Nottinghamshire Healthcare NHS Trust in any way. However, the information that has already been collected from you will not be destroyed and may still be used in the final analysis of the study.
What will happen to me if I take part?
If you decide to take part in this project you will be asked, on one occasion only, to take part in a 90-minute interview. The interview will take place at a time and place convenient to you. During the interview you will be invited through a process of questions and discussion to share your experiences, opinions and beliefs about depression. It is hoped that the information we gather will help researchers understand more fully the role of key factors believed to be responsible for maintaining episodes of. From this it is hoped we could develop and refine more effective psychological treatments to help people tackle their depression.
With your permission the interview will be audio recorded. The purpose of the recording is to ensure the information gathered in the interview is accurate and used to verify any written notes and identify common themes in the research.
Expenses and payments
A thank you gift to the value of £10.00 will be offered to you for taking part What are the possible advantages and disadvantages of taking part?
Your participation may help further our understanding of depression, potentially leading to improved treatment of this mental health problem.
There is some possibility that sharing your experiences of depression will give rise to feeling sad and upset. At the end of the interview there will be opportunity to discuss this with the interviewer and we will provide the necessary support should the need arise.
What happens if something goes wrong?
If you have any concerns about the study, you should speak to the researcher Anne Garland on 0115 8440517 who will do her best to answer your questions.
In the event that something does go wrong and you are harmed during the research, and this is due to someone’s negligence, then you may have grounds for a legal action for compensation against the University of Nottingham but you may have to pay your legal costs.
If you wish to make a formal complaint you can do this through the NHS complaints procedure. Details can be obtained through your GP surgery.
Will my taking part in the project be kept confidential?
All information which is collected about you during the course of the research will be kept strictly confidential, and any information about you which leaves the team will have your name and personal information removed so that you cannot be identified. The only exception to this is if you reveal that you, or anyone else, are at risk of harm because of how you are feeling. In this event, the researcher is obliged to break confidentiality to ensure your/others safety.
In order to analyse the data fully some of your therapy sessions and assessments may be audio taped or digitally recorded and then transcribed. Recordings will be held securely in a locked filing cabinet or as a password-protected, access-controlled, computer file. All recordings will be made completely anonymous so that there will be no indication of who any given quote belongs to. All the recordings will be destroyed once they have been transcribed.
The patient research file will only collect the minimum required information for the purposes of the study and will be held securely in a locked room, cupboard or cabinet. Access to the information will be limited to the research staff and relevant regulatory authorities. Computer held data, including the trial database, will be held securely and will be password protected. All data will be stored on a secure dedicated web server. Access will be restricted by user identifiers and passwords. Information about the trial in your medical records/hospital notes will be treated confidentially, in the same way as all other confidential medical information.
We will keep your data securely and confidentially for 7 years after the study has finished, in accordance with University of Nottingham regulations. We will only keep your personal contact details until the completion of the study.
Involvement of the General Practitioner/Family doctor (GP)
We will inform your family doctor if any details arise that may be relevant to my medical care.
What will happen to the results of the research study?
The results will be publicised through the extensive arrangements for dissemination locally within the University and the healthcare trust (through road shows, websites and annual conferences), as well as through publication in peer reviewed journals, local, national and international scientific conferences.
Who is organising and funding the research?
This study is part of a larger study which is funded by National Institute for Health Research and matched funding from NHS Trusts, the East Midlands Special Health Authority, the University of Nottingham and two local councils. The chief investigator is based at the University of Nottingham and the principle investigator (Anne Garland) is based at Nottingham Psychotherapy Unit.
Contact details:
Anne Garland
Nottingham Psychotherapy Unit……..
Appendix XI: Healthy Controls Participant Consent Form
Participant Consent Form
Title of study: Mood Disorder RCT – An evaluation of the psychometric properties of self-report measures of mindfulness, shame, self-criticism and self-compassion in a depressed population.
REC ref: 09/H0405/42
Name of Chief Investigator: Prof. Richard Morriss Name of Participant:
Please give your consent to participating in the study by answering the following questions and initialling the boxes.
1. I confirm that I have read and understand the information sheet (V.1) for the above study. I have had the opportunity to consider the information, ask questions and have had these answered satisfactorily
2. I understand that my participation is voluntary and that I am free to withdraw at any time, without giving any reason, and without my medical care or legal rights being affected. I understand that should I withdraw then the information collected so far cannot be erased and that this information may still be used in the project analysis
3. I give permission for my interviews and therapy sessions to be audio taped and transcribed. I understand that any quotes will be anonymous and I will not be identified and that the recordings will be destroyed following analysis
4. I understand that relevant data collected during the study may be looked at by authorised individuals from the University of Nottingham, the research group and regulatory authorities where it is relevant to my taking part in this study. I give permission for these individuals to have access to my records and to collect, store, analyse and publish (anonymised) information obtained from my participation in the study
5. I agree to my GP being informed if any details arise that may be relevant to my medical care
6. I agree to take part in the above study
Name of participant……………………………Signature……………………….Date………….
Name of researcher……………… Signature……………………….Date………......
Copy – 1 for patient, 1 for investigator site file, 1 in patient’s research file
Appendix XII: Other as Shamer Scale
(Allan, Gilbert and Goss, 1994)
Appendix: XIII: The Forms of Self-Criticising and Self-Reassuring Scale (FSCRS)
(Gilbert, Clarke, Hempel, Miles and Irons, (2004)
When things go wrong in our lives or don’t work out as we hoped, and we feel we could have done better, we sometimes have negative and self-critical thoughts and feelings. These may take the form of feeling worthless, useless or inferior etc. However, people can also try to be supportive of themselves. Below are a series of thoughts and feelings that people sometimes have. Read each statement carefully and circle the number that best describes how much each statement is true for you.
Please use the scale below.
Not at all A little bit Moderately Quite a bit Extremely like me like me like me like me like me 0 1 2 3 4
When things go wrong for me:
1. I am easily disappointed with myself. 0 1 2 3 4
2. There is a part of me that puts me down. 0 1 2 3 4
3. I am able to remind myself of positive 0 1 2 3 4
about myself
4. I find it difficult to control my anger and 0 1 2 3 4 frustration
at myself
5. I find it easy to forgive myself. 0 1 2 3 4 6. There is a
part of me that feels I am not 0 1 2 3 4 good enough.
7. I feel beaten down by my own self-critical 0 1 2 3 4 thoughts.
8. I still like being me. 0 1 2 3 4
9. I have become so angry with myself that 0 1 2 3 4 I want to
hurt or injure myself.
10. I have a sense of disgust with myself. 0 1 2 3 4
11. I can still feel lovable and acceptable. 0 1 2 3 4
12. I stop caring about myself. 0 1 2 3 4
13. I find it easy to like myself. 0 1 2 3 4
14. I remember and dwell on my failings. 0 1 2 3 4
15. I call myself names. 0 1 2 3 4
16. I am gentle and supportive with myself. 0 1 2 3 4
17. I can’t accept failures and setbacks 0 1 2 3 4 without
feeling inadequate.
18. I think I deserve my self-criticism. 0 1 2 3 4
19. I am able to care and look after myself. 0 1 2 3 4
20. There is a part of me that wants to get 0 1 2 3 4
rid of the bits I don’t like.
21. I encourage myself for the future. 0 1 2 3 4
22. I do not like being me. 0 1 2 3 4
Appendix XIV: Self Compassion Scale (SCS)
How I Typically Act Towards Myself in Difficult Times
(Neff, 2003b)
Please read each statement carefully before answering. To the left of each item, indicate how often you behave in the stated manner, using the following scale:
Almost Almost never always
1 2 3 4 5
_____ 1. I’m disapproving and judgmental about my own flaws and inadequacies.
_____ 2. When I’m feeling down I tend to obsess and fixate on everything that’s wrong.
_____ 3. When things are going badly for me, I see the difficulties as part of life that everyone goes through.
_____ 4. When I think about my inadequacies, it tends to make me feel more separate and cut off from the rest of the world.
_____ 5. I try to be loving towards myself when I’m feeling emotional pain.
_____ 6. When I fail at something important to me I become consumed by feelings of inadequacy.
_____ 7. When I’m down and out, I remind myself that there are lots of other people in the world feeling like I am.
_____ 8. When times are really difficult, I tend to be tough on myself.
_____ 9. When something upsets me, I try to keep my emotions in balance.
_____ 10. When I feel inadequate in some way, I try to remind myself that feelings of inadequacy are shared by most people.
_____ 11. I’m intolerant and impatient towards those aspects of my personality I don’t like.
_____ 12. When I’m going through a very hard time, I give myself the caring and tenderness I need.
_____ 13. When I’m feeling down, I tend to feel like most other people are probably happier than I am.
_____ 14. When something painful happens, I try to take a balanced view of the situation.
_____ 15. I try to see my failings as part of the human condition.
_____ 16. When I see aspects of myself that I don’t like, I get down on myself.
_____ 17. When I fail at something important to me I try to keep things in perspective.
_____ 18. When I’m really struggling, I tend to feel like other people must be having an easier time of it.
_____ 19. I’m kind to myself when I’m experiencing suffering.
_____ 20. When something upsets me, I get carried away with my feelings.
_____ 21. I can be a bit cold-hearted towards myself when I’m experiencing suffering.
_____ 22. When I’m feeling down I try to approach my feelings with curiosity and openness.
_____ 23. I’m tolerant of my own flaws and inadequacies.
_____ 24. When something painful happens, I tend to blow the incident out of proportion.
_____ 25. When I fail at something that’s important to me, I tend to feel alone in my failure. _____ 26. I try to be understanding and patient towards those aspects of my personality I don’t like.
Appendix XV: Hamilton Depression Rating Scale-17</strong> (Hamilton, 1960)
Please complete the scale based on a structured interview
Instructions: for each item select the one ‘cue’ which best characterises the patient. Be sure to record the answers in the appropriate spaces.
1. Depressed Mood 0 Absent.
1. These feeling states indicated only on questioning.
2. These feeling states spontaneously reported verbally.
3. Communicates feeling states non-verbally i.e. through facial expression, posture, voice and tendency to weep.
4. Patient reports virtually only these feeling states in his/her spontaneous verbal and non-verbal communication
2. Feelings of guilt 0. Absent.
1. Self-reproach, feels he/she has let people down.
2. Ideas of guilt or rumination over past errors or sinful deeds.
3. Present illness is punishment. Delusions of guilt.
4. Hears accusatory or denunciatory voices and/or experiences threatening visual hallucinations.
3. Feelings of guilt 0. Absent.
1. Feels like life is not worth living.
2. Wishes he/she were dead or any thoughts of possible death to self.
3. Ideas or gestures of suicide.
4. Attempts at suicide (any serious attempts 4).
4. Insomnia: early in the night 0. No difficulty falling asleep.
1. Complains of occasional difficulty falling asleep, I.e. more than half an hour 2. Complains of nightly difficulty falling asleep.
5. Insomnia: middle of the night 0. No difficulty.
1. Patient complains of being restless and disturbed during the night.
2. Waking during the night-any getting out of bed rates 2 (except for purposes of voiding).
6. Insomnia: early hours of the morning 0. No difficulty.
1. Waking in the early hours of the morning but goes back to sleep.
2. Unable to fall asleep again if he/she gets out of bed.
7. Work and activities 0. No difficulty.
1. Thoughts and feelings of incapacity, fatigue or weakness related to activities, work or hobbies.
2. Loss of interest in activity, hobbies or work-either directly reported by the patient or indirect in listlessness, indecision and vacillation (feels he or she has to push self to work or activities).
3. Decrease in actual time spent in activities or decrease in productivity. Rate 3 if the patient does not spend at least 3 hours a day in activities (job or hobbies).
4. Stopped working because of present illness. Rate 4 if patient engages in no activities except routine chores, or if patient fails to perform routine chores unassisted.
8. Retardation (slowness of thought and speech, impaired ability to concentrate, decreased motor activity)
0. Normal speech and thought.
1. Slight retardation during interview. 2 obvious retardation during interview 3. Interview difficult.
4. Complete stupor.
9. Agitation 0. None.
1. Fidgetiness.
2. Playing with hands, hair, etc.
3. Moving about can’t sit still.
4. Hand wringing, nail biting, hair pulling, biting of lips.
10. Anxiety psychic 0. No difficulty.
1. Subjective tension and irritability.
2. Worrying about minor matters.
3. Apprehensive attitude apparent in face or speech.
4. Fears expressed without questioning.
11. Anxiety somatic (physiological concomitants of anxiety) such as: Gastrointestinal: dry mouth, wind, indigestion, diarrhoea, cramps, belching
Cardio-vascular: palpitations, headaches
Respiratory: hyperventilation, sighing
Urinary Sweating
0. Absent.
1. Mild.
2. Moderate.
3. Severe.
4. Incapacitating.
12. Somatic symptoms gastrointestinal 0.
None.
1. Loss of appetite but eating without staff encouragement. Heavy feelings in abdomen.
2.Difficulty eating without staff urging. Requests or requires laxatives or medication for bowels or medication for gastrointestinal symptoms.
13. General somatic symptoms 0. None.
1. Heaviness in limbs, back or head. Backaches, headaches, muscle aches. Loss of energy and fatigability.
2.Any clear-cut symptoms rates 2.
14. Genital symptoms 0. Absent.
1. Mild.
2. Severe.
15. Hypochondriasis 0. Not present.
1. Self-absorption (bodily).
2. Preoccupation with health.
3. Frequent complaints, requests for help etc.
4. Hypochondriacal delusions.
16. Weight loss (rate either a or b)
a. According to the patient:
0. No weight loss.
1. Probably weight loss associated with present illness.
2. Definite (according to patient) weight loss.
3. Not assessed.
b. According to weekly measurements:
0. Less than 1 lb. in a week.
1. Greater than 1 lb. weight loss in a week.
2. Greater than 2lbs. weight loss in a week.
3. Not assessed.
17. Insight
0. Acknowledges being depressed and ill.
1. Acknowledges illness but attributes cause to bad food, climate, overwork, virus, need for rest etc.
2. Denies being ill at all.
Total score:
Appendix XVI: Beck Depression Inventory-I (BDI-I)
(Beck, Ward, Mendelson, Mock and Erbaugh (1961) Please
rate how you have been feeling in the last 2 weeks.
1. 0 I do not feel sad
1 I feel sad
2 I am sad all the time and I can’t snap out of it
3 I am so sad and unhappy that I can’t stand it
2. 0 I am not particularly discouraged about the future
1 I feel discouraged about the future
2 I feel I have nothing to look forward to
3 I feel the future is hopeless and that things cannot improve
3. 0 I do not feel like a failure
1 I feel I have failed more than the average person
2 As I look back on my life, all I can see is a lot of failures
3 I feel I am a complete failure as a person
4. 0 I get as much satisfaction out of things as I used to
1 I don’t enjoy things the way I used to
2 I don’t get real satisfaction out of anything anymore
3 I am dissatisfied or bored with everything
5. 0 I don’t feel particularly guilty
1 I feel guilty a good part of the time
2 I feel quite guilty most of the time
3 I feel guilty all of the time
6. 0 I don’t feel I am being punished
1 I feel I may be punished
2 I expect to be punished
3 I feel I am being punished
7. 0 I don’t feel disappointed in myself
1 I am disappointed in myself
2 I am disgusted with myself
3 I hate myself
8. 0 I don’t feel I am any worse than anybody else
1 I am critical of myself for my weaknesses or mistakes
2 I blame myself all the time for my faults
3 I blame myself for everything bad that happens
9. 0 I don’t have any thoughts of killing myself
1 I have thoughts of killing myself, but I would not carry them out
2 I would like to kill myself
3 I would kill myself if I had the chance
10. 0 I don’t cry any more than usual
1 I cry more now than I used to
2 I cry all the time now
3 I used to be able to cry, but now I can’t cry even though I want to
11. 0 I am no more irritated by things than I ever was
1 I am slightly more irritated now than usual
2 I am quite annoyed or irritated a good deal of the time
3 I feel irritated all the time
12. 0 I have not lost interest in other people
1 I am less interested in other people than I used to be
2 I have lost most of my interest in other people
3 I have lost all of my interest in other people
13. 0 I make decisions about as well as I ever could
1 I put off making decisions more than I used to
2 I have greater difficulty in making decisions more than I used to
3 I can’t make decisions at all anymore
14. 0 I don’t feel that I look any worse than I used to
1 I am worried that I am looking old or unattractive
2 I feel there are permanent changes in my appearance that make me look unattractive 3 I believe that I look ugly
15. 0 I can work about as well as before
1 It takes an extra effort to get started at doing something
2 I have to push myself very hard to do anything
3 I can’t do any work at all
16. 0 I can sleep as well as usual
1 I don’t sleep as well as I used to
2 I wake up 1–2 hours earlier than usual and find it hard to get back to sleep
3 I wake up several hours earlier than I used to and cannot get back to sleep.
17. 0 I don’t get more tired than usual
1 I get tired more easily than I used to
2 I get tired from doing almost anything
3 I am too tired to do anything
18. 0 My appetite is no worse than usual
1 My appetite is not as good as it used to be
2 My appetite is much worse now
3 I have no appetite at all anymore
19. 0 I haven’t lost much weight, if any, lately
1 I have lost more than five pounds
2 I have lost more than ten pounds
3 I have lost more than fifteen pounds
20. 0 I am no more worried about my health than usual
1 I am worried about physical problems like aches, pains, upset stomach, or constipation
2 I am very worried about physical problems and it’s hard to think of much else
3 I am so worried about my physical problems that I cannot think of anything else
21. 0 I have not noticed any recent change in my interest in sex
1 I am less interested in sex than I used to be
2 I have almost no interest in sex
3 I have lost interest in sex completely
Appendix XVII: The Patient Health Questionaire-9 (PHQ-9)
(Kroenke, Spitzer and Williams, 2012)
| PATIENT HEALTH QUESTIONNAIRE-9 |
(PHQ-9) | |
| Over the last 2 weeks, how often have you been bothered by any of the following problems? (Use “✔” to indicate your answer) | Not at all | Several days | More than half the days | Nearly |
every day |
| 1. Little interest or pleasure in doing things | 0 | 1 | 2 | 3 |
| 2. Feeling down, depressed, or hopeless | 0 | 1 | 2 | 3 |
| 3. Trouble falling or staying asleep, or sleeping too much | 0 | 1 | 2 | 3 |
| 4. Feeling tired or having little energy | 0 | 1 | 2 | 3 |
| 5. Poor appetite or overeating | 0 | 1 | 2 | 3 |
| 6. Feeling bad about yourself — or that you are a failure or have let yourself or your family down | 0 | 1 | 2 | 3 |
| 7. Trouble concentrating on things, such as reading the newspaper or watching television | 0 | 1 | 2 | 3 |
| 8. Moving or speaking so slowly that other people could have noticed? Or the opposite — being so fidgety or |
restless that you have been moving around a lot more than usual | 0 | 1 | 2 | 3 |
| 9. Thoughts that you would be better off dead or of hurting yourself in some way | 0 | 1 | 2 | 3 |
Appendix XVIII: Qualitative Interview Topic Guide
Study title: Mood Disorder RCT – An investigation into the role of Shame, self-criticism and self-compassion in persistent, treatment resistant depression
Aim: The interview will investigate how participants experience depression, shame, selfcriticism and self-compassion
Introduction
Good afternoon. My name is _______ Thank you for meeting with me today….
Present the purpose
We are meeting today to explore in some detail your experience of depression and more specifically shame, self-criticism and self-compassion. The purpose is to understand how you experience depression and whether or not shame, self-criticism and self-compassion are aspects of your experience of depression, its impact on your life and how you deal with it on a day to day basis. I am particularly interested in hearing about this in your own words. Your experiences and perceptions are what matter. There are no right or wrong, desirable or undesirable answers. I would like you to feel comfortable saying what you really think and how you really feel.
Discuss procedure
I will be taking notes and recording the discussion so that I do not miss anything you have to say. I explained these procedures to you when we set up this meeting. As you know everything is confidential. No one will know who said what as any information you provide will be anonymous – nothing you say will be linked to your name.
The discussion will last approximately 90 minutes. As you know we will be talking about your experience of depression and this may at times be distressing. If at any point, you would like to take a break or need any support with this, just let me know.
Any questions about this?
Interview
Background information and rapport building
Tell me a little about yourself……
-
Name, age
-
Home life o Who do you live with/family? o Employment o Activities during a typical week
Research topic
(Aim: to explore participant’s experience of depression, shame, self-criticism and selfcompassion
This section includes questions of participants experience in the following areas:
Key questions
-
Can you tell me how depression affects you on a day to day basis?
(possible prompts: What activities does it interfere with? How do you feel? How does it impact on how you think about yourself?
-
What do you spend more time doing and thinking about when your mood is depressed?
-
What do you spend less time doing and thinking about when your mood is depressed?
-
Does depression affect the way you react to things? In what way?
-
Can you tell me about a recent time when X (depending on reply above) was particularly noticeable?
(possible prompts: What happened? How did you feel? What went through your mind? What did you do?)
-
How do you see yourself as a person when your mood is depressed/less depressed?
-
Can you give me an example of how you talk to yourself when your mood is depressed/less depressed?
(possible prompts: for example, if you made a mistake? If you were at a social gathering? When you are at work?)
-
Can you recall when thinking about yourself in this way first began?
(possible prompts: for partner, family, friends, work colleagues, strangers) • How do you think those experiences you are describing have affected you?
-
How do you think other people see you?
(possible prompts: for example, partner, family, friends, work colleagues, strangers)
-
What do you find most helpful in dealing with your depression?
-
What do you find most unhelpful in dealing with your depression?
-
What would it be like to try and be kind to yourself when your mood is depressed?
Summary
(Aim: to round up the interview and close)
Researcher summarise conversation and what has been discussed throughout the interview
Any questions about the interview? Anything else that we haven’t discussed today that you feel is important?
I appreciate that talking through these experiences can be upsetting.
Is there anything you would like to discuss in relation to this?
Thanks, and close
Appendix XIX: Histogram and box plot for the OAS sub- inferior at baseline
Appendix XX: Histogram and box plot for the OAS sub-scale emptiness at baseline
Appendix XXI: Histogram and box plot for the OAS sub- mistakes at baseline
Appendix XXII: Histogram and box plot for the FSCSR sub-scale inadequate self at baseline
Appendix XXIII: Histogram and box plot for the FSCSR sub- hated self at baseline
Appendix XXIV: Histogram and box plot for the FSCSR sub-scale reassured self at baseline
Appendix XXV: Histogram and box plot for the SCS sub-scale self-kindness at baseline
Appendix XXVI: Histogram and box plot for the SCS sub-scale self-judgement at baseline
Appendix XXVII: Histogram and box plot for the SCS sub-scale common humanity at baseline
Appendix XXVIII: Histogram and box plot for the SCS sub-scale isolation at baseline
Appendix XXIX: Histogram and box plot for the SCS sub-scale mindfulness at baseline
Appendix XXX: Histogram and box plot for the SCS sub-scale overidentification at baseline
Appendix XXXI: Example of steps of qualitative data analysis (participant 12)
| Transcript | Round 1 analysis | Round 2 analysis | Emergent themes | Round 4 analysis |
| Participant 12 | Descriptive/conceptual/linguistic comments: How the participant describes depression; shame; self-criticism and selfcompassion | Individual Mind Map | Emergent themes convergent/divergent with Gilbert’s model | |
| Page 1 lines 1–8 |
In response to question:
‘So perhaps if you could just start just telling me in your own words how your depression affects you on a day to day basis?
‘You don’t feel good enough for anything there is no point in anything you do criticise yourself all the while you feel other people are fed up with you and don’t want to listen and you feel isolated (and would you say that is pretty consistent does it vary at all?)It used to be consistent but I am fighting with myself and I think at the moment doing quite well’
Page 1 lines 9–10
In response to question: | Tendency towards self-criticism is articulated without promoting-she recognises it as part of the depression. She also recognises a perception ‘you feel others are fed up with you and don’t want to listen’.
Concept of doing battle ‘with self’ rather than illness? | See appendix XXXII | Self-criticism | Convergent: sense of self in the mind of the other –‘others fed up with you’ |
Right ok tell me a little bit about that idea of fighting with yourself
‘You just need the strength that it is worth the fight’
P1 lines 11–19
Can you say a little bit about the strength where that might come from?
‘My eldest daughter and my sister my husband to an extent. Erm I have been very low since the depression, with cancer. And I think none of this is going to beat me anymore life is worth living so it is just such an awful place to be’
P1-2 lines 20–36 In response to question:
‘What sort of things have you tried to do in order to fight it?’ | Constructs of strength (vs. weakness) and a sense there is something worth fighting for
What does fighting with yourself mean?
Inner sense of self?
No recognition or articulation of any of her own internal strength or mettle
Makes a connection between treatment for cancer and depression sense ‘none of this is | | | |
‘I used to have a CPN and he used to tell me go outside smell things, walk, I walked miles. (Do | going to beat me anymore’ a sense of purpose and possibly strength drawn from treatment for cancer to tackle depression | | Strength comes from others | Convergent: we are inherently social creatures -we survive in groups and need each other to develop and thrive -attachment |
| you?) Yeah thinking what you have got to realise that life is still going on around you and others think life is wonderful so it has got to be you but you are back to self-criticism and other people have to build and rebuild my self-confidence (And how do they do that?)They take me out, because I got I couldn’t go out and leave the house at all and I would wander off with the least provocation just to get away from anybody. It got they couldn’t take me out as I want to throw myself under passing trains, cars but somehow they have just made me see life is worth living again’. …… |
P14 lines 349–364
In response to question:
Do you have a sense of what you might say to yourself if you were trying to be kinder to yourself in relation to finding it difficult to cope?
‘To be kinder to myself? (What about the compassionate
stance towards your struggle?)
Not something I think about. (again, if you were well and it was your sister who was saying I am selfish what would you say | Acknowledgment ?depression ?cancer both are an awful placeempathy for self and own suffering?
Again, recognition of
selfcriticism and its effects and also a need for help from others in order to deal with depression and see life as worth living. Possibly an acceptance of needing to do this repeatedly, again and again and an acceptance it cannot be done without help and support. | | Negative view of self -no recognition/acknowledgment of her own mettle -Attribution in depression
Self-criticism | Divergent: attribution |
to her? Yeah she has told me off I am still trying to do too much | | | | |
| for others (would be kind to your sister what would you say to her?) You have got your own health and future to think of |
Jackie be kinder to yourself silly isn’t it?
P14 lines 365–291
In response to question:
And how would it feel to try and say that to yourself about the same thing?
‘That you are blowing your own trumpet you know if you told yourself you were good. Well that is all fairly recent you see. So, I did not think of that before. That is since the cancer that is very levelling cancer. And I am still under them they have not given me the all clear and I fought so hard with that, mother was shouting. Oh yes. (What was she saying? Well she would hide the cancer. Come on you can do it pull yourself together oh she still shouts at me (Does she?) Yeah not nastily. She is trying to encourage me.
(And does it help?). Oh yeah
(and so what sort of shouting is it is it sort of a? Firm but a kind. | Also, if we are not used to kindness in voice or manner does this activate feelings of worthlessness? Compassion in voice tone and action may be alien but it may also be aversiveactivating feelings of worthlessness, anxiety, shame
(if it is perceived as not deserved)?
Kindness is associated with being boastful-‘blowing your own trumpet’- ‘speak openly and boastfully about your own achievements’-marker for deference? Subjugation | | Absence of kindness to self never thought about it | Convergent: lack of selfcompassion | | An observation: participant fought hard against the cancer, encouraged by an internalised version of her mother ‘shouting’ | | | |
| at her. This shouting is not described as ‘nasty’ or ‘harsh’ but as encouraging ‘firm (voice tone) but kind’. Implicit in this description is the idea that to speak to yourself with kindness (gentle voice tone) somehow means it will not be so effective? Firmness is required to spur you on? In some situations, this may well be trueis speaking to yourself in a firm but encouraging tone-is this compassionate if you are trying to engage with something that is hard? | Deference/subjugation | Convergent: social rank | ||||||
| Voice tone | Convergent and divergent: |
Gilbert only speaks of warm, gentle, kind voice tone-firm but fair may also be compassionate?
Do we as therapists have an idealised stereotypical view of what a compassionate voice tone means. |
Appendix XXXII: Photographs of an example of a mind map (participant 12)
Appendix XXXIII: Biographies of participants in qualitative arm of this PhD study
Participant 8 (interview 61 minutes duration): A 48-year-old white British man, single with no children who worked as a taxi driver. He described his depression as ‘lifelong’ and had been in contact with mental health services intermittently for the last fifteen years. His conversational style was garrulous, frequently tangential and the content at times contradictory. During the interview his voice tone was often sad and at two points he became tearful. At other points in the interview his tone was angry and resentful with a dismissive and denigratory tone towards others. He was keen to participate in the interview process but at times sought reassurance from the interviewer that he was answering the questions correctly, often denigrating his responses. The interview took place in the office of the interviewer.
Participant 9 (interview 55 minutes duration): A 25-year-old white British woman, single working as a dietician. She described a 6-year history of depression and at the time of the interview she described residual depressive symptoms and anxiety. She had completed a course of cognitive behaviour therapy (CBT) in the last 12 months. During the interview her voice tone conveyed a constant sense of irritation at herself for her perceived short comings and she frequently criticised herself during the interview. Her voice tone was anxious and earnest throughout, as if her striving to be perfect (which was a core feature of her conversation) was active in the moment e.g. answer the interview questions correctly. As a result, at times it was difficult to follow the thread of her conversation as she hesitated and often changed tack mid-sentence. She was a practising Christian and her relationship with God was a central part of our conversation. The interview took place in her own home.
Participant 11 (interview 33 minutes duration): A 58-year-old British born Afro-Caribbean woman married with three adult children who was retired from her profession (general nurse) on the grounds of ill health (rheumatoid arthritis and depression). She described a ten-year history of depression. In addition, this participant was diagnosed with three physical health conditions, rheumatoid arthritis, lupus and fibromyalgia and consequently experienced a continuous level of pain. She spoke quietly throughout the interview and with great reserve. The interview was the shortest conducted. In the transcription, there are very few statements that are longer than one line. There was warmth and gentleness in her voice tone mixed with sadness and resignation at the restrictions her ill health imposes on her day to day functioning. There was a sense she was complying with the interview process rather than participating in it. It felt as if she needed to keep the interviewer at arm’s length. The interview took place in the participants own home.
Participant 12 (interview 85 minutes duration): A 64-year-old, white British woman, married with two adult children who has been a carer all her life for various family members. She described a seven-year history of depression. In addition, she had in the last three months completed three years of treatment for bowel cancer and was making a good recovery. Her experience of having cancer had led her to conclude ‘life was worth fighting for’ and as result had made some significant changes in her life, particularly in terms of standing up for herself, which had exerted a beneficial impact on her depression. Her mood was euthymic at interview and throughout, when she shared examples of her thoughts and feelings and behaviour, she contrasted how she would have been in the past to how she was currently. She was open and honest in her sharing of information. Her voice tone conveyed mettle and determination to move forward from her previous view of herself towards a new way of being in the world. The interview took place in the participants own home.
Participant 15 (interview 90 minutes duration): A 59-year-old white man, married with two adult children and three grandchildren. He reported a 35-year history of depression. He was raised in the North East of England and joined the army at age 18. In his 20’s he was diagnosed with stomach ulcers. He had always smoked cigarettes and drank heavily since his teenage years. He had two cardiac arrests at age 35 years and was subsequently retired from work on the grounds of ill health. Throughout the interview, which took place in his own home, he dominated the room and took charge in the interaction. Throughout his voice tone was measured and controlled but with a sense that anger and shame simmered beneath. His speech was often hesitant. He was over inclusive in his self-report and he frequently made contradictory statements, moving the focus of the conversation away from the question posed. These behaviours can be markers of avoidant coping, which in turn may have been a marker for shame being present in an interaction. His voice tone was strident, irritable and despairing of his current perceived predicament regarding the constraints his medical problems placed on his day to day activities.
Participant 16 (interview 70 minutes duration): A 56-year-old, white British man. Divorced with two adult children. He reported a nineteen-year history of depression. He qualified and worked as a Civil Engineer for 25 years and five years previously had retired from his profession on the grounds of ill health due to depression. He worked full time in an administrative role. At the time of the interview his mood was euthymic and throughout the conversation he drew contrasts between how his thoughts, feelings and behaviours were when his mood was depressed versus not depressed. He was articulate throughout the interview. His voice tone was upbeat and inquisitive and he engaged in the discussion with enthusiasm. He was slightly preoccupied whilst speaking due to the fact he was in the process of making a fresh start in life. He was moving home to a different part of the country to live with his new partner and his telephone rang twice during the interview.
Participant 20 (interview 67 minutes duration): A 52-year-old, unemployed, white British man, divorced with two adult children. He described a 25-year history of depression. He was anxious during the session and self-conscious in relation to his lifelong stammer, which emerged in stressful situations, of which the interview was a possible trigger which he stated at the outset of the interview. However, he did not stammer at any point in the interview. His voice tone was cautious, with undertones of anxiety, sadness and shame. He conveyed a fear of being judged by the interviewer. He engaged in the interview with both honesty and integrity and spoke eloquently about his life and events which he felt contributed to his experience of depression. The interview took place in the office of the interviewer.
Participant 28 (interview 65 minutes duration): A 51-year-old white British woman, married with no children, who was retired from her profession (mental health nurse) on the grounds of ill health (depression) two years prior to the interview. She described a 20-year history of depression. She spoke quickly in the interview, with a voice tone that was matter of fact, even when the vocabulary used pointed towards feelings of anxiety, sadness and shame. She was articulate and considered throughout the interview and candid in her responses to questions, participating actively in the conversation. The interview took place in the office of the interviewer.
Participant 88 (interview 94 minutes duration): A 43-year-old single white British woman, living alone but with a partner. She had no children. She engaged in voluntary work with a mental health charity 2 days a week. She described a lifelong history of depression and had first sought help in her early twenties. She was very candid in the interview, not only disclosing childhood sexual abuse but speaking with frankness and eloquence about the impact of this on her internal world and her struggles to function in everyday life. At times in conversation with her it felt as if she had no means of drawing a boundary around disclosing intimate information to the interviewer. Her voice tone was both warm and solicitous unless she was disclosing details of childhood trauma and then her tone became matter of fact. The interview took place at the house of a friend.
Participant 136 (interview 47 minutes duration): A 54-year-old white British man living alone with no partner or children. He had been employed as a storeman in a local company for the last thirty years. He described having two friends whom he saw every 2–3 weeks. He described a twenty-year history of depression. He was softly spoken. His voice tone conveyed warmth and gentleness but with an anxious and embarrassed air. He was reserved and nervous throughout the interview and his answers to questions were short and to the point. There was a sense in which he held back certain information for fear of negative judgement. He described a life of isolation and aloneness which for him seemed a retreat from a world experienced as harsh and judgemental. The interview took place in his own home.
Appendix XXXIV: The subscales and items of the OAS
Inferior:
Item 1: I feel other people see me as not good enough
Item 2: I think that other people look down on me
Item 4: I feel insecure about others opinion of me
Item 5: Other people see me as not measuring up to them
Item 6: Other people see me as small and insignificant
Item 7: Other people see me as somehow defective as a person
Item 8: people see me as unimportant compared to others
Emptiness:
Item 15: Others see me as fragile
Item 16: Others see me as empty and unfulfilled
Item 17: Others think there is something missing in me
Item 18: Other people think I have lost control over my body and feelings
Mistakes:
Item 3: Other people put me down a lot
Item 9: Other people look for my faults
Item 10: People see me as striving for perfection but being unable to reach my own standards
Item 11: I think others are able to see my defects
Item 12: Others are critical and punishing when I make a mistake
Item 13: People distance themselves from me when I make mistakes
Item 14: Other people always remember my mistakes
Appendix XXXV: The sub-scales and items of the FSCSR
Inadequate Self
Item 1: I am easily disappointed in my self
Item 2: There is part of me that puts me down
Item 4: I find it difficult to control my anger and frustration at myself
Item 6: There is part of me that feels I am not good enough
Item 7: I feel beaten down by my own self-critical thoughts
Item 14: I remember and dwell on my failings
Item 17: I can’t accept failures and setbacks without feeling inadequate
Item 18: I think I deserve my self-criticism
Item 20: There is part of me that wants to get rid of the bits I don’t like
Hated Self
Item 9: I have become so angry with myself that I have wanted to hurt or injure myself
Item 10: I have a sense of disgust with myself
Item 12: I stop caring about myself
Item15: I call myself names
Item 22: I do not like being me
Reassured Self
Item 3: I am able to remind myself of positive things about myself
Item 5: I find it easy to forgive myself
Item 8: I still like being me
Item 11: I can still feel loveable and acceptable
Item 13: I find it easy to like myself
Item 16: I am gentle and supportive with myself
Item 19: I am able to care and look after myself
Item 21: I encourage myself for the future
Appendix XXXVI: The items and sub-scales of the SCS
Self-Kindness
Item 5: I try to be loving towards myself when I’m feeling emotional
Item 12: When I’m going through a very hard time, I give myself the caring and tenderness I need
Item 23: I am tolerant of m own flaws and inadequacies
Item 26: I try to be understanding and patient towards those aspects of my personality I don’t like
Item 19: I’m kind to myself when I’m experiencing suffering
Self-judgement
Item 1: I’m disapproving and judgemental about my own flaws and inadequacies
Item 8: When times are really difficult, I tend to be tough on myself
Item 11: I’m tolerant and impatient towards those aspects of my personality I don’t like
Item 16: When I see aspects of myself I don’t like, I get down on myself
Item 21: I can be a bit cold-hearted towards myself when I’m feeling emotional pain
Common Humanity
Item 3: When things are going badly for me, I see the difficulties as part of life that everyone goes through
Item 7: When I’m down and out, I remind myself that there are lots of other people in the world feeling like me
Item 10: When I feel inadequate in some way, I try to remind myself that feelings of inadequacy are shared by most people
Isolation
Item 4: When I think about my inadequacies, it tends to make me feel more separate and cut off from the rest of the world
Item 13: When I’m feeling down, I tend to feel like most other people are probably happier than I am
Item 18: When I’m really struggling, I tend to feel like most other people must be having an easier time of it
Item 25: When I fail at something that is important to me, I tend to feel alone in my failure
Mindfulness
Item 9: When something upsets me, I try to keep my emotions in balance
Item 14: When something painful happens, I try to take a balanced view of the situation
Item 17: When I fail at something important to me, I try and keep things in perspective
Item 22: When I’m feeling down, I try to approach my feelings with curiosity and openness
Overidentification
Item 2: When I’m feeling down, I tend to obsess and fixate on everything
Item 6: When I fail at something important to me, I become consumed by feelings of inadequacy
Item 20: When something upsets me, I get carried away with my feelings
Item 24: When something painful happens, I tend to blow the situation out of proportion
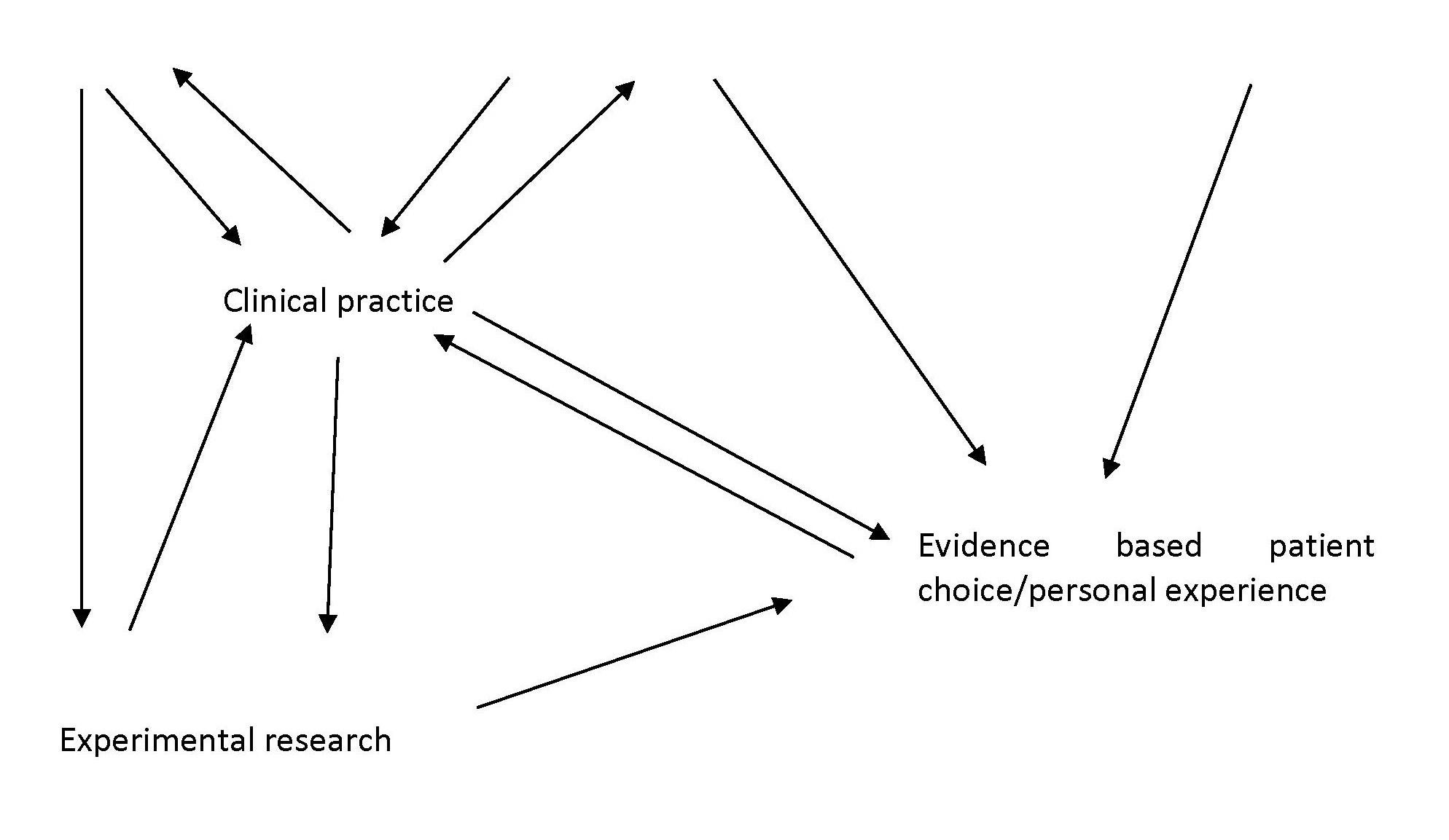
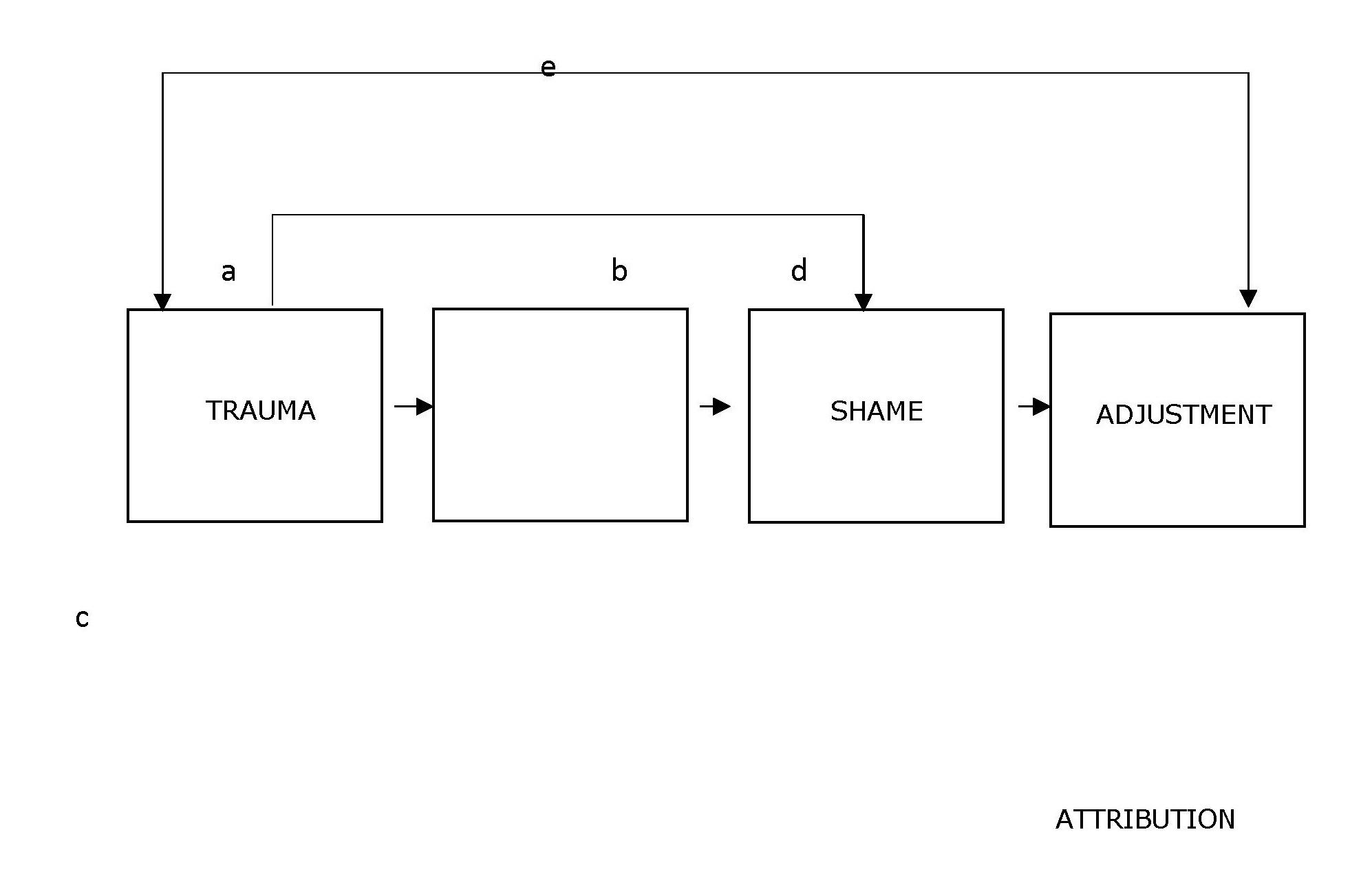
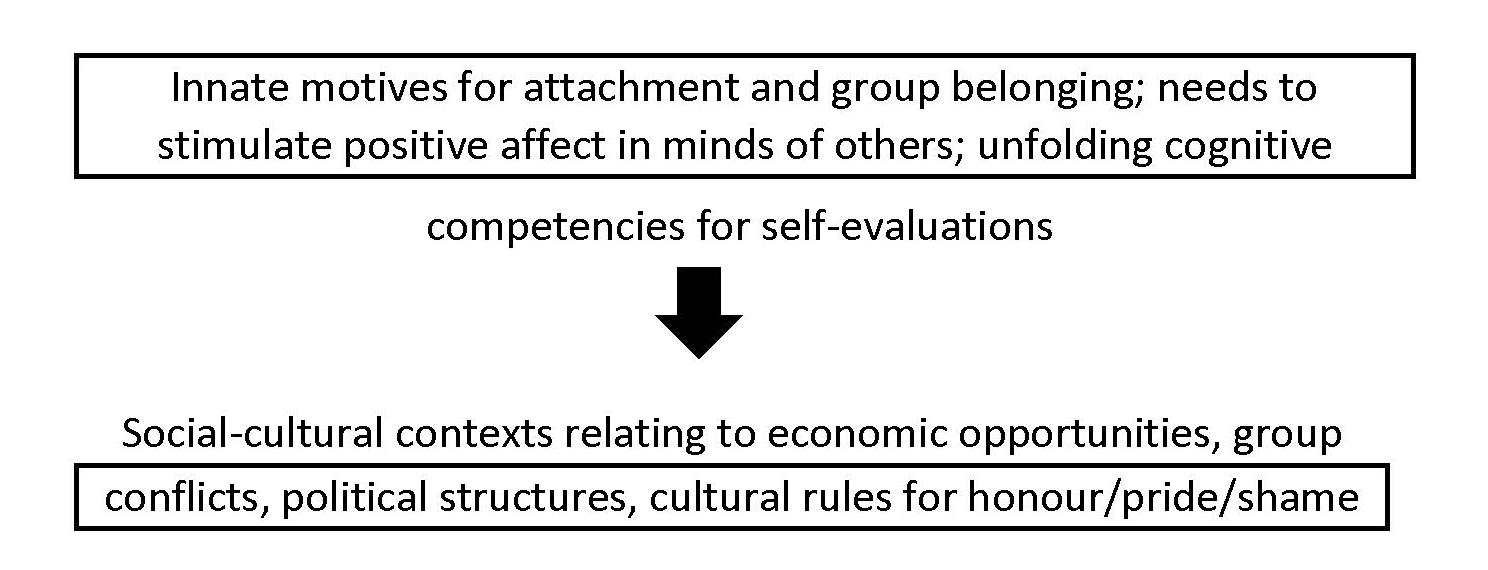
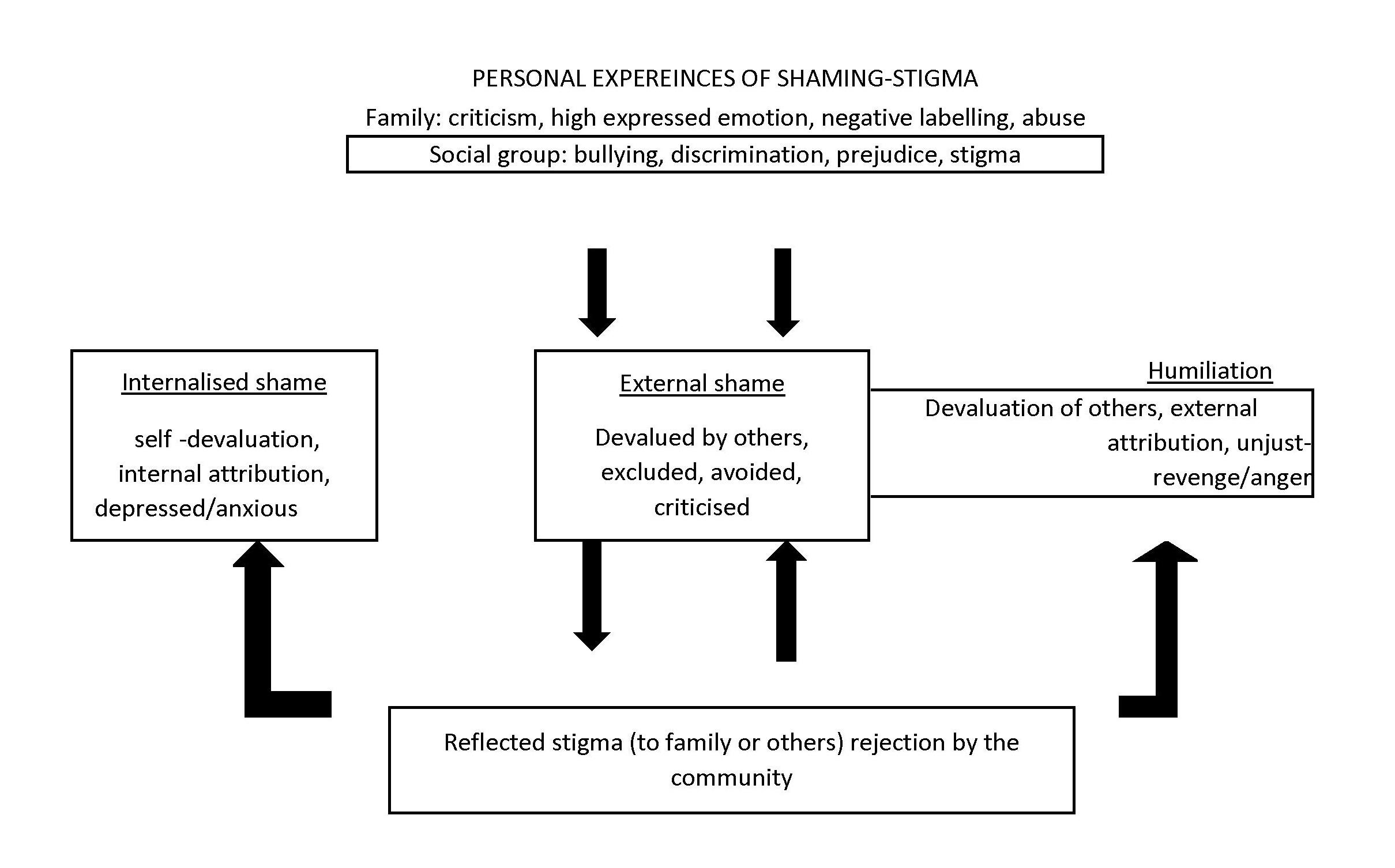
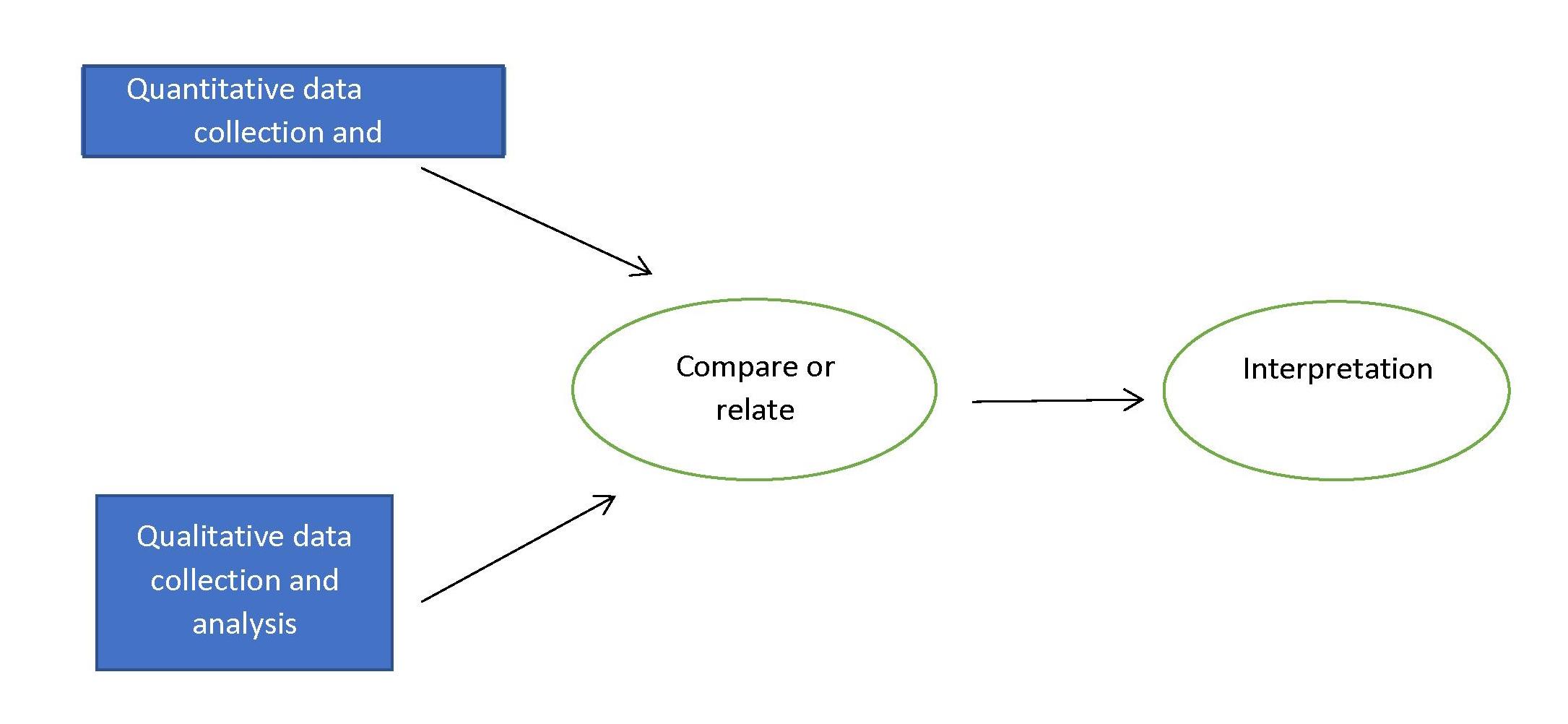
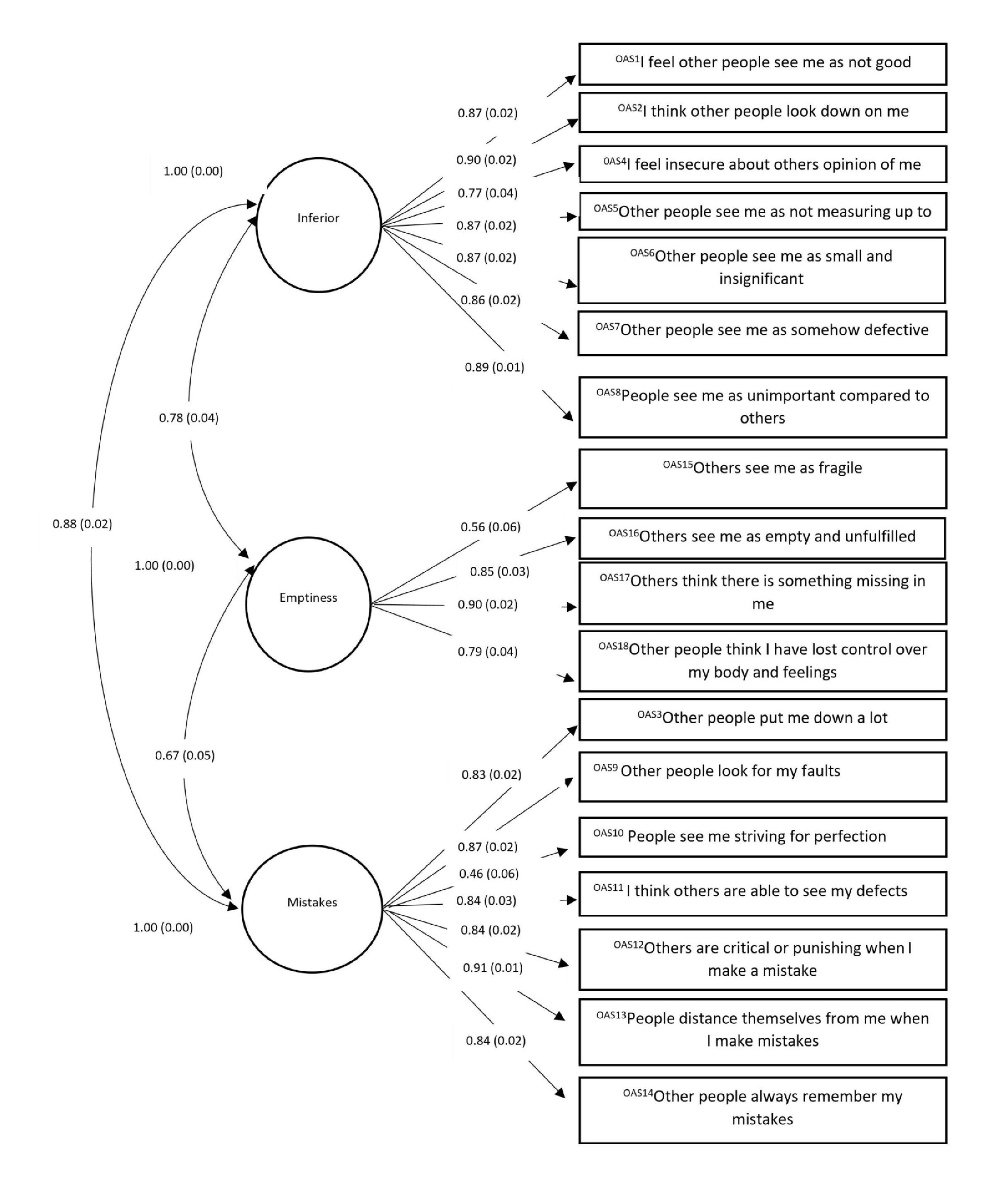
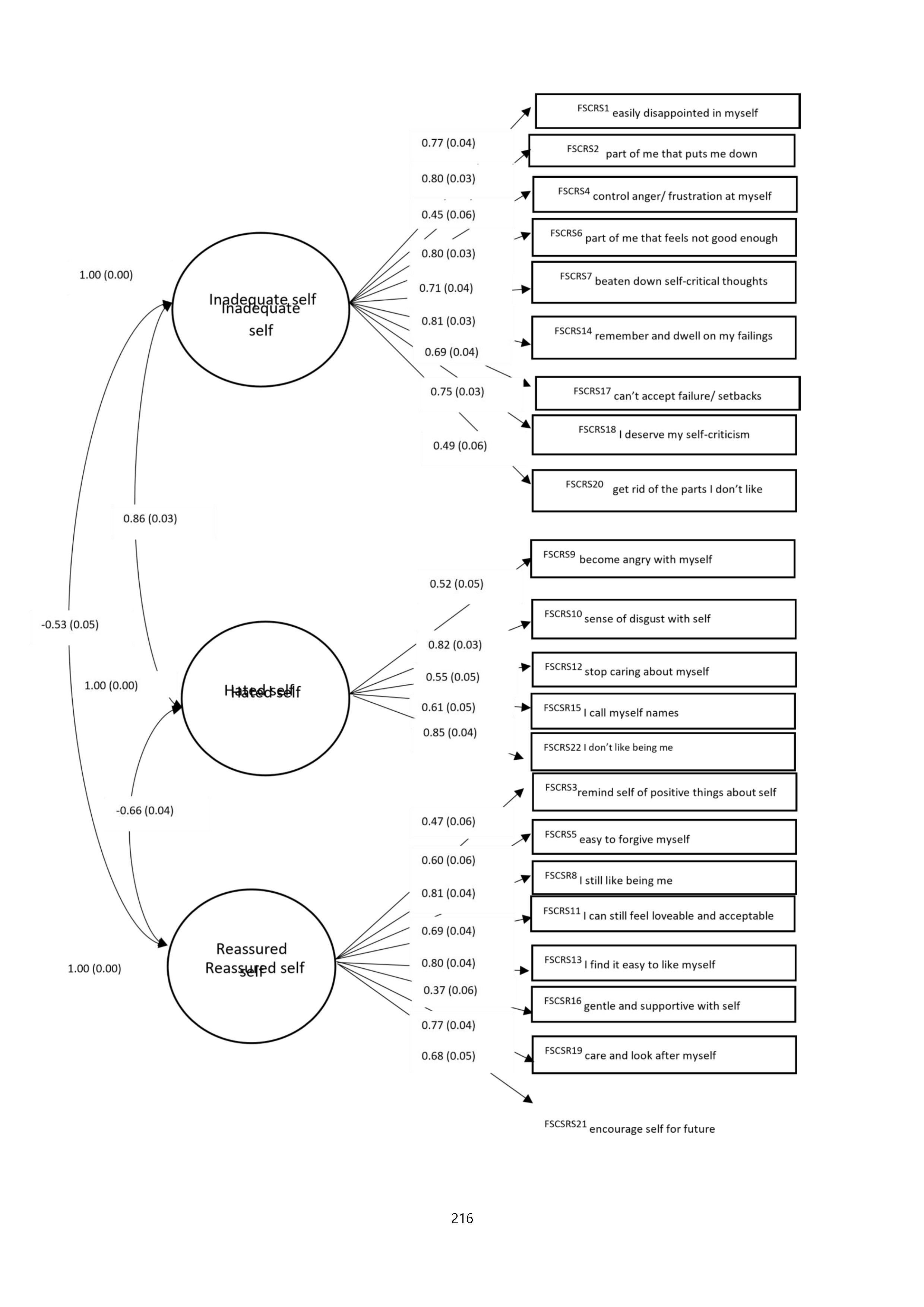
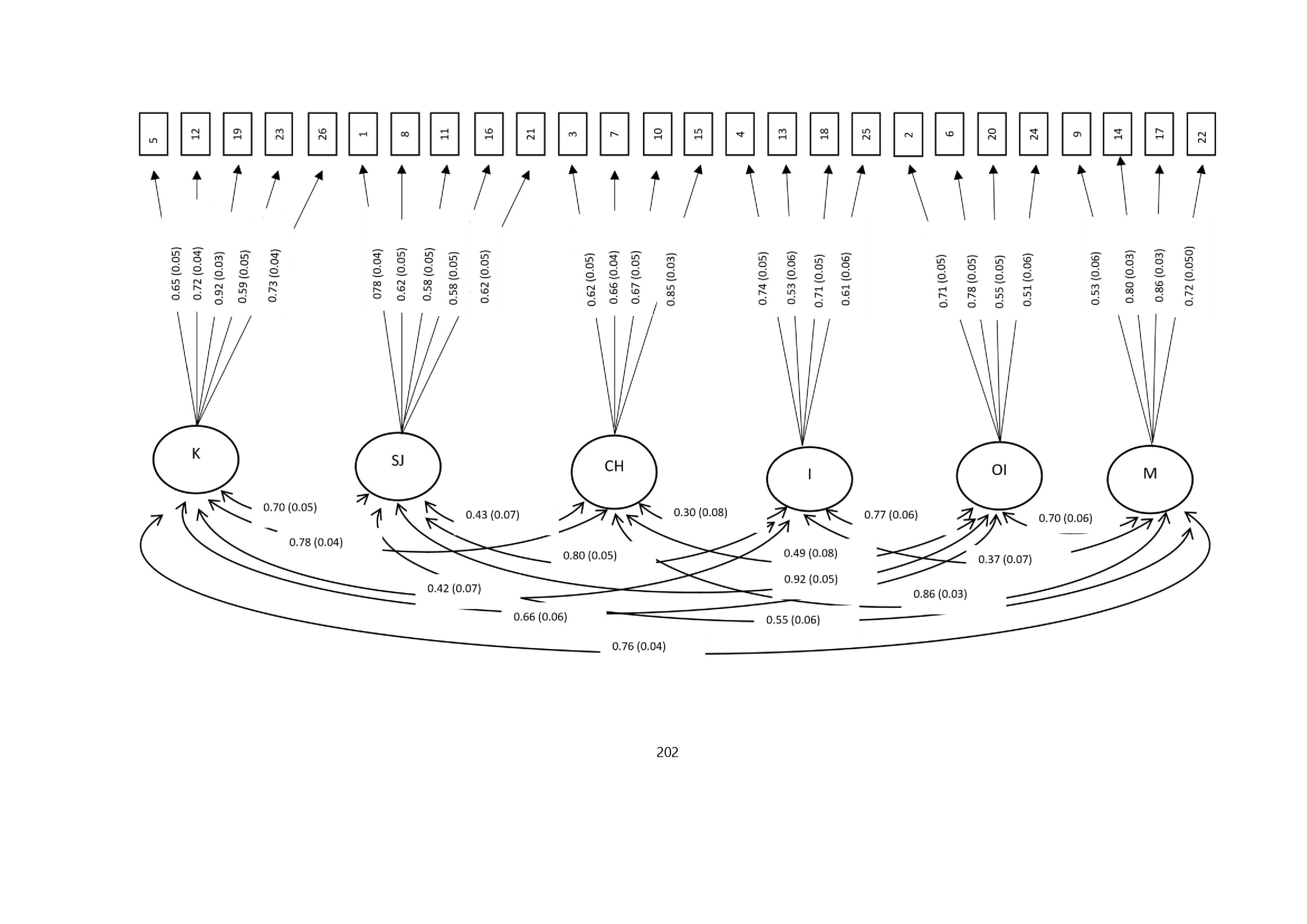
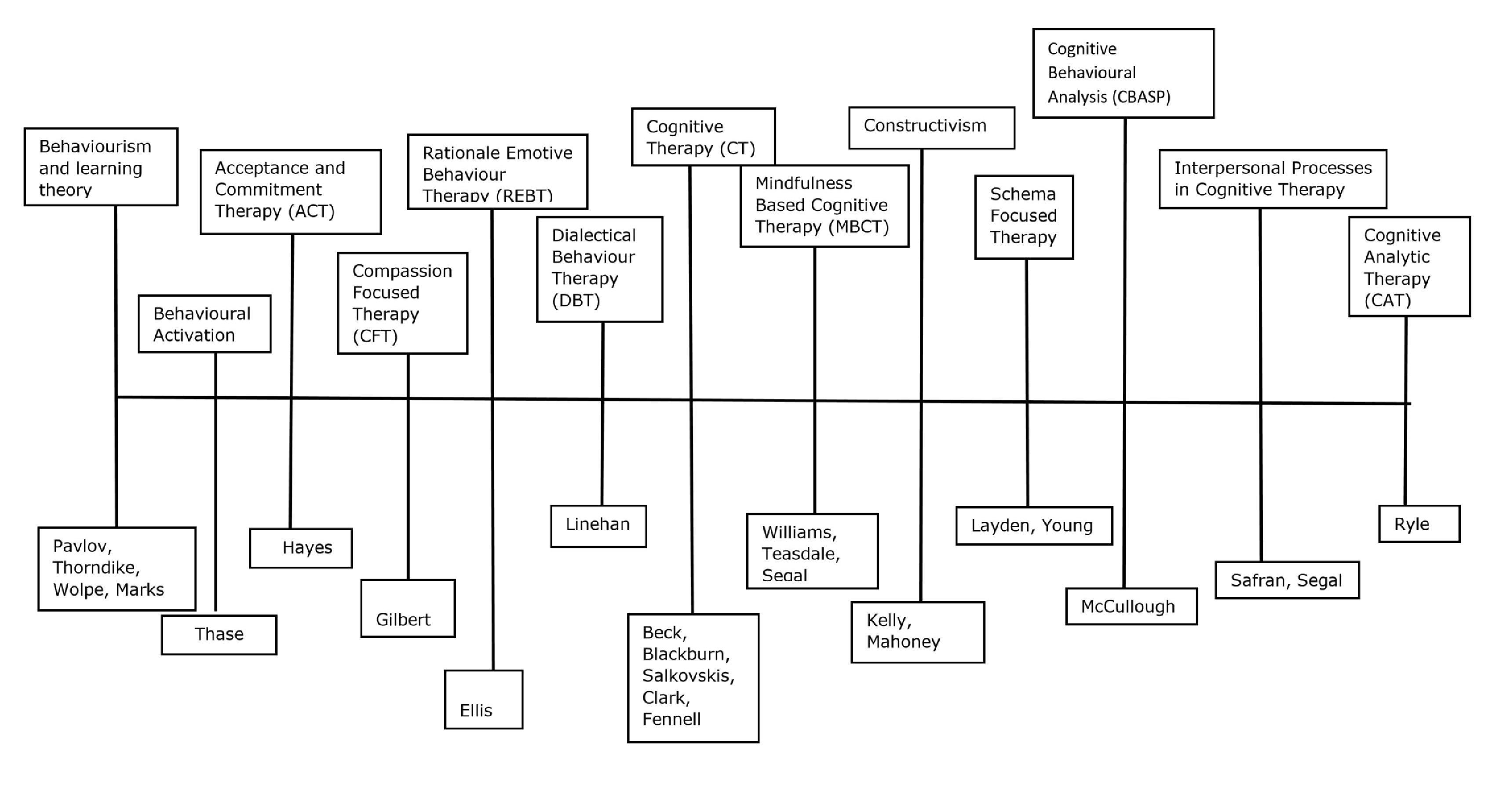
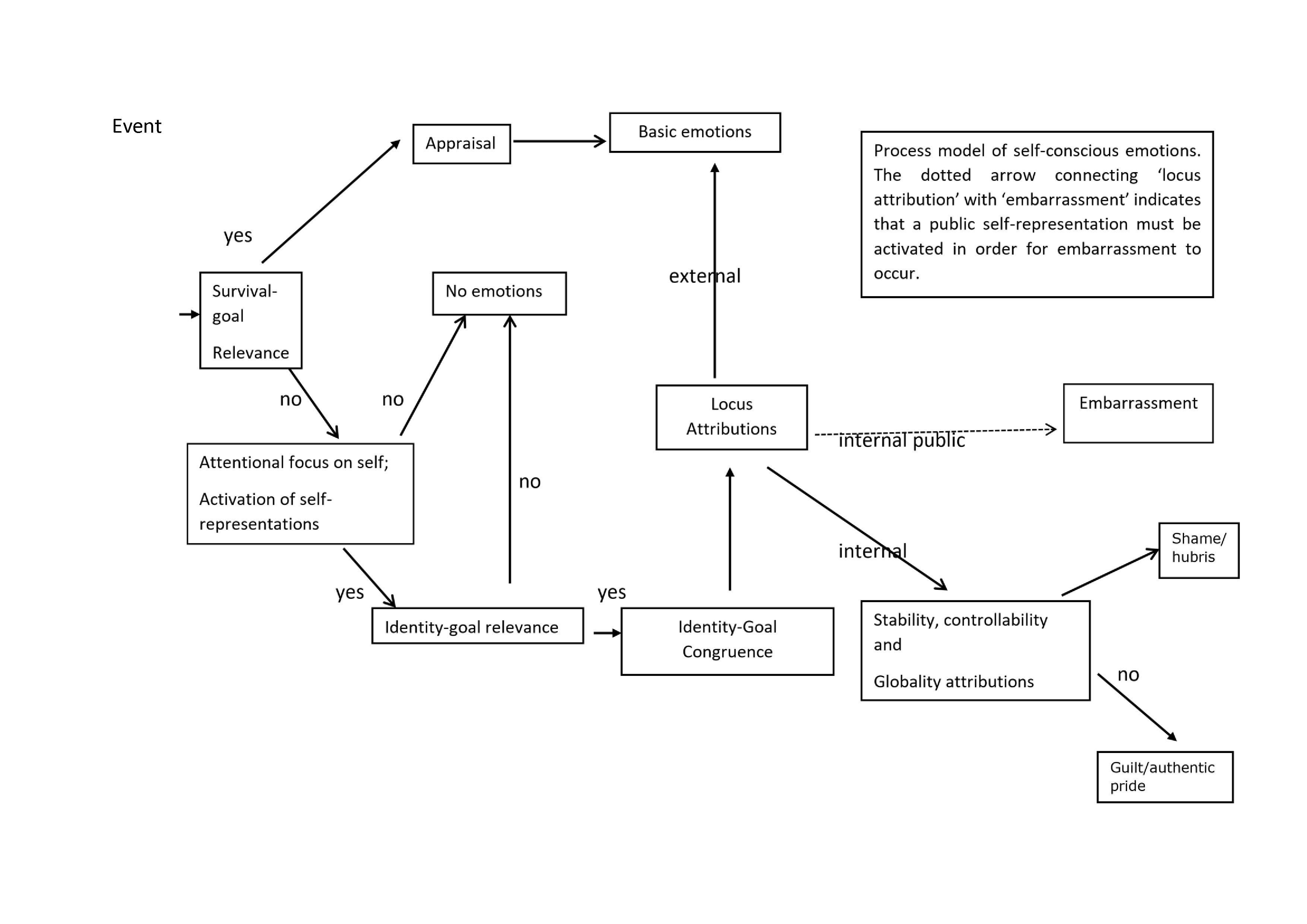
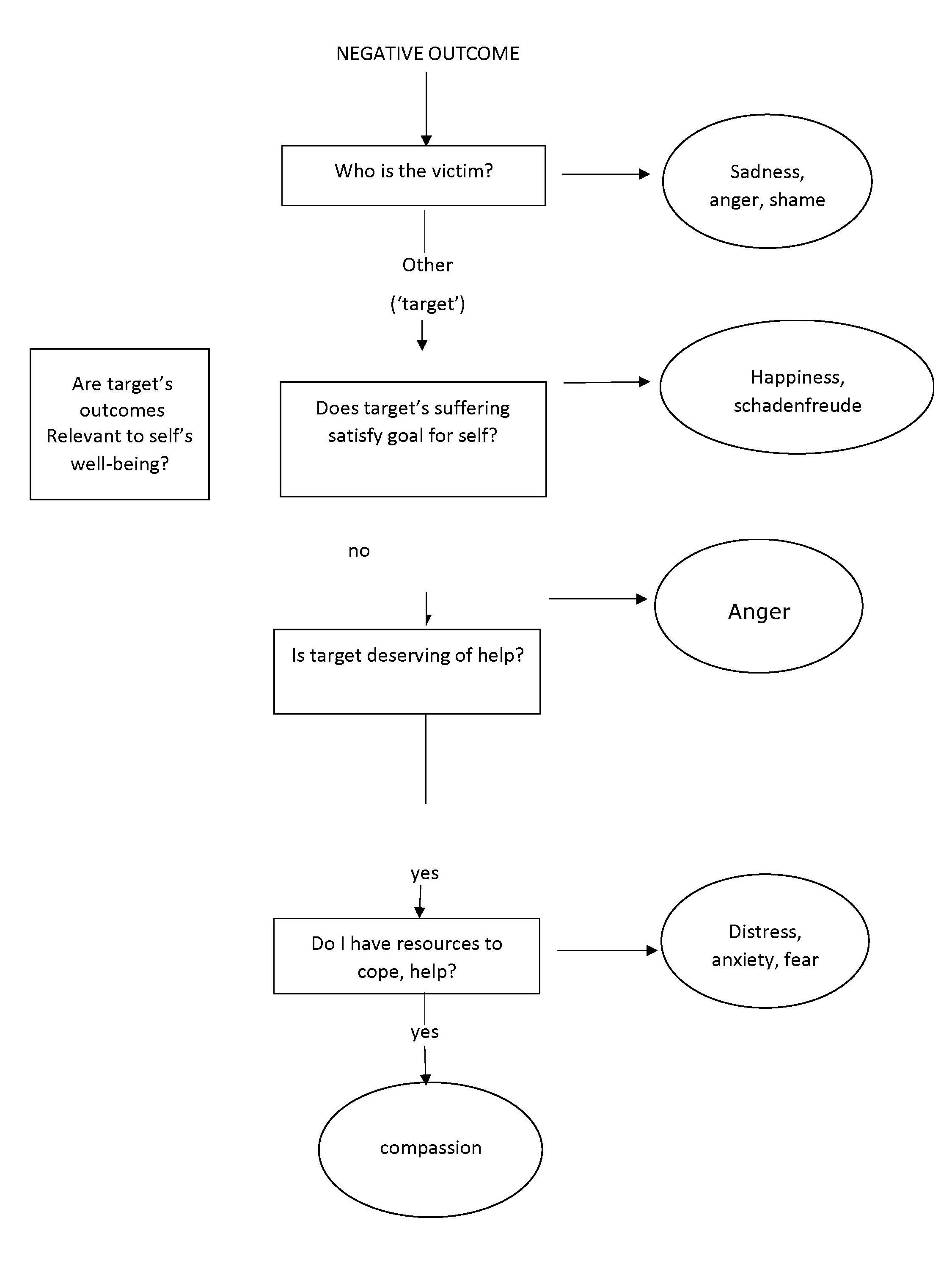
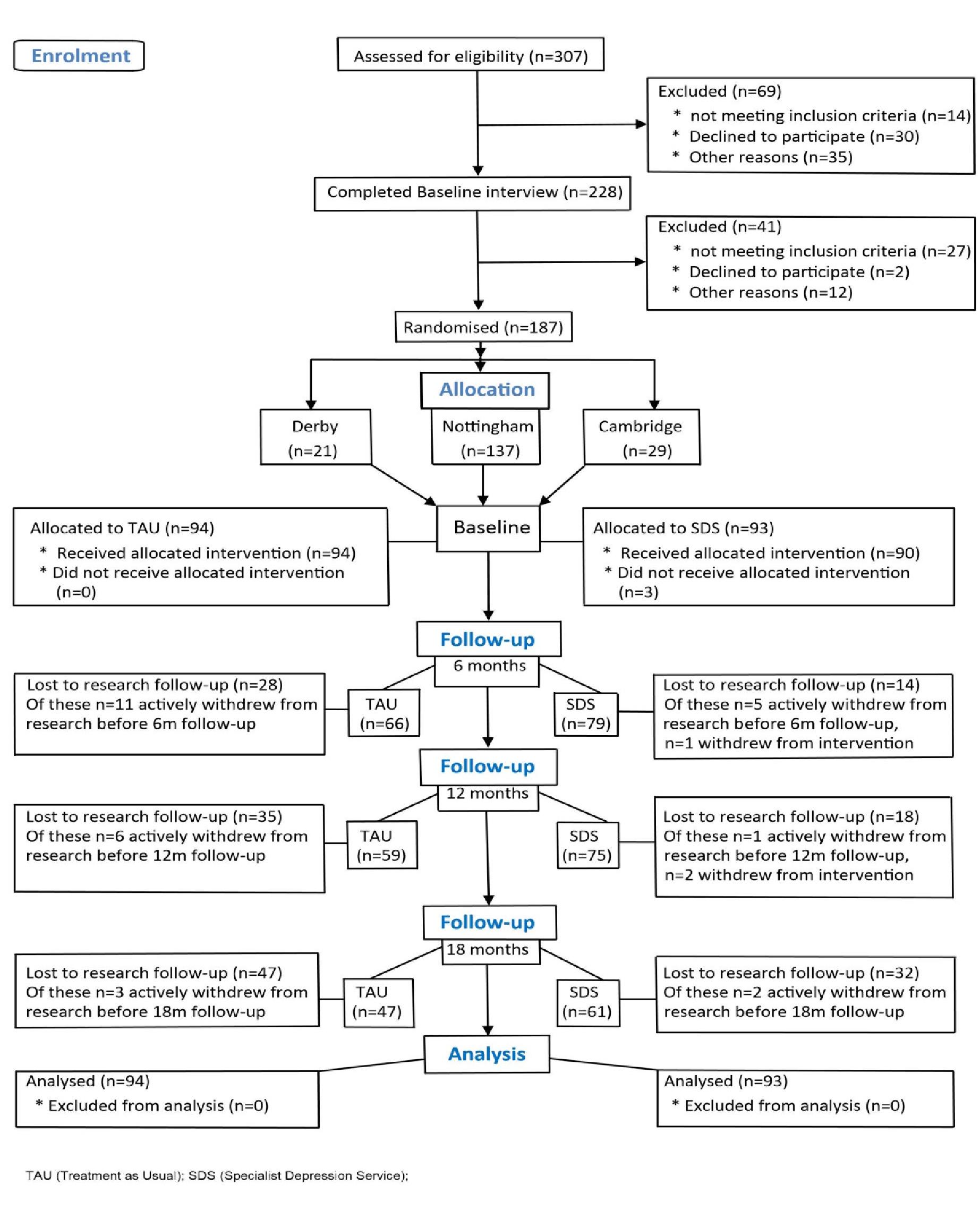
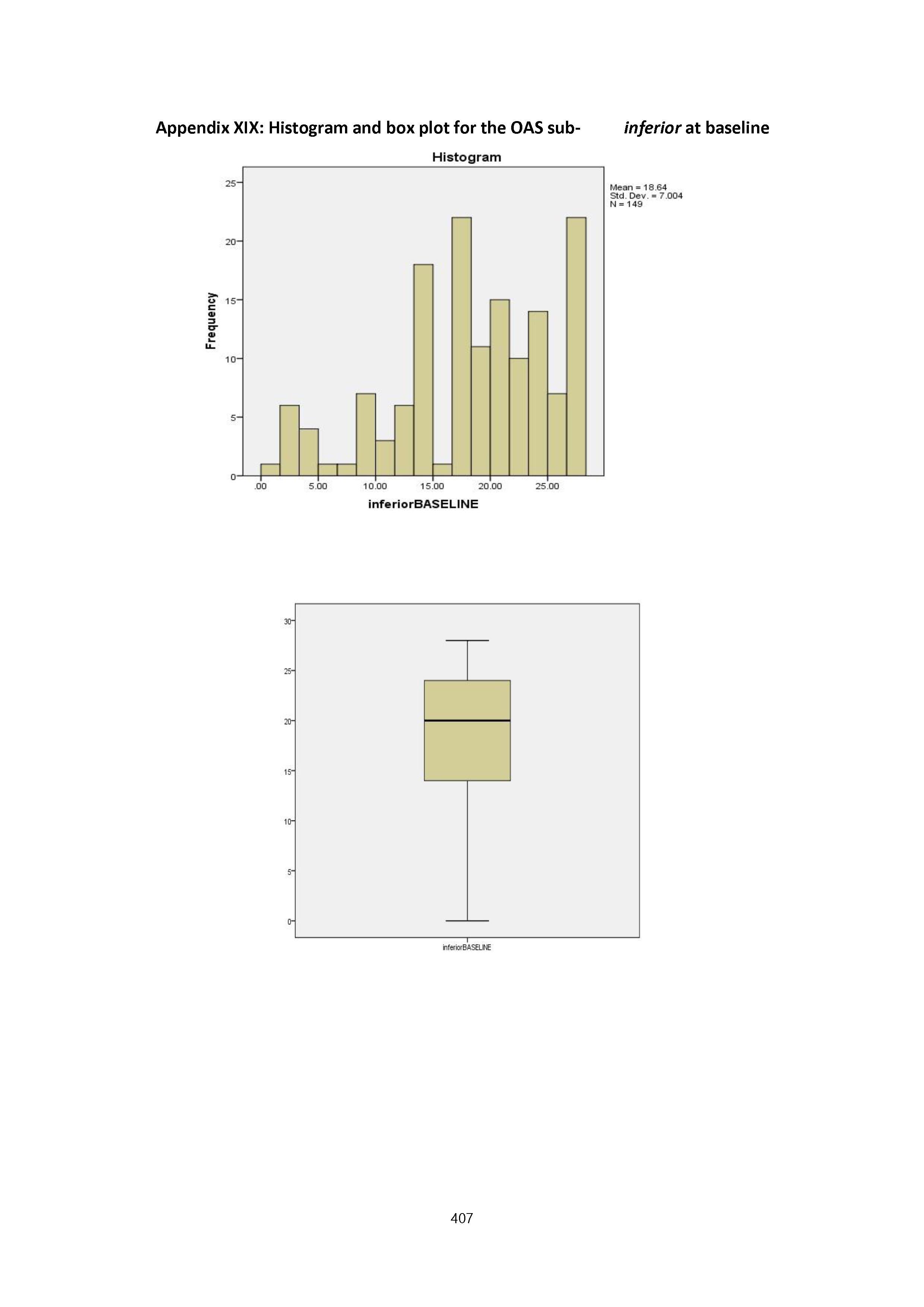
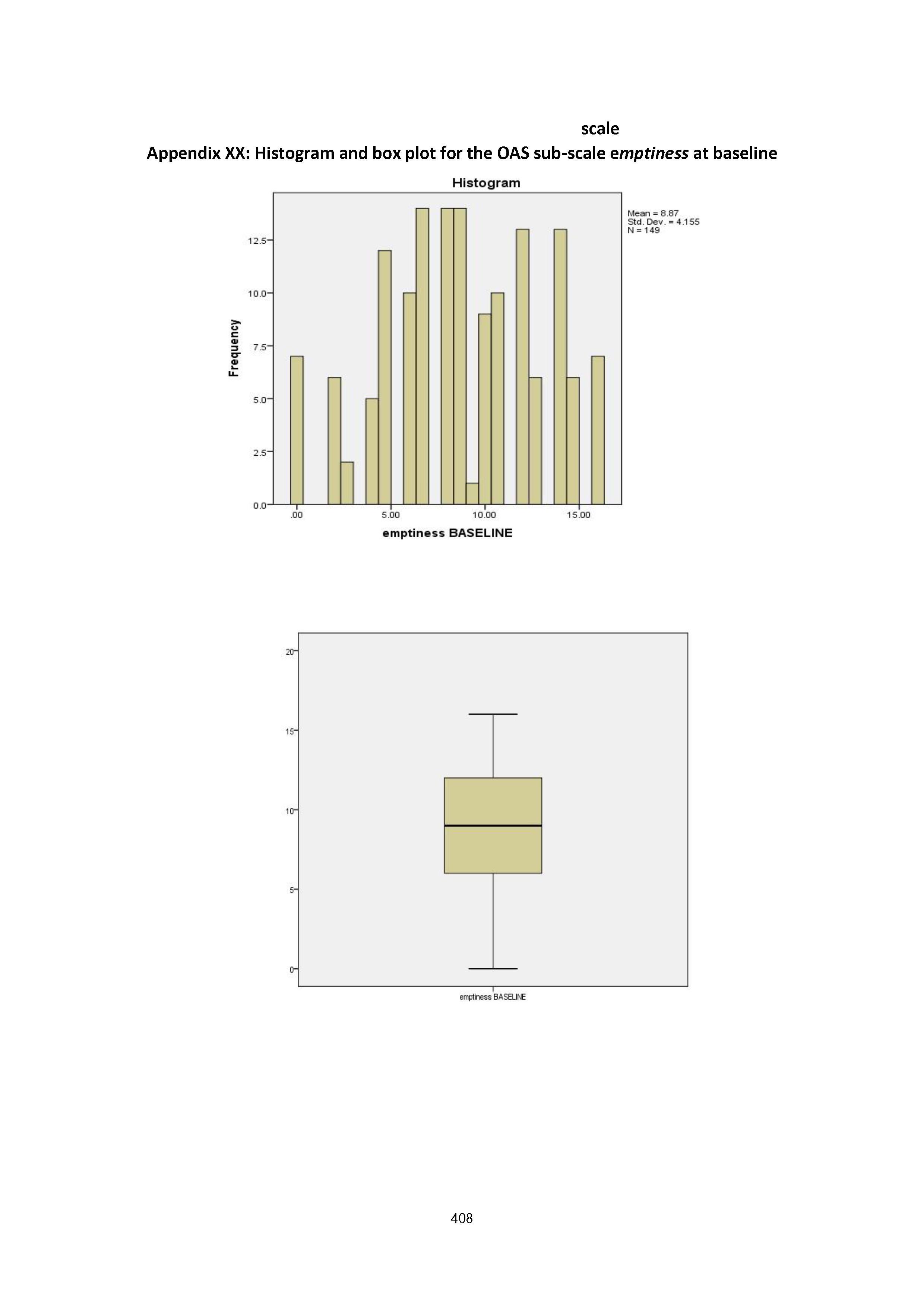
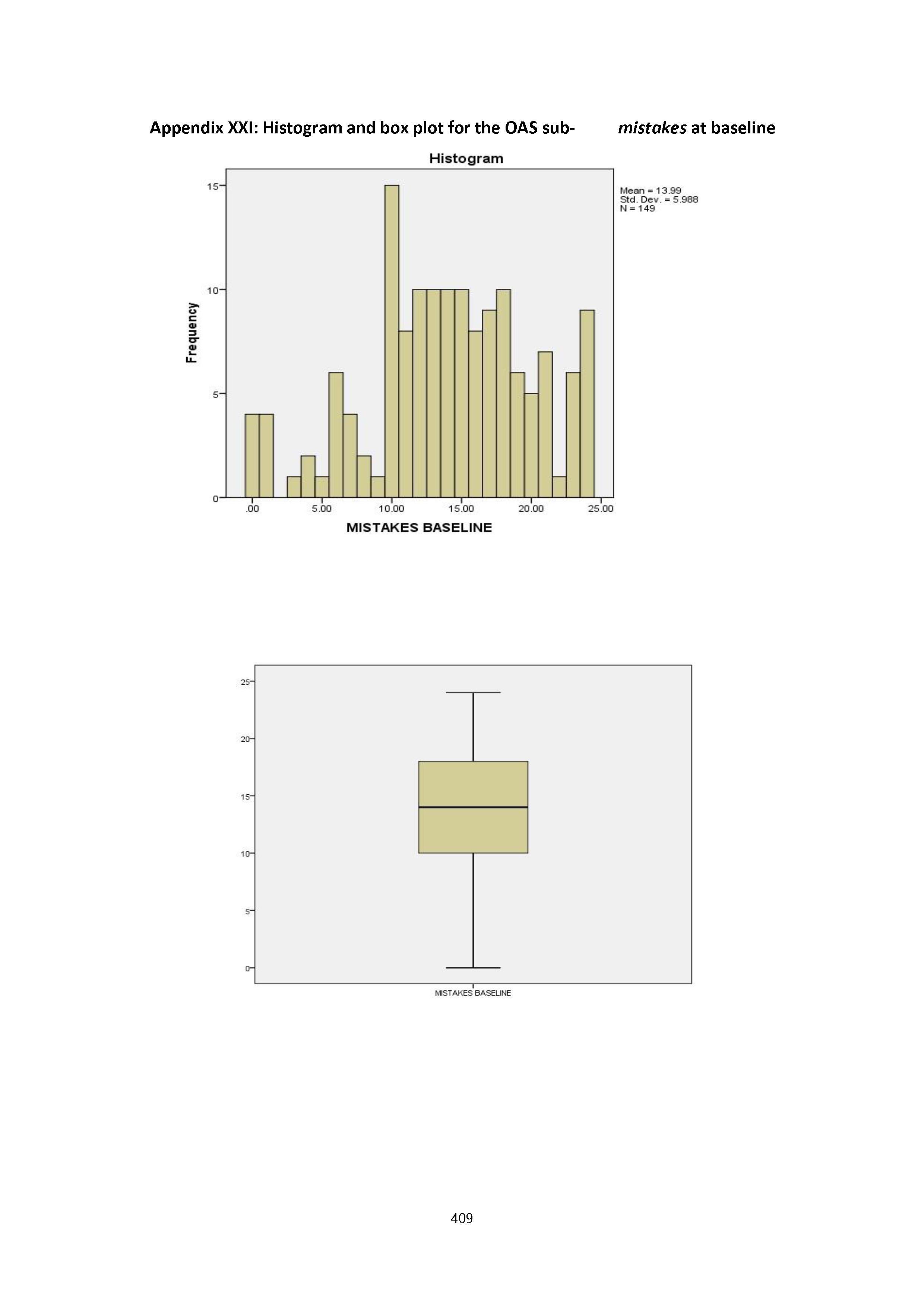
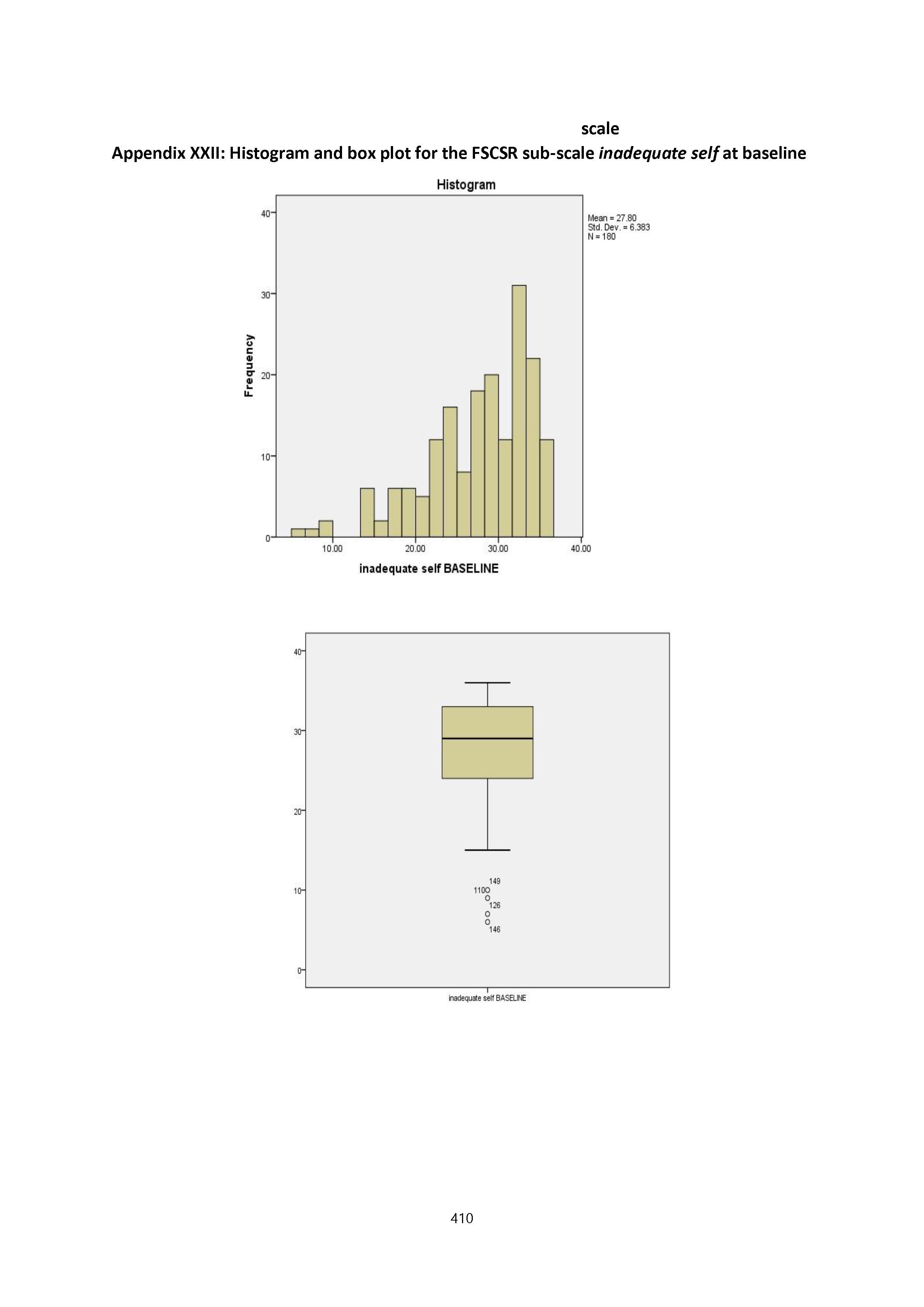

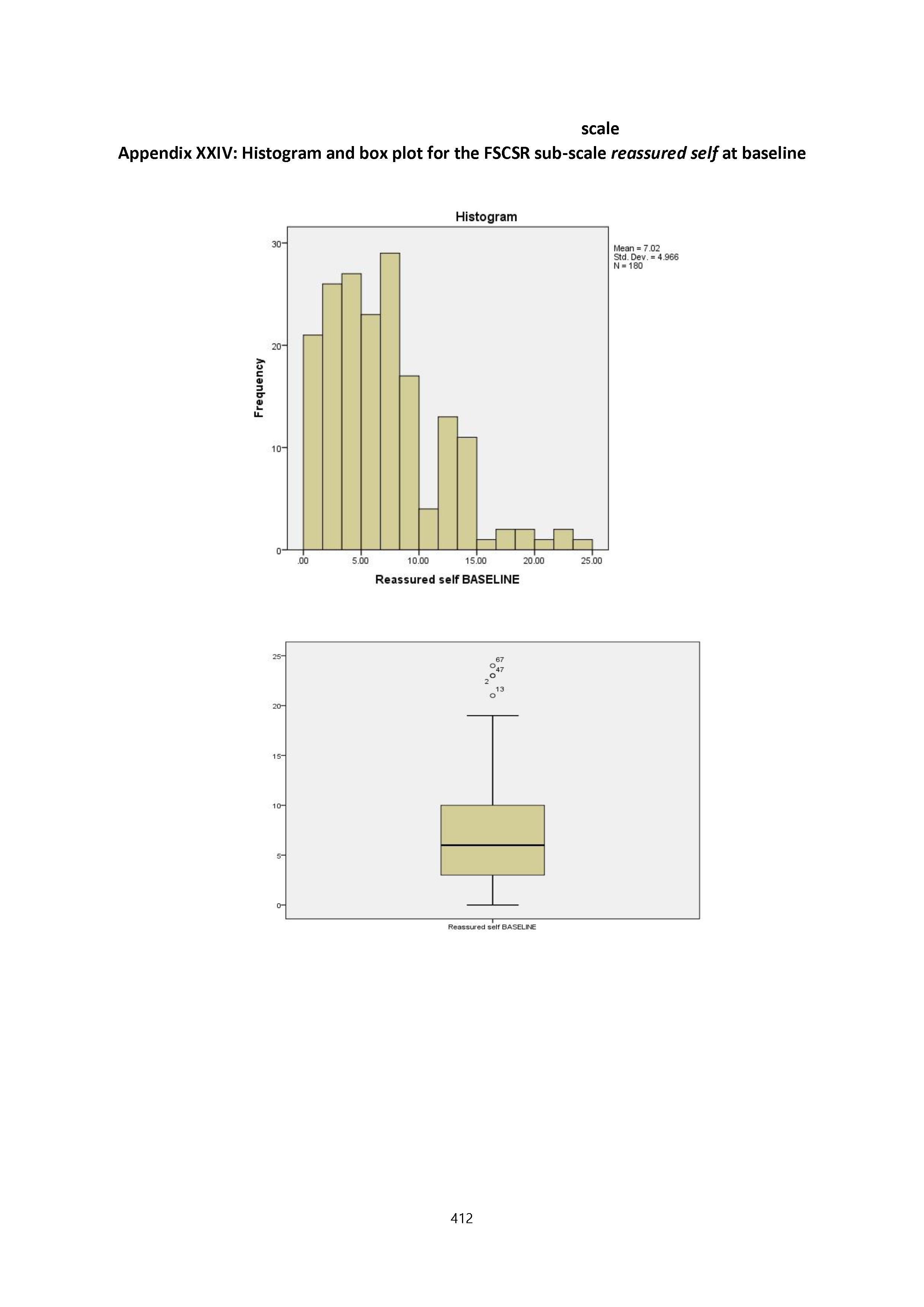
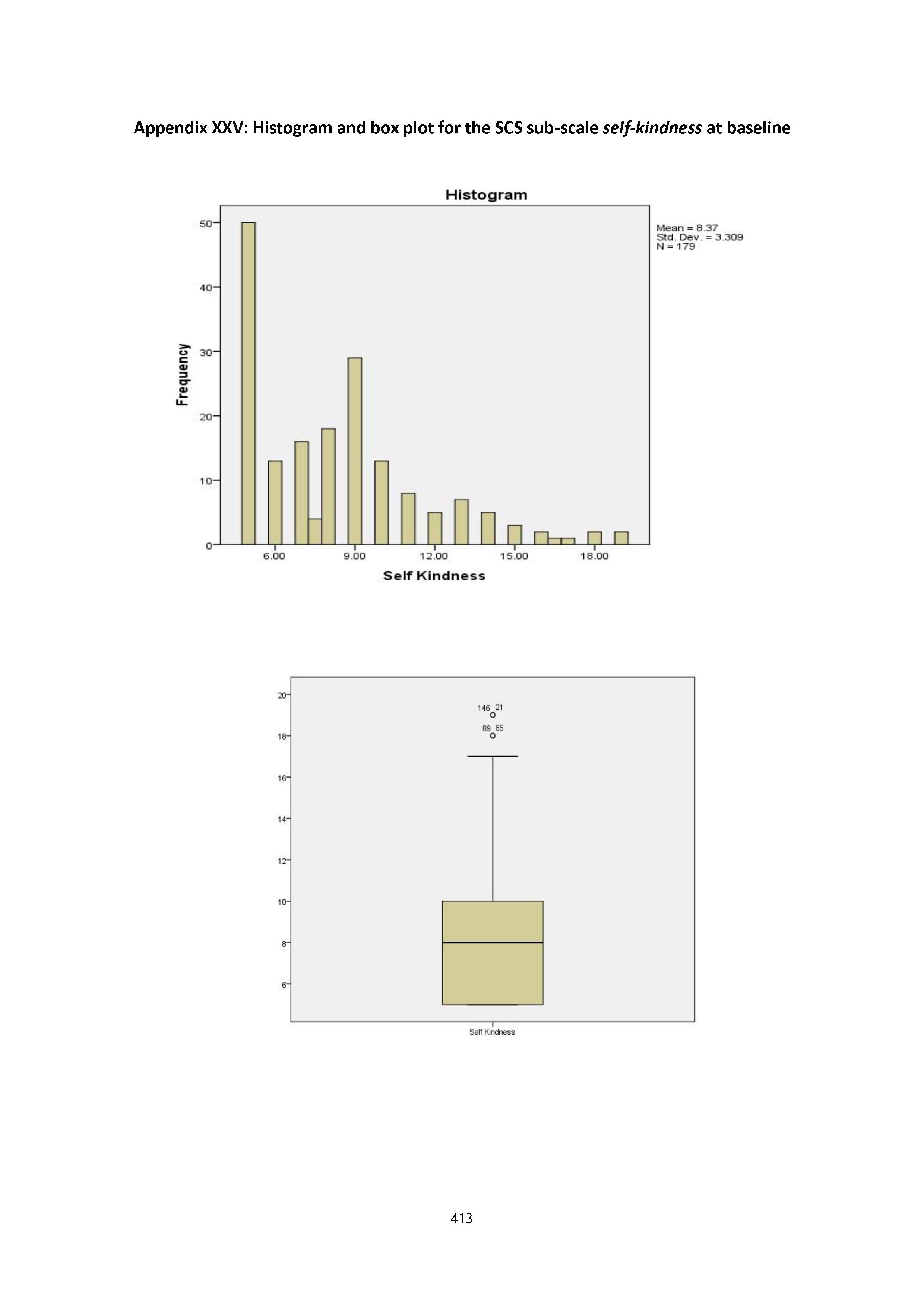
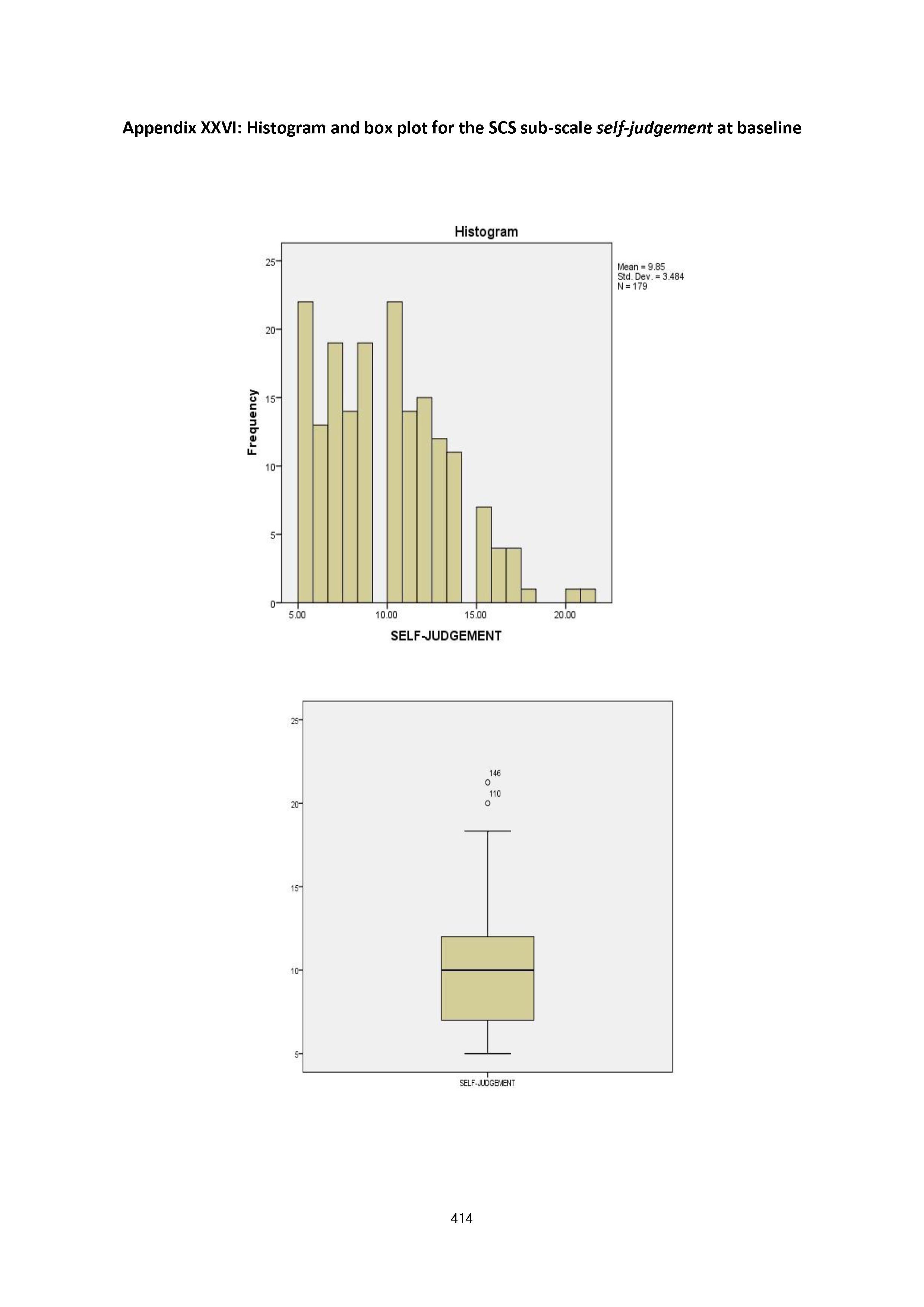

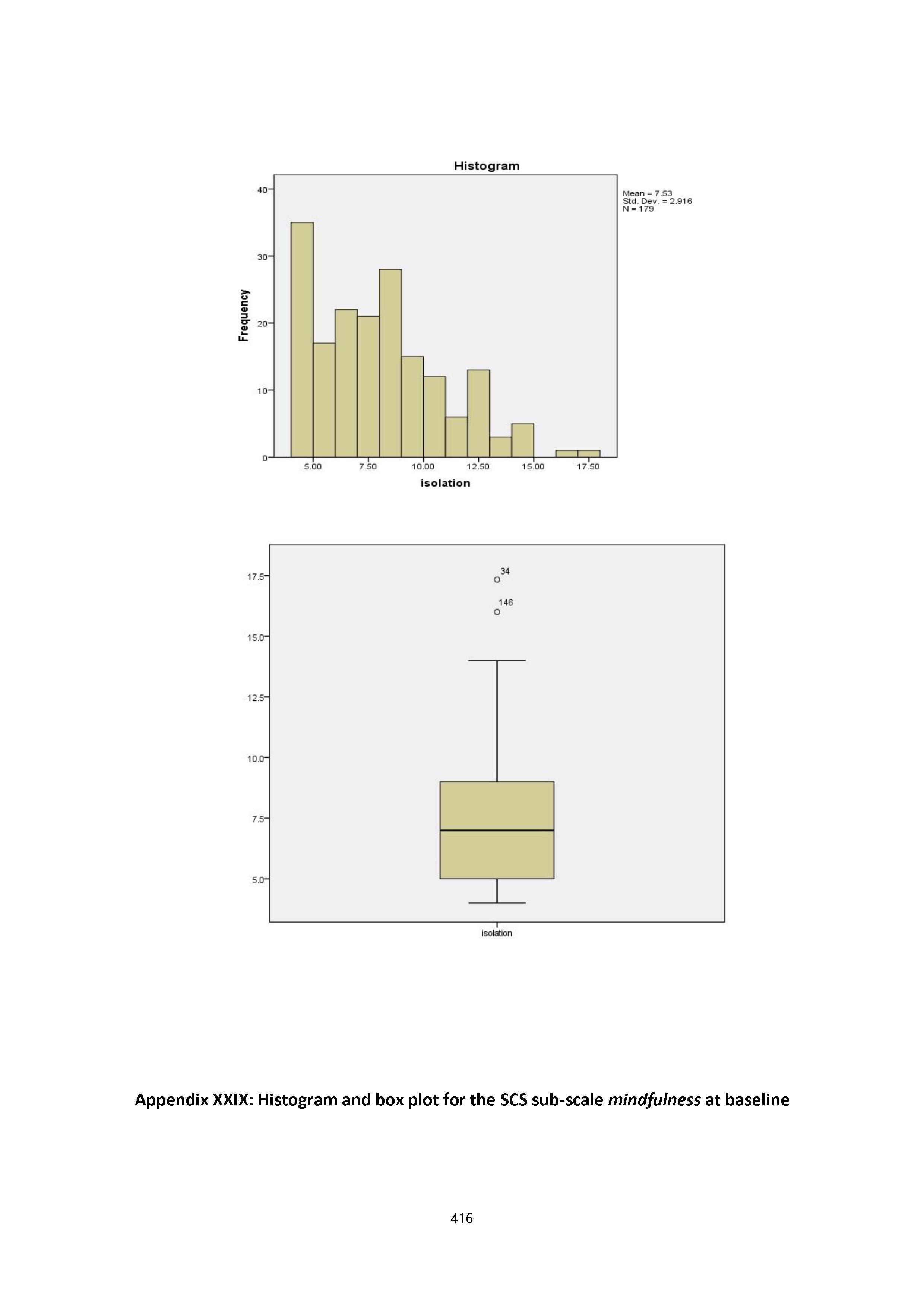
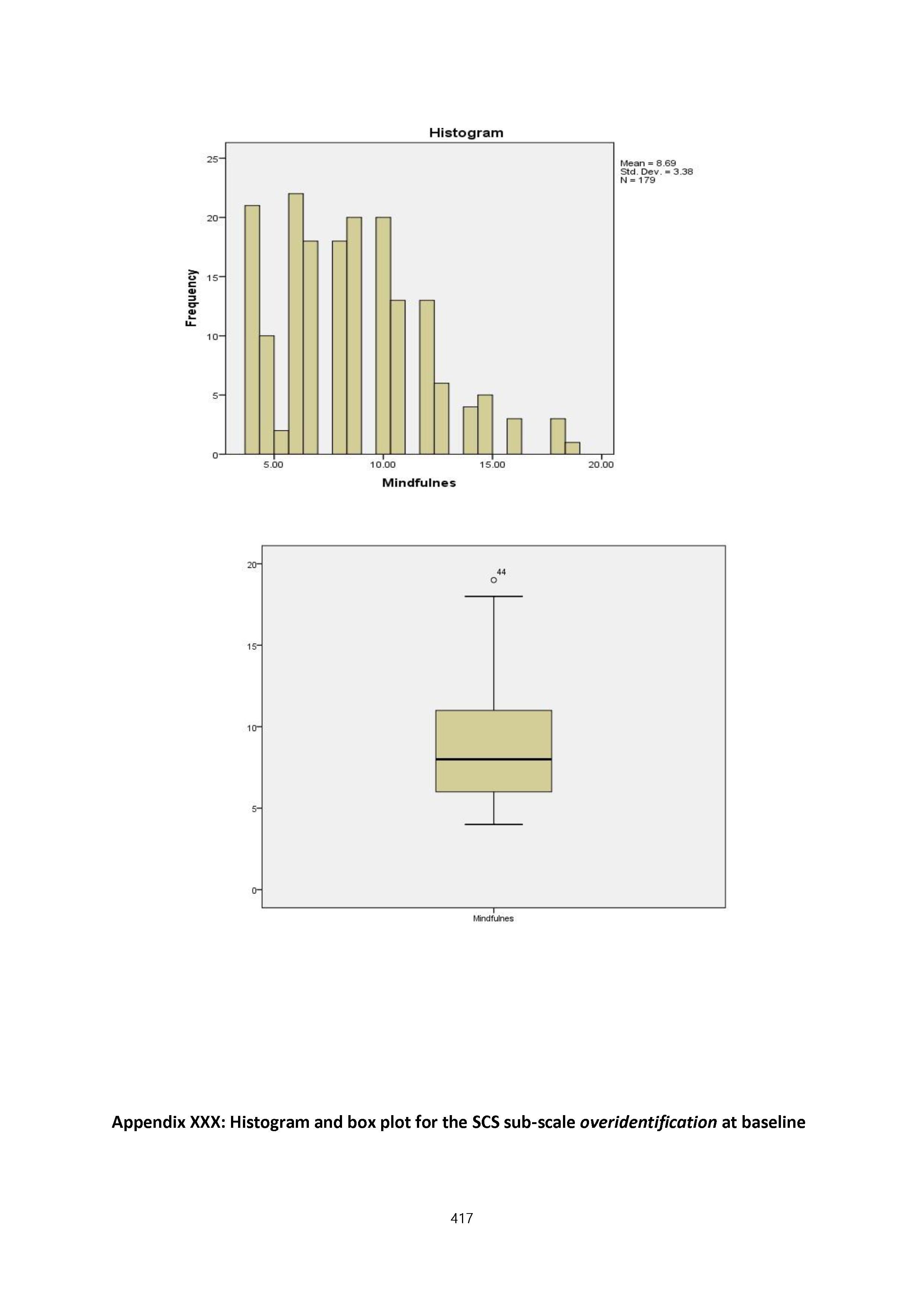
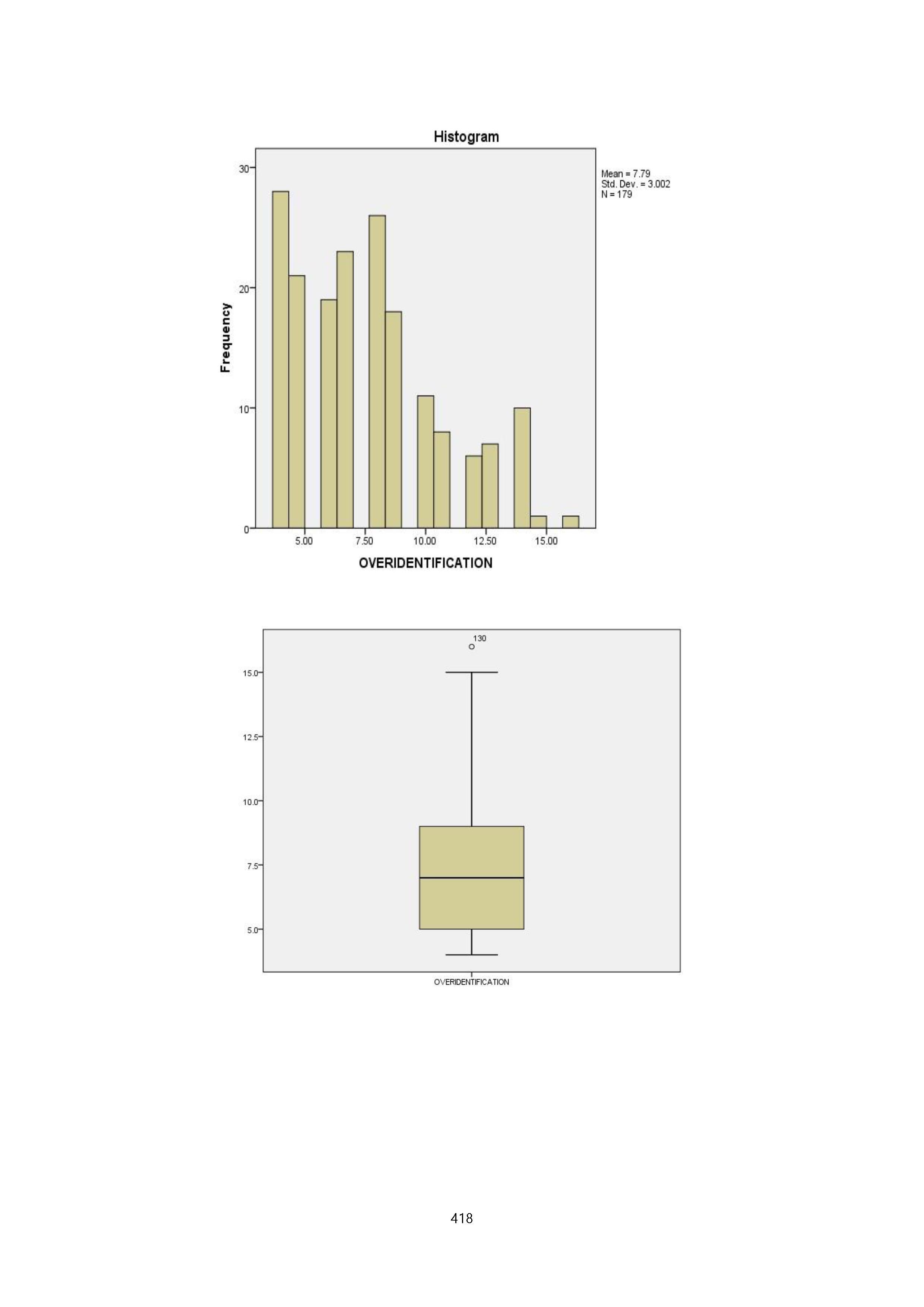

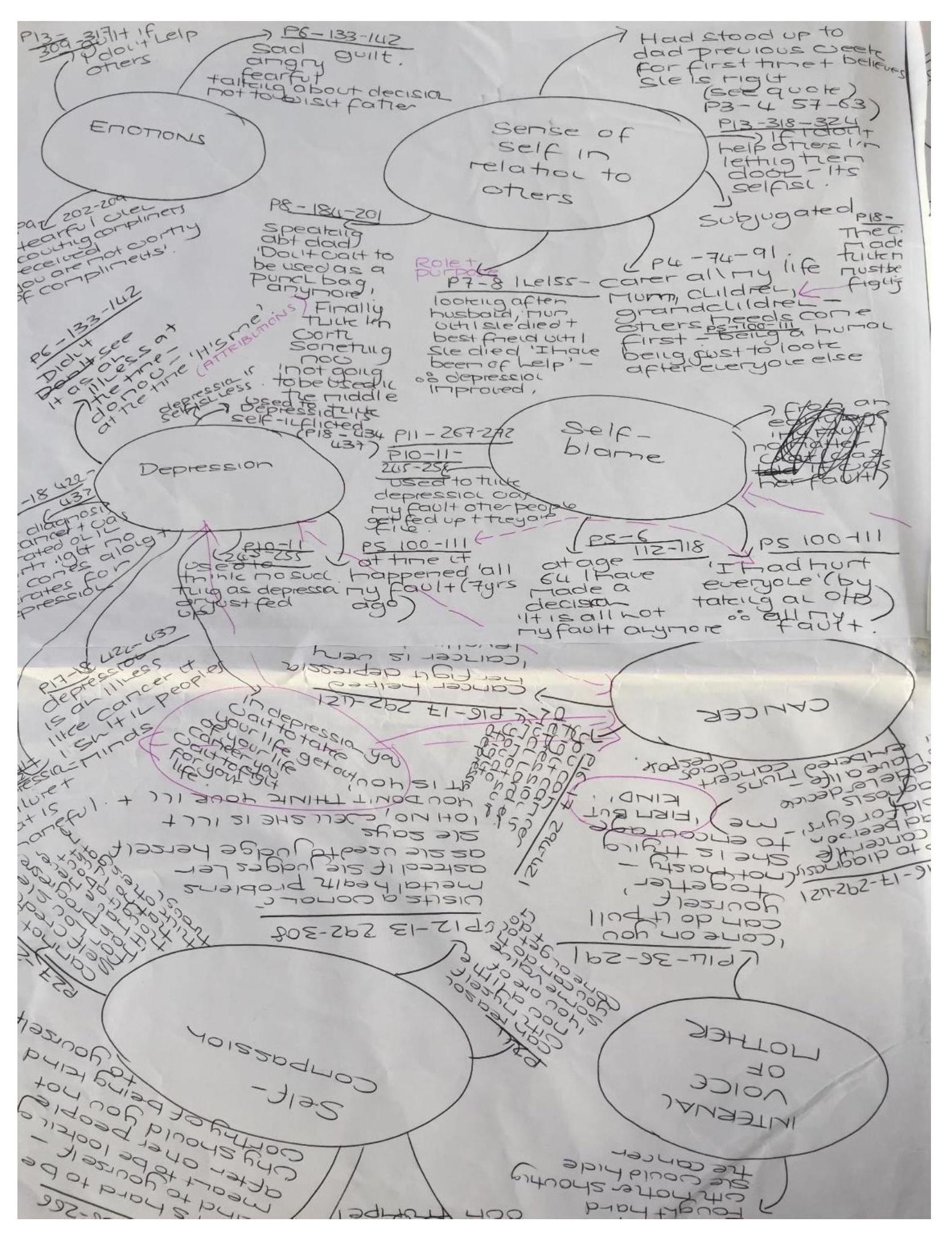
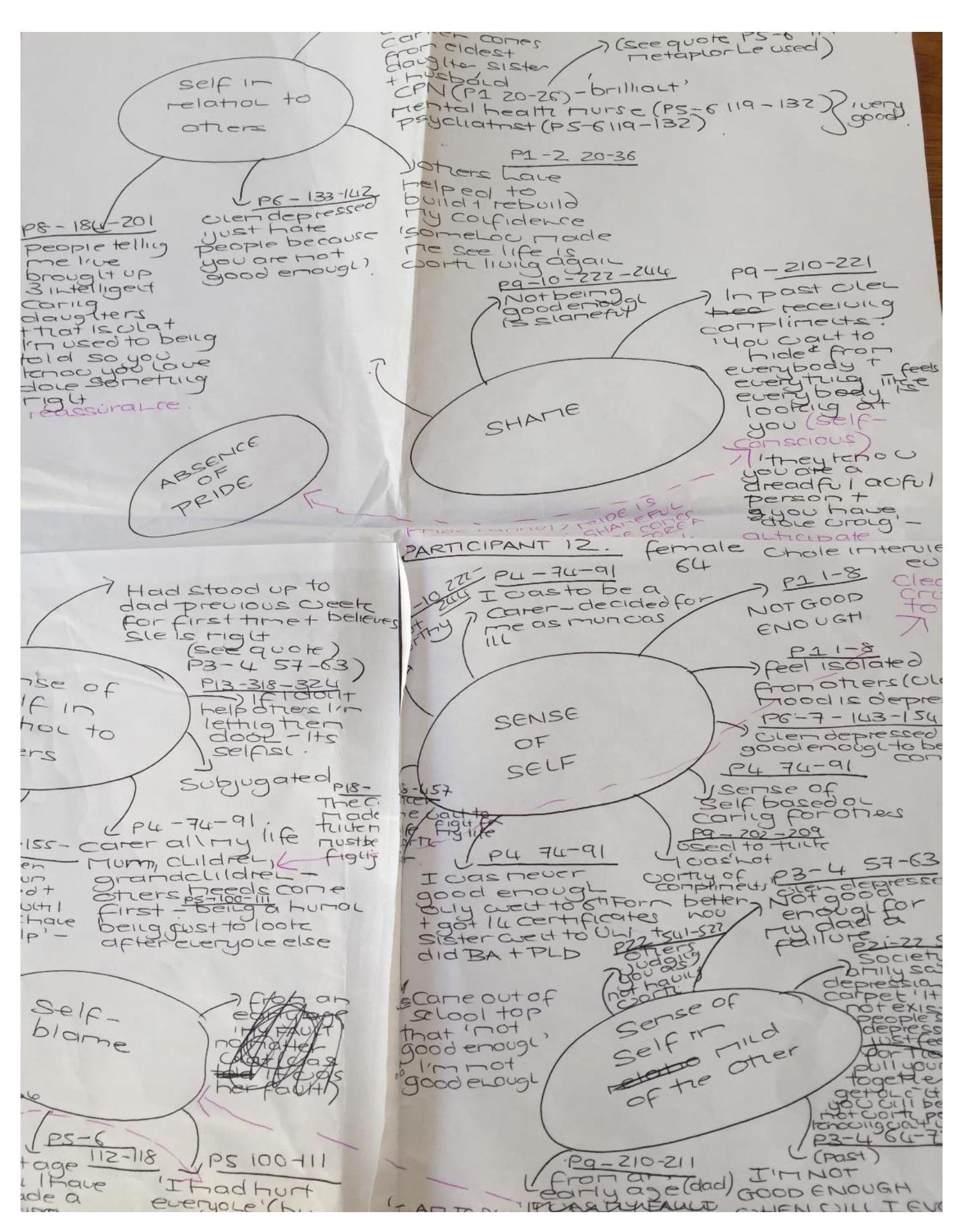
[1] Other employment includes part-time, sheltered and voluntary employment and higher education